
Article Type: Abstracts
Paul O’Connor 1, 2, Carla Sa-Couto 3, Sharon Marie Weldon 4, 6, Robyn Jane Stiger 7, 8, Colette Laws-Chapman 9
[1]
[2]
[3]
[4]
[5]
[6]
[7]
[8]
[9]
The Association for Simulated Practice in Healthcare (ASPiH) annual conference is held in Bournemouth, England from the 11th to the 13th November 2025. The three-day conference includes more than 170 poster presentations, 75 oral presentations, and 42 workshops. As can be seen from the published abstracts, a wide range of topics are addressed concerned with simulation education, technical innovation, and the use of simulation for transformation. Presenters and attendees come from a wide range of healthcare professions and specialties from across the UK, Ireland, and internationally, with participation from more than 15 countries spanning all 5 continents. This global participation underscores the theme of the conference: Simulation for Impact. More specifically, the impact of simulation on culture, co-production, and creativity.
Culture has been described as a slippery and ubiquitous concept [1]. This statement reflects the fact that there is no one agreed definition of culture, and the meaning has shifted over time. An anthropological definition of culture is “the socially transmitted knowledge and behaviour shared by some group of people” (p.23) [2]. The behavioural component of culture means that it is something that can be influenced through healthcare simulation. There are many examples of the use of simulation to impact the organisational culture. It has been suggested that in-situ simulation is particularly suited to providing valuable insight into both how ‘work is done’ and the related cultural aspects of the work in a healthcare unit [3]. There are also examples of the use of simulation to address specific aspects of organisational culture: such as safety culture or patient safety culture. For example, a Danish study found an improvement in healthcare providers’ perceptions of patient safety culture of healthcare providers following an in-situ simulation intervention [4].
An approach to using simulation to impact culture relates to improving the cultural competency of healthcare providers. Cultural competency is concerned with addressing barriers to the accessibility and effectiveness of health care services for people from racial or ethnic minorities [5]. In more recent years this concept has also been expanded to include language, sexual orientation, gender identity, class and professional status [6,7]. A systematic review of 27 papers concerned with providing simulated participant cultural competency education to student healthcare providers found that the intervention improved the cultural competence and confidence of learners [8]. More recently there has been a move away from cultural competence to cultural humility [9]. This is due to a recognition that culture perceived from a competency perspective implies that there is an endpoint to understanding culture when in reality it is fluid and requires an open and self-aware position [9,10]. Using simulation to improve cultural humility has great potential to promote equitable treatment of different cultural groups, and support culture differences across the healthcare system [9].
Co-production is an approach used to meaningfully integrate the knowledge, expertise, and experience of healthcare users into the design and delivery of healthcare services and research [11]. A distinct feature of co-production is that it does not distinguish between healthcare providers and recipients. This is achieved by reducing the social distance, knowledge, and power imbalances between different participant groups in the co-production activity [12]. It has been suggested that although co-production has great promise, it may be limited due to the risk of entanglement in existing involvement frameworks and practices [13]. Simulation offers an approach to address this limitation by providing a forum to support co-production. To illustrate, a systematic review of co-production in nursing and midwifery education identified 23 studies. It was concluded that there was preliminary evidence that participatory approaches can improve learning and positively impact on nursing and midwifery students, service users, and carers [14]. Additionally, simulation has been used to co-produce new models of care, generate more integrated care, and bridge gaps in understanding [15,16,17]. However, co-production within simulation remains limited with no clear definition of co-production within the context of healthcare simulation [18].
Creativity is integral to simulation. The range of simulation applications covered in the abstracts, posters, and workshops at ASPiH 2025 is a clear demonstration of the creativity of the community. Simulation has been described as ‘theatre with purpose’ [19]. This theatre analogy is very apt and recognises the creativity and imagination required to design and deliver simulation activities. However, this is only one aspect of simulation creativity. Increasingly simulation is also being used to impact health and care through collective understanding, insight, and learning garnered from transformative simulation approaches [20]. A visit to the ASPiH conference exhibition hall demonstrates the creativity of the simulation industry and the resulting sophistication and realism of the latest simulator technologies. It is therefore important to recognise that simulation is as complex as healthcare and more, and therefore designing it requires collective creativity to ensure it is intentional and impactful.
Although the use of simulation in healthcare might seem a relatively recent phenomenon, simulators have, in fact, been used to support the education of healthcare professionals for thousands of years. It has been suggested that the 20th century was a ‘dark age’ for healthcare simulation as compared to the previous two centuries [21]. Yet, the range of presentations, workshops, and industry stands at the APSiH 2025 conference suggest that we are now in a new and exciting age of healthcare simulation. One where the convergence of different cultures, co-production, and creativity is possible if we align with purpose.
Thank you to everyone who responded to the call for abstracts for this year’s ASPiH conference and to the scientific committee members involved in the reviewing process.
Authors’ contributions. POC conceived and wrote the first draft of the article. All other authors reviewed and contributed to subsequent drafts of the article and approved the final version.
Funding. None declared.
Availability of data and materials. Not applicable
Ethics approval and consent to participate. Not applicable
Competing interests. None declared.
1. Birukou A, Blanzieri E, Giorgini P, Giunchiglia F. A formal definition of culture. In: Sycara K, Gelfand M, Abbe A (Eds). Models for Intercultural Collaboration and Negotiation. Advances in Group Decision and Negotiation, Vol 6. London: Springer. 2013. pp. 1–26.
2. Peoples JG, Garrick AB. Humanity: An Introduction to Cultural Anthropology. Belmont, CA: West/Wadsworth. 1994.
3. Patterson MD, Eisenberg EM, Murphy A. Using Simulation to Understand and Shape Organizational Culture. In: Deutsch ES, Perry SJ, Gurnaney HG (Eds.). Comprehensive Healthcare Simulation: Improving Healthcare Systems. London: Springer. 2021. pp. 169–17.
4. Schram A, Paltved C, Christensen KB, Kjaergaard-Andersen G, Jensen HI, Kristensen S. Patient safety culture improves during an in situ simulation intervention: a repeated cross-sectional intervention study at two hospital sites. BMJ Open Quality. 2021;10(1):e001183.
5. Truong M, Paradies Y, Priest N. Interventions to improve cultural competency in healthcare: a systematic review of reviews. BMC health services research. 2014;14(1):99.
6. Yu H, Flores DD, Bonett S, Bauermeister JA. LGBTQ+ cultural competency training for health professionals: a systematic review. BMC medical education. 2023;23(1):55.
7. World Health Organisation. Cultural contexts of health and well-being principal author and editor culture matters: using a cultural context of health approach to enhance policymaking. 2020. Available from: https://www.euro.who.int/__data/assets/pdf_file/0009/334269/14780_World-Health-Organisation_Context-of-Health_TEXT-AW-WEB.pdf.
8. Walkowska A, Przymuszała P, Marciniak-Stępak P, Nowosadko M, Baum E. Enhancing cross-cultural competence of medical and healthcare students with the use of simulated patients- a systematic review. International Journal of Environmental Research and Public Health. 2023;20(3):2505.
9. Gonzales-Walters F, Weldon S, Essex R. Cultivating cultural humility through healthcare simulation-based education: a scoping review protocol. International Journal of Healthcare Simulation. 2024; doi: 10.54531/rafh4191.
10. Foronda C, Baptiste DL, Reinholdt MM, Ousman K. Cultural humility: a concept analysis. Journal of Transcultural Nursing. 2016;27(3):210–217.
11. Filipe A, Renedo A, Marston C. The co-production of what? Knowledge, values, and social relations in health care. 2017; PLoS Biology. 15(5): e2001403.
12. Ramrez R. Value co-production: intellectual origins and implications for practice and research. Strategic Management Journal.1999;20:4965.
13. Bovaird T. Beyond engagement and anticipation: user and community co-production of public services. Public Administration Review. 2007;67: 846860.
14. O’Connor S, Zhang M, Trout KK, Snibsoer AK. Co-production in nursing and midwifery education: A systematic review of the literature. Nurse Education Today. 2021;102:104900
15. Weldon SM, Kneebone R, Bello F. Collaborative healthcare remodelling through sequential simulation: a patient and front-line staff perspective. BMJ Simululation and Technology Enhanced Learning. 2016. 27;2(3):78–86.
16. Weldon S-M, Ralhan S, Paice E, Kneebone R, Bello F. Sequential simulation of a patient pathway. Clinical Teacher. 2016;14(2):90–94.
17. Kneebone R, Weldon S-M, Bello F. Engaging patients and clinicians through simulation: rebalancing the dynamics of care. Advances in Simulation 2016;1:19. doi: 10.1186/s41077-016-0019-9.
18. Philpott L, Markowski M & Weldon SM. Lived experience co-production in simulation education and practice- a scoping review protocol. Journal of Healthcare Simulation. 2025. [In print].
19. Dieckmann P, Gaba D, Rall M. Deepening the theoretical foundations of patient simulation as social practice. Simulation in Healthcare. 2007; 2(3):183–93.
20. Weldon SM, Buttery AG, Spearpoint K, Kneebone R. Transformative forms of simulation in health care-the seven simulation-based ‘I’s: a concept taxonomy review of the literature. International Journal of Healthcare Simulation. 2023 Jul 7:1–13.
21. Owen H. Early Use of Simulation in Medical Education. Simulation in Healthcare. 2012;7(2):102–116.
Diana Dupont 1, Karen Furlong 1, Jaime Riley 2
[1]
[2]
A multi-patient simulation involving patients with acute health challenges was co-created by nursing faculty at the University of New Brunswick, Canada. The integration of this simulation occurred during the 2023 Fall term. Presented findings are focussed on data collected in the 2024 Fall term as research leads obtained ethical approval prior to this second offering. Although simulation-based experiences (SBEs) are well established as effective tools in building capacity in health care programs [1], the use of multi-patient simulations in support of skills such as clinical judgement and time management remain underexplored. The National Council State Boards of Nursing’s Clinical Judgement Measurement Model (CJMM)[2] helped frame learning objectives while INASCL standards were adhered to in the design of this simulation [3]. The purpose of this presentation is to share key findings and recommendations for a study exploring student perceptions of this multi-patient SBE.
A mixed-methods approach was used in this study. Quantitative data were collected using pre- (n=70) and post-(n=60) simulation quizzes, with questions aligned to learning objectives. These quizzes assessed students’ knowledge and clinical judgement before and after the simulation. Qualitative data were collected through two focus groups (n=7) which included an exploration of students’ perceptions of elements impacting their ability to meet learning objectives. Quantitative data were analysed using descriptive statistics. Content analysis was used to identify key concepts which were organized into categories.
Quiz responses between subgroups of students were compared – students were either enrolled in the BN program through a bridging model or entered through a four-year pathway. All students scored poorly on questions involving teamwork and scope of practice considerations. In contrast, students who entered the BN program through the bridging model scored significantly higher on time management.
Content analysis of focus group data revealed key categories: 1) knowing what to expect and what is expected of me; 2) realism as a performance factor; and; 3) acknowledging the impact of past experience.
Findings from this study offer insights into how senior nursing students experience and respond to a multi-patient simulation. Relationships between previous clinical experience, preparation, perceived realism, and the link to performance have implications for simulation design and teaching and learning strategies beyond a simulation context. A limitation of this study is the focus group participants included only students enrolled in the four-year pathway.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Bray L, Østergaard D. A qualitative study of the value of simulation-based training for nursing students in primary care. BMC Nursing. 2024;23(1):1–10. doi: 10.1186/s12912-024-01886-0.
2. National Council of State Boards of Nursing. (2019). Clinical judgment measurement model. Next Generation NCLEX News,13, 1–6. Available from: https://www.ncsbn.org/public-files/NGN_Winter19.pdf
3. INACSL Standards Committee, Watts PI, McDermott DS, Alinier G, Charnetski M, Ludlow J, Horsley E, Meakim C, Nawathe P. Healthcare Simulation Standards of Best Practice® Simulation Design. Clinical Simulation in Nursing, 2021;58:14–21. doi: 10.1016/j.ecns.2021.08.009.
Ingrid Bispo 1, Carla Cerqueira 2, Isilda Ribeiro 2, Cristina Carvalho 2, Fernanda Carvalho 2, Carla Sá-Couto 1
[1]
[2]
Simulation-based interprofessional (IP) education programs at the undergraduate level remain limited both worldwide [1] and within the Portuguese educational context [2]. The LINKS workshop - Lifting INterprofessional Knowledge through Simulation - is a novel initiative designed for IP teams of healthcare students (medicine and nursing). It aims to enhance team-based behavioural competencies that are essential for effective IP teamwork. This pilot study aims to assess the impact of the LINKS workshop on communication skills within IP undergraduate teams.
This quasi-experimental study involved final-year medical and nursing students participating in a 4-hour, simulation-based IP workshop. Working in mixed teams, students managed two clinical scenarios designed to promote interprofessional communication, each offering equivalent challenges and opportunities to practice key communication strategies. Each scenario was followed by a structured debriefing led by experienced facilitators, focusing on teamwork skills, including key communication strategies. A total of thirteen IP teams participated. The scenarios were video recorded for subsequent analysis of the teams’ performance.
Interprofessional communication was assessed using an observational tool for monitoring non-technical skills [3], focusing on four communication strategies: (1) iSBAR (e.g., identification, situation, background, assessment and request/recommendation); (2) cross-checks; (3) closed-loop communication; and (4) summaries/time-outs. Four independent observers reviewed the recordings and scored team performance on each communication skill, using a 3-points scale: 0 - Not observed; 1 - Observed but inconsistent or incorrect use; 2 - Observed consistently and correctly used.
The Wilcoxon signed-rank test was used to compare performance in both scenarios. Inter-rater reliability was assessed using Cronbach’s alpha. This study was approved by the ethical committee of the Faculty of Medicine of the University of Porto, and written informed consent was obtained from all participants.
Internal consistency of communication strategies scores was acceptable (Cronbach 0.7 ≤ α < 0.8), for both scenarios. Statistically significant improvements were observed in all four communication strategies and in the overall communication score between the two scenarios (p<0.05, Figure 1).
Teams demonstrated improved use of communication strategies in the second scenario, suggesting a positive effect of the IP simulation activity combined with a structured debriefing. This pilot study reinforces the value of simulation-based IP educational at the undergraduate level in clarifying professional roles and enhancing team communication. Continued implementation of such programs within clinical training can foster essential teamwork competencies and drive meaningful curriculum reform, preparing students for effective collaborative practice in healthcare settings.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Choudhury RI, Salam Mau, Mathur J, et al. How interprofessional education could benefit the future of healthcare – medical students’ perspective. BMC Med Educ. 2020;20:242.
2. Sa-Couto C, Fernandes F, Pinto CC, Loureiro E, Cerqueira C. Impact of a simulation-based interprofessional workshop (LINKS) on Portuguese healthcare students’ perception of roles and competencies: a quasi-experimental pilot study. Int J Healthc Simul. 2024;XX(XX). doi: 10.54531/PRHF1746
3. Rosário L, Sá-Couto CD, Loureiro E. An observational and action-based tool for non-technical skills monitoring in Simulation-Based Training. SESAM 2019 Proceedings.

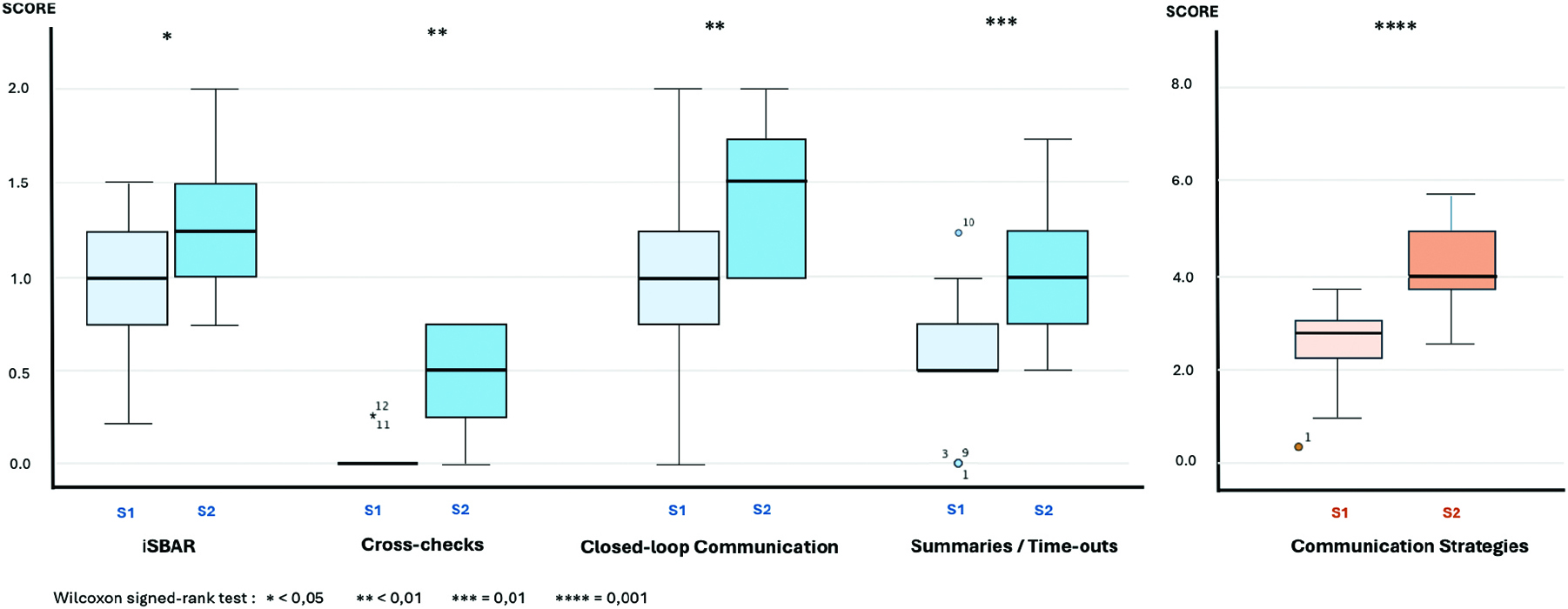
Box plots illustrating team scores (n=13) for each communication strategy in Scenario 1 (S1) and Scenario 2 (S2). Scores represent the mean ratings from the four independent observers, assessing the application and consistency of the communication strategies.
Oliver Hart 1, Alex Hall 2, Johann Willers 2
[1]
[2]
Emergency department thoracotomy (EDT) in children is a rare, high-stakes procedure performed primarily during traumatic cardiac arrest [1]. Training opportunities are limited, and current reliance on porcine models raises ethical concerns and lacks paediatric anatomical fidelity. This project aimed to develop and evaluate a low-cost, Aqueous Dietary fibre Antifreeze Mix gel (ADAMgel) based, synthetic model tailored to paediatric EDT, improving training accessibility, anatomical realism, and trainee confidence [2].
A novel thoracotomy model replicating the thoracic cavity of a 9-year-old child was constructed using synthetic materials, including ADAMgel-laminated soft tissues and a skeletal framework, Figure 1. The model underwent iterative development informed by expert focus groups. Final evaluation included two simulation sessions with doctors (n=11), who completed pre- and post-simulation Likert scale questionnaires assessing confidence and understanding. Data were collected between January and March 2025. Results were analysed using Wilcoxon signed-rank tests. Qualitative feedback was gathered from participants and faculty at the Royal College of Surgeons (RCS) Pre-hospital emergency resuscitative thoracotomy course.
All procedures were conducted with appropriate institutional approval for educational simulation-based research.
Statistically significant improvements were observed across several domains: confidence in performing EDT increased from median 1 to 4 (p=0.027), understanding of the procedure (p=0.016) and anatomy (p=0.019) also improved. All participants unanimously agreed the model improved their confidence and was a useful training aid. Surface tissues were rated realistic by 91%, and bony structures by 82%. Feedback from RCS faculty highlighted the model’s advantages over porcine equivalents, including reusability, independent practice opportunities, and superior anatomical accuracy. Suggested improvements included stronger tissue fixation and simulated aortic control.
This ADAMgel-based model demonstrates a feasible, ethical, and effective alternative to animal models in paediatric EDT simulation. Improvements in learner confidence and anatomical understanding support its utility in early procedural training. Planned enhancements, including aortic occlusion simulation, will increase fidelity. Broader validation across experience levels will determine its future role in standardised trauma education.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Moskowitz EE, Burlew CC, Kulungowski AM, Bensard DD. Survival after emergency department thoracotomy in paediatric trauma. Pediatr Surg Int. 2018;34(8):857–860.
2. Clifford E, Stourton F, Willers J, Colucci G. Development of a Low-Cost, High-Fidelity, Reusable Model to Simulate Clamshell Thoracotomy. Surg Innov. 2023;30(6):739–744.


Anoopkishore Chidambaram 1
[1]
Simulation-based education (SBE) has become a cornerstone of healthcare training, providing hands-on learning experiences that develop technical proficiency while also promoting critical thinking and clinical judgement [1-3]. These cognitive skills are essential for delivering safe and effective patient care. This scoping review explores recent innovations in SBE and examines their impact on the development of critical thinking and decision-making among undergraduate and postgraduate healthcare learners.
A structured scoping review was conducted using peer-reviewed articles published between 2020 and 2025. A systematic search strategy, developed with support from an academic librarian, identified relevant studies across CINAHL, MEDLINE, and Embase databases. Inclusion criteria focused on studies reporting outcomes related to critical thinking or clinical decision-making within a simulation context. Both qualitative and quantitative studies were included. A thematic synthesis approach was applied to identify key patterns across different simulation modalities (e.g., high-fidelity simulation, virtual reality, blended learning) and learner groups.
Thirty-three articles met the inclusion criteria. The findings consistently demonstrate that SBE enhances learners’ critical thinking and clinical reasoning abilities. Effective educational strategies included the use of high-fidelity simulation environments, structured debriefing, psychological safety, and reflective learning models. Technological innovations, particularly screen-based simulation and virtual reality (VR), were noted to improve learner engagement and cognitive development. Interprofessional simulations were highlighted as valuable in supporting real-time decision-making under pressure. However, evidence regarding the long-term retention and clinical transferability of these skills was limited.
Simulation-based education appears highly effective in promoting critical thinking and clinical decision-making skills within healthcare education. Successful outcomes depend on deliberate instructional design, appropriate use of fidelity, effective feedback processes, and learner-centred approaches. While technological advances offer promising new avenues for skill development, further longitudinal research is needed to determine the durability of these cognitive gains and their impact on clinical practice. These insights may inform the future design and optimisation of simulation-based curricula.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Alharbi A, Nurfianti A, Mullen RF, et al. Enhancing critical thinking through simulation: a systematic review. BMC Med Educ. 2024;24(1):1099–1111.
2. Stenseth HV, Steindal SA, Solberg MT, et al. Virtual reality in healthcare simulation: a systematic review. J Med Internet Res. 2025;27:e58744.
3. Marchi AJ, Paganotti L. Simulation fidelity and clinical judgement: a narrative review. Simul Healthc. 2025;20(1):N.PAG.
Emma-May Curran 1, Victoria Meighan
[1]
Haemorrhagic shock is the one of the leading causes of death in trauma patients and early recognition of blood loss, haemorrhage control and rapid massive transfusion is lifesaving [1]. Efficient delivery of blood products is essential to the care of trauma patients [2] and is dependent on excellent multi-disciplinary teamwork and communication.
In our institution, a Dublin based designated Trauma Unit, we sought to investigate the effect of multi-disciplinary simulation based medical education on time to delivery of blood products in a massive transfusion.
Four multi-disciplinary team (MDT) simulation based medical education training sessions were held between 2020 and 2022. The MDT included prehospital National Ambulance Service, emergency department medical and nursing staff, porters, health care assistants, surgical and intensive care doctors and blood bank staff.
Each simulation was based on a major trauma and used a standardised massive transfusion protocol.
To evaluate the efficacy of the MDT simulation-based training, a retrospective review was carried out which analysed the; i) Activation of the massive transfusion protocol, ii) time to issue pack one, and, iii) time for pack one to be collected from the lab.
Prior to the MDT simulation-based education the average time from activation of the MTP to the blood arriving in the emergency department was in excess of 40 minutes. After conducting the training, the time decreased to 32 minutes. The average time from activation of the MTP to issuing pack one was 13 minutes and from issuing the blood to delivery to the emergency department was 20 minutes which was a significant improvement on the pre-training times.
We demonstrated a reduction in time to delivery of blood products associated with regular MDT in situ simulation training. Deliberate practice of the massive transfusion protocol improved teamwork and communication which lead to a reduction in time taken for the delivery of blood products.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Eastridge BJ, Holcomb JB, Shackelford S. Outcomes of traumatic hemorrhagic shock and the epidemiology of preventable death from injury. Transfusion. 2019;59:1423–1428. doi: 10.1111/trf.15161.
2. Nunez TC, Young PP, Holcomb JB, Cotton BA. Creation, implementation, and maturation of a massive transfusion protocol for the exsanguinating trauma patient. J Trauma. 2010 Jun;68(6):1498–505. doi: 10.1097/TA.0b013e3181d3cc25. PMID: 20539192; PMCID: PMC3136378.
Helen Jarvis 1, Tiffany McCurdy 1, Rufaro Ndokera 1, Emma Sang 1
[1]
There is limited research providing guidance on deliverance of in-situ simulation (ISS) in ambulances, within the transport setting. Previous studies have shown that only 67% of UK neonatal transport teams provide ISS and this takes place less than weekly in 60% of teams surveyed [1]. Simulation-based education (SBE) is well established in enhancing team-work, communication and awareness of human factors, all of which are significantly more challenging in transport, due to clinical isolation, scarcity of resources and physical and sound barriers.
KIDSNTS is a joint paediatric and neonatal transport service, covering the West-Midlands region. Many staff members are dually trained in paediatric and neonatal retrieval allowing speciality collaboration. St Johns Ambulance technicians additionally contribute to the multi-disciplinary team (MDT) care. Many team members have limited or no experience of SBE previously. Joint ISS delivery literature is scarce.
This project will evaluate the newly introduced KIDSNTS ISS programme. MDT ISS’ run at least twice-monthly and cover neonatal and paediatric scenarios. A continued review of staff pre- and post-ISS questionnaires will examine SBE expectations and prior experience. Psychological measures of wellbeing, stress and self-efficacy will be tested with staff attending ISS, to determine their feasibility for measuring long-term service impact. Prospectively, objective data will be collected from stabilisation times and adverse event submissions to evaluate ISS impact. Data will be used to provide future direction for the KIDSNTS programme.
In less than a year since introduction, the KIDSNTS simulation team, comprising of a neonatal and a paediatric consultant, and a dually-trained education lead nurse, has so far delivered close to 20 ISS, reaching approximately 50 staff members. Pre-ISS feedback has revealed ongoing staff anxiety and reluctance to engage in SBE. Early post-ISS feedback however, indicate that staff have all experienced positive learning outcomes and are eager to continue to take part. Introduction of a pre-briefing information video, general raised awareness of SBE, as well as pre-planned, clinically monthly-themed scenarios are all being undertaken, aiming to lessen anxiety and increase uptake. ISS has already led to service provision changes and increased enthusiasm for SBE, with some team members undertaking additional training to be become simulation facilitators.
Evaluating KIDSNTS staff perceived barriers to transport ISS will support the embedding and success of the SBE programme. Further research will focus on the positive outcomes that ISS will have on safe patient transport care, as well as staff confidence and well-being.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. MacLaren AT, Peters C. In situ simulation in neonatal transport. Infant. 2016;12(5):168–170.
Sasha Bryan 1, Amy Purse 1, Chelsea Curry 1, Heidi Singleton 1, Bernice Law 1, Jakob Rossner 1, Emily Brooks 1, Alex Hull 1, Debbie Holley 1
[1]
Individuals with ASC experience poorer health outcomes globally, yet healthcare professionals often lack adequate ASC knowledge [1]. Simulation-based learning enhances recall and practice [2], though resource limitations often restrict its use. Mental health nursing simulations are less developed compared to other fields, leaving a gap in training. Our co-created 360-degree video aims to address this by providing realistic scenarios that enhance students’ empathy and confidence in working with ASC patients.
This research aimed to co-create real-time scenarios filmed in 360-degree video to help students understand how a person with ASC experiences hospital admission or clinical procedures. Working with qualified nurses and individuals with lived experience, we developed a 360-degree video of an ASC patient being assessed in a hospital setting. The video was embedded in a Complex Health Care teaching unit and viewed by third-year nursing students using Oculus Quest™ devices. Data were collected via an online survey and focus group discussions (with students and staff) and thematically analysed [3]. Ethical clearance was obtained from our university’s ethics committee.
Eighty students responded to our survey (32% response rate), with 65% reporting no prior ASC training. Seventy-four per cent found the VR resource useful, and 66% felt it would benefit their clinical practice. The small sample size is a limitation, and responses may not be fully representative of the broader student population. Ongoing focus group analysis suggests that the VR exercise helps increase students’ confidence, knowledge, and empathy, as evidenced by comments like: “This was excellent as it put you in the shoes of someone with ASC.” Staff facilitators provided insights into running VR sessions with large cohorts, including the need for preparatory and debriefing sessions, managing background noise, appropriate staff-to-student ratios, and addressing students entering the session late.
This study highlights a significant educational gap, with many students lacking prior ASC training. The positive response to the VR experience suggests it can improve understanding, empathy, and confidence, which may translate to better clinical interactions with ASC patients. Facilitators also identified key considerations for optimizing VR sessions, such as session preparation, managing group dynamics, and debriefing for knowledge consolidation and reflective practice. These findings have implications for nursing education policies, emphasizing the need for structured VR training in mental health curricula. Future research should explore the long-term impact of VR training on knowledge retention and clinical practice, as well as best practices for large-group VR training.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable
1. Corden K, Brewer R, Cage E. A Systematic Review of Healthcare Professionals’ Knowledge, Self-Efficacy and Attitudes Towards Working with Autistic People. Rev J Autism Dev Disord. 2022 Sep 1;9(3):386–99.
2. Singleton H, James J, Falconer L, Holley D, Priego-Hernandez J, Beavis J, et al. Effect of non-immersive virtual reality simulation on Type 2 diabetes education for nursing students: a randomised controlled trial. Clin Simul Nurs. 2022;66:50–7.
3. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Internal QR funding received for this research.
Kirsty Duncan 1, Olivia Cole 1, Rose Edwards 1
[1]
38% of LGBTQIA+ individuals report negative experiences within healthcare in the United Kingdom [1], yet no mandatory LGBTQIA+ training exists for NHS staff post-qualification. Simulation-based training can provide a platform to promote culturally competent LGBTQIA+ care [2]. University Hospitals Dorset developed a livestream simulation to increase healthcare staff access to LGBTQIA+ education, with the aim of improving staff confidence in communicating with LGBTQIA+ people.
The simulation was co-produced with LGBTQIA+ community members as knowledge experts with lived experience, including a Transgender woman contacted through the hospital’s Pride Network. The simulation was live streamed via Microsoft Teams from the simulation suite with 40 multiprofessional healthcare staff and students attending online, through voluntary self-selection. Two students participated in the simulation using a high-fidelity manikin voiced by a transgender woman. The scenario focused on pre-operative care, including pregnancy testing, sex assigned at birth, pronouns, and bed allocation in the context of single-sex bays. A facilitated debrief involved in-person participants, online participants through a monitored Teams chat and LGBTQIA+ contributors including a Transgender woman. Online pre- and immediate post-simulation questionnaires captured participant self-assessment and feedback for mixed-method evaluation focusing on accessibility and impact on staff.
Accessibility - 87.5% reported this as first time attending LGBTQIA+ training. Rated as easy to engage with, useful and recommendable. Participants included nurses, physicians, administrators, educators, students, OPDs and child health. 27 of 40 online participants actively communicated via Microsoft Teams chat.
Confidence - Increased confidence communicating with LGBTQIA+ individuals’ post-session. Valued knowledge experts openly sharing feelings and lived experiences.
Qualitative feedback indicated increased awareness of emotional impact of assumptions and importance of open, person-centred communication.
Reported online participant disclosed transgender status to peers post-session.
This project addressed a training gap through accessible simulation that attracted multiprofessional attendees, demonstrating relevance across diverse roles, and increased staff confidence in communicating with LGBTQIA+ individuals. Participants valued the inclusion of diverse faculty and LGBTQIA+ experiences, highlighting the importance of co-production and collaborative facilitation from knowledge experts with lived experience. Feedback from 25% of participants provided valuable insights, and future efforts will focus on increasing response rates for online sessions. Faculty expressed concern about potential incivility in the online format, however none arose likely due to the voluntary session attracting people sensitive to the topic. Research into the process and impact of engaging healthcare staff who would not typically volunteer for such sessions would be valuable.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Government Equalities Office. National LGBT Survey: Research report. Government Equalities Office; 2018. Available from: https://www.gov.uk/government/publications/national-lgbt-survey-research-report Accessed 15 April 2025.
2. Pittiglio L, Lidtke J. The use of simulation to enhance LGBTQ+ care competencies of nursing students. Clin Simul in Nurs. 2021;56:133–136. doi: 10.1016/j.ecns.2021.04.010.
This project would not have been possible without the technical expertise of Thomas Randell-Turner, Andrew Lawrence and Sam Pask.
Shiv Vohra 1, Nicholas Stafford, Hermione Tolliday, Matthew Williams
[1]
All anaesthetic and Acute Care Common Stem (ACCS) trainees are expected to undergo an Initial Assessment of Competence (IAC) during the first 3 to 6 months of their anaesthetic training. The umbrella term ‘novice anaesthetist’ is used to describe an anaesthetist in training yet to achieve their IAC.
As per the Royal College of Anaesthetists, one of the two core learning outcomes of the IAC is to provide general anaesthesia for American Society of Anesthesiologists (ASA) I/II patients having uncomplicated surgery [1,2].
A new regional two-day simulation course was developed to enhance novice anaesthetists’ preparedness and confidence during their IAC period. The broader aims of the course were to improve equity of access to and ensure sustainability of simulation training for novice anaesthetists across the region.
The course was delivered to two cohorts of novice anaesthetists in September 2024 (August 2024 intake) and February/March 2025 (February 2025 intake). Participants engaged in structured simulation scenarios across two days, targeting key anaesthetic competencies including both technical and non-technical skills. Preparedness to join the anaesthetic on-call rota and confidence in managing ASA I/II cases were assessed via pre- and post-course surveys, using a 5-point Likert scale (1 = not at all prepared/confident; 5 = very well prepared/confident). Post-course evaluation of educational value, scenario quality, facilitation, and facilities was conducted, alongside collection of qualitative feedback.
Analysis demonstrated a consistent increase in self-reported preparedness and confidence following course completion as shown in Figure 1.
The majority of participants rated educational value, clinical relevance, and facilitation quality as excellent (scores of 4 or 5).
Qualitative responses highlighted the benefits of scenario variety and the supportive learning environment provided by the faculty.
Participation in a structured regional simulation course significantly improves novice anaesthetists’ preparedness and confidence during the IAC period.
Future work should examine longitudinal outcomes, including impact on clinical performance and progression, and consider evolving the course to incorporate contemporary anaesthetic techniques such as total intravenous anaesthesia (TIVA) [1,2].
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Royal College of Anaesthetists. Entrustable Professional Activities (EPAs) for Anaesthetic Training: EPA 1 & 2 v1.2. 2022. Available from: https://www.rcoa.ac.uk/sites/default/files/documents/2022-09/EPA-1-2-2022%20v1.2.pdf
2. Royal College of Anaesthetists. Guidance for Simulation-Based Education in Anaesthesia Training v1.0. 2024. Available from: https://www.rcoa.ac.uk/sites/default/files/documents/2024-11/Guidance%20for%20Simulation-based%20education%20in%20anaesthesia%20training_v1.0_Nov_2024.pdf
The Simulation Centre team, Quad Centre, Queen Alexandra Hospital, Portsmouth
All faculty members from Hampshire Hospitals NHS Foundation Trust and Portsmouth University Hospitals NHS Trust

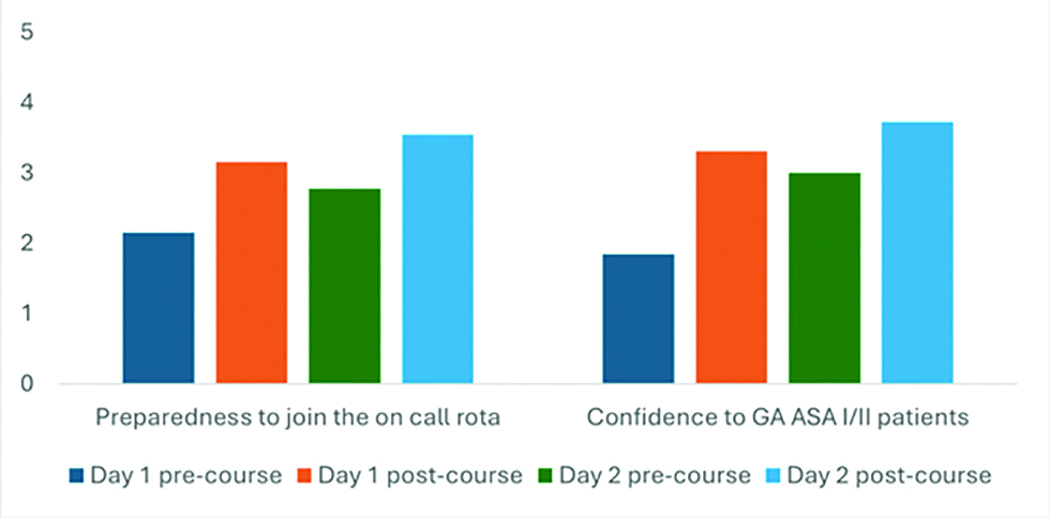
Bar Chart Showing Pre- and Post-course Scores for the Novice Anaesthetic Simulation Course
Iman Denideni 1
[1]
Foundation Year 1 (FY1) doctors are unlikely to have firsthand experience of navigating the unique chaos of a Medical Emergency Team (MET) call before joining the team. Experiential learning through simulation could help to bridge this gap between theory and practice [1].
The aim of this simulation project was to provide a realistic view of a MET call from the FY1 perspective. The simulation scenarios progressed in real-time, to uncover hidden internal pressures caused by delayed access to crucial information. They also replicated some logistical challenges commonly encountered by MET members, such as locating necessary equipment in an unfamiliar environment.
Three groups of eight final-year medical students participated in a simulated on-call shift in which they were alerted to a medical emergency (septic shock) using a high-fidelity simulation suite. Psychological safety was maintained by the inclusion of a ‘medical registrar’ acting as team leader. Participants were delegated common tasks undertaken by an FY1, such as establishing intravenous access, obtaining a blood gas, scribing, etc.
Participants had been pre-briefed that all tasks must be completed accurately in real-time. The scenario ran for thirty minutes, followed by a structured debrief addressing human factors [2]. The students repeated the experience a month later with a different clinical scenario (hypoglycaemic seizure). Anonymous reflective questionnaires were collected after each scenario.
Free-text answers from the first (n=23) and second (n=19) questionnaires were analysed for recurring themes [3]. Participants appreciated that their first exposure to the unique pressures of working in a MET was in a safe, simulated environment.
Working in real-time made the scenario feel more realistic but introduced uncertainty and time-pressure that had to be managed. 96% of respondents underestimated the time required to complete their tasks in a stressful environment, which caused further anxiety.
The first scenario gave participants a frame of reference from which they felt better prepared to approach the second. They also reported a greater appreciation for non-technical skills such as closed-loop communication, time-management, prioritisation and teamwork, and applied these more consciously in the second scenario [2].
Hands-on experience made final-year medical students feel better prepared for attending MET calls as future FY1s. The real-time element highlighted latent human factors, necessitating the application of non-technical skills. This simulation design has potential for use during FY1 induction programmes to safely introduce the challenges of working in a MET.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Watmough S, Box H, Bennett N, Stewart A, Farrell M. Unexpected medical undergraduate simulation training (UMUST): can unexpected medical simulation scenarios help prepare medical students for the transition to foundation year doctor? BMC Medical Education. 2016 Apr 14;16(1).
2. Pruden C, Beecham GB, Waseem M. Human Factors in Medical Simulation [Internet]. PubMed. Treasure Island (FL): StatPearls Publishing; 2021. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559226/
3. Naeem M, Ozuem W, Howell KE, Ranfagni S. A step-by-step process of thematic analysis to develop a conceptual model in qualitative research. International Journal of Qualitative Methods [Internet]. 2023 Nov 8;22(1):1–18. Available from: https://journals.sagepub.com/doi/10.1177/16094069231205789
Ingrid Bispo 1, Emil Havránek 2, Kristýna Hrachovinová 2, Dominika Králová 2, Marc Lazarovici 3, Carla Sá-Couto 1
[1] Community Medicine, Information and Decision Sciences Department (MEDCIDS), Faculty of Medicine,
[2]
[3]
Current midwifery curricula often lack adequate training in optimal positioning techniques for pregnant women, a critical factor for ensuring safe labour outcomes. Evidence from other disciplines [1,2] strongly suggests that enhanced visualization techniques significantly improve proficiency, accelerate learning, and deepen understanding. The PROGRESSION project, funded by the Erasmus+ program, aims to develop a VR-based learning concept to visualize and train positioning maneuvers while illustrating the subtle movements of internal anatomical structures. This study aimed to assess the educational impact of PROGRESSION on midwifery students’ knowledge. Additionally, the usability of the system was also evaluated.
This pre-post-test study was conducted with second-year midwifery students in the Czech Republic as part of their regular 3-year curriculum. Students’ knowledge of maternal positioning during labour was initially assessed using an online questionnaire consisting of 10 clinical case-based questions. Approximately two weeks later, students participated in a 4-hour VR-based training session, held in groups of four. Prior to the session, students were given time to familiarize themselves with the VR technology.
The practical VR training included two hours of self-training on basic labour positioning techniques, followed by two hours of facilitated training during which each student engaged in a clinical scenario and received structured feedback. At the end of the training, knowledge was reassessed using the same questionnaire, with the order of questions and answers shuffled to minimize recall bias. Additionally, students evaluated the usability of the VR system using the System Usability Scale (SUS) [3].
The study was approved by the Ethical Committee of the Faculty of Medicine of Masaryk University, and informed consent was obtained from all participants.
Nineteen midwifery students participated in the study. Students’ knowledge significantly improved following the VR-based educational experience compared to baseline (p=0.008), with a median increase in scores of approximately 10% (Figure 1). Regarding usability, twelve students (63%) rated the VR system above average according to the SUS scoring system (Score≥68).
Midwifery students demonstrated improved knowledge following the VR-based educational experience. By enabling the visualization of pelvic anatomical structures and interactive positioning of the pregnant woman, this approach appears to be a promising tool for enhancing students’ skills in maternal positioning during labour and ultimately promoting safer maternal care. Furthermore, the positive usability ratings suggest that the system is well accepted by students, supporting its further development and future integration into midwifery education.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Kyaw BM, Saxena N, Posadzki P, et al. Virtual reality for health professions education: systematic review and meta-analysis by the Digital Health Education Collaboration. J Med Internet Res. 2019;21(1). doi: 10.2196/12959.
2. Smelt J, Corredor C, Edsell M, Fletcher N, Jahangiri M, Sharma V. Simulation-based learning of transesophageal echocardiography in cardiothoracic surgical trainees: A prospective, randomized study. J Thorac Cardiovasc Surg. 2015 Jul;150(1):22–5. doi: 10.1016/j.jtcvs.2015.04.032. Epub 2015 Apr 23.
3. Brooke J. Usability Evaluation in Industry. CRC Press; London, UK: 1996. SUS-A quick and dirty usability scale; pp. 4–7.
The authors would like to acknowledge the team of professionals from the Faculty of Medicine of Masaryk University who also contributed to this study: Barbora Ježková, Matěj Anton, Marika Bajerová, Lukáš Hruban, as well as the students who volunteered their time and effort.
This study is co-funded by the European Union (Erasmus+ KA220 HED Cooperation Partnerships for higher education 2023-1-DE01-KA220_HED-000158531).

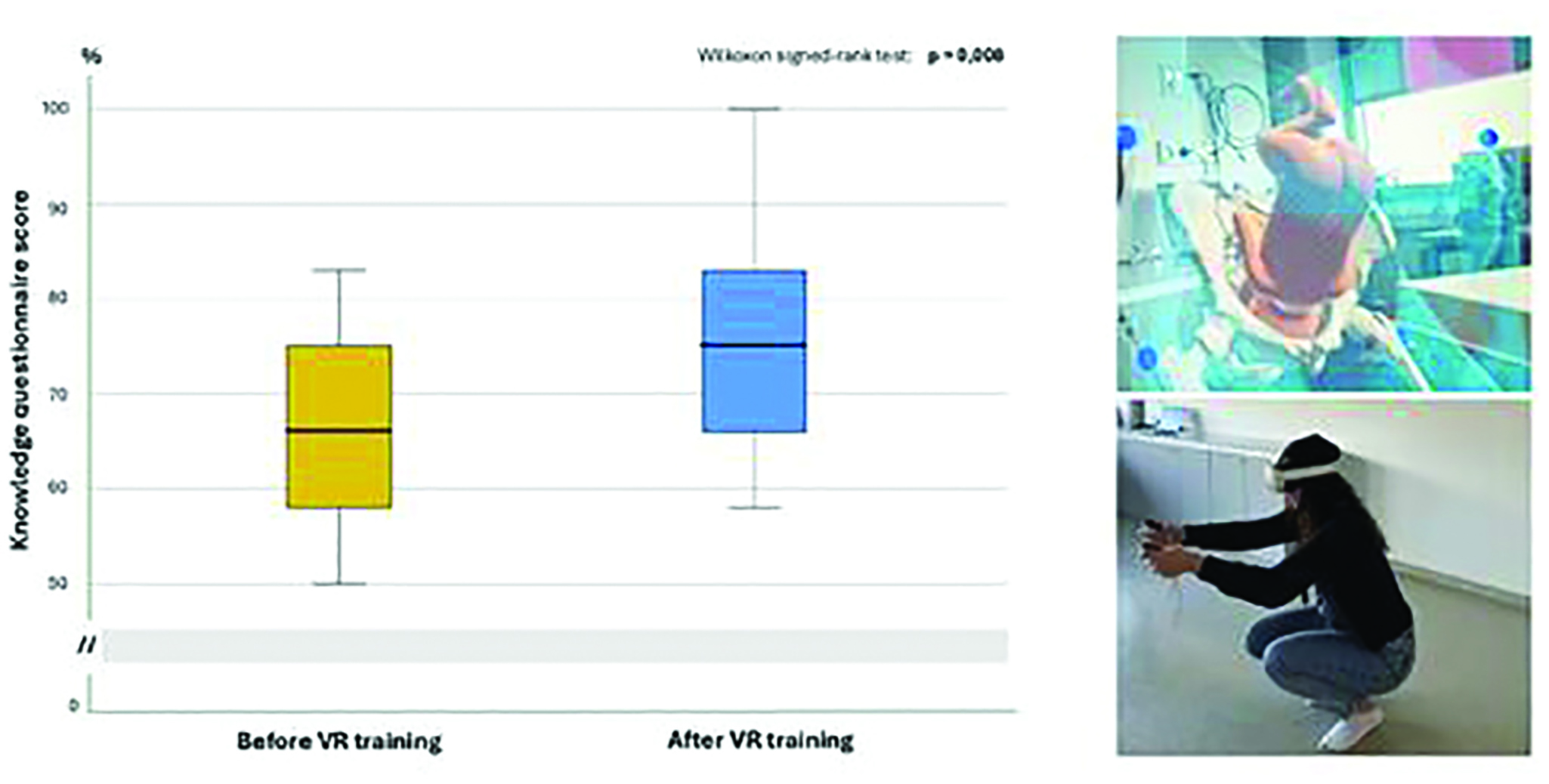
Box plots showing midwifery students’ knowledge levels before and after the VR-based educational experience. On the right, illustrative images of the VR training environment are presented.
Rachel Cichosz 1, Joseph Wheeler 1, Harjinder Kainth 1, Andrea Adjetey 1, Karishma Mann 1
[1]
Simulation based education (SBE) is integral to the Internal Medical trainee (IMT) curriculum (1). As a centre, we have developed a run-through series of courses delivered annually to IMT doctors across the region in years 1-7 of their training- IMTSim. The learning objectives for these courses are curriculum mapped and incorporate spiral learning to build on key topics. Data collected through pre- and post- course questionnaires suggest that trainees find our courses enjoyable and beneficial to their professional development. As data on the longer term benefits of SBE is limited, we felt it important to evaluate the ongoing impact of our courses via a ‘one year on’ impact survey.
A ‘one year on’ survey was developed for each of our individual IMT courses, allowing the questions to be specific to learning outcomes at different levels of training, and distributed to all doctors who attended our courses between August 2022 and 2024. Questions focused on the application of candidates’ learning during IMTSim to their every-day practice, and their thoughts on SBE as a whole. Qualitative data underwent thematic analysis by two individuals. Quantitative Ordinal Likert scale data was analysed using non-parametric statistical tests.
‘On the day’ surveys showed a significant difference in pre- and post-course ratings of knowledge of human factors, non-technical skills and the role of debriefing, as well as confidence ratings across a range of skills appropriate to specific learning outcomes at different levels of training. Around 200 doctors attend our IMTSim courses each year, and a total of 60 respondents contributed to our follow-up impact survey, with significant numbers reporting use of the skills/ themes explored during our courses in their everyday practice. When asked about SBE as a whole, significant numbers reported that they felt it was more impactful (87%) and more focused on the individual learner (78%) compared to more traditional teaching modalities.
Our data demonstrates immersive simulation has longer term impact on IMT doctors. Learning continued to be retained at one year post-course, with individuals going on to use and implement skills learned within their routine clinical practice.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. JRCPTB ‘Curriculum for General Internal Medicine (Internal medicine stage 2) training (2022)’. Royal College of Physicians. Available from: https://www.gmc-uk.org/-/media/documents/gim---internal-medicine--stage-2--2022-curriculum-final-july-2022_pdf-91723907.pdf. Accessed 23 April 2025.
Nikki Biggs 1, Alex Jolly 2, Russell McDonald 2, Lorraine Apps 1, Fielding Dave 2
[1]
[2]
WingFactors, a collaboration between aviation professionals and NHS educators, has been working with healthcare simulation faculties since 2020 and with Frimley Park’s Emergency Department (ED) since 2022. Drawing on aviation’s established use of Crew Resource Management (CRM) [1], CRM-trained airline pilots contribute to medical simulation debriefs – an approach that has supported a clearer focus on non-technical skills (NTS). This exposed a lack in NTS-specific training within Emergency Medicine (EM) and positive feedback from clinicians informed the development of a dedicated NTS curriculum and a bespoke training programme.
Our objective was to design and deliver a training programme that strengthened NTS competencies in EM by applying CRM principles and experiential learning in a structured format.
We achieved this by reviewing thousands of non-technical data points from over 100 observed simulations in EDs, and in collaboration with key EM educators, identified 6 core NTS modules: Communication, Leadership, Situational Awareness, Decision Making, Managing Bandwidth and Startle.
We designed each training day to incorporate medical, aviation and abstract simulation to heighten engagement and develop critical thinking and problem-solving skills [2].
The programme was structured around Kolb’s Experiential Learning Cycle [3]- concrete experience, reflective observation, abstract conceptualisation, and active experimentation. A model underpinned in both aviation and healthcare simulation, reinforcing shared learning processes and supporting the transfer of cognitive strategies.
These modules were delivered across three training days with CRM-trained pilots participating as observers and co-debriefers, offering valuable insights into behaviour, communication, and decision-making under pressure.
These have been piloted within the Kent, Surrey, and Sussex (KSS) Deanery, with modules paired as follows:
Day 1: Communication and Leadership
Day 2: Situational Awareness and Decision Making
Day 3: Managing Bandwidth and Startle
Feedback was overwhelmingly positive, with participants noting a greater appreciation for the NTS and the value of cross-industry perspectives:
“Such a valuable opportunity to look at NTS, not just as the ‘afterthought’ they usually are.”
“Very well delivered and lots of thought-provoking content.”
“Great to see human factors applied in a new way—this felt more relevant than some traditional teaching days.”
Nine further training days are planned across the next academic year within KSS, with potential expansion to other regions under review.
This programme illustrates how aviation-derived CRM principles can enhance NTS training in healthcare. Anchored in a shared experiential learning model, it provides a structured, scalable approach to strengthening and developing NTS in medical education.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Dekker S, Lundström J. From threat and error management (TEM) to resilience. Journal of Human Factors and Aerospace Safety. 2006;12.
2. Kahneman D. A perspective on judgment and choice: Mapping bounded rationality. American Psychologist. 2003;58,697–720.
3. Kolb DA. Experiential Learning Experience as the Source of Learning and Development. Englewood Cliffs, NJ Prentice Hall; 1984.
Jacqueline Driscoll 1, Katie Campion 1, Judith Ibison 1, Jane Roome 2, Holly Coltart 1, Gerard Gormley 3
[1]
[2]
[3]
This study shares phase one results of a two-phase participatory research project that joins simulation faculty (educators), GP trainees (learners), simulated participants (SP’s) and persons with lived experience of chronic conditions (patients) to co-design simulations for primary care. Phase one is concerned with understanding each group’s starting perspectives on, and to surface the tensions within, the current design of simulation scenarios. The purpose is to intervene in the existing epistemic underpinnings of simulation whereby faculty are the primary source of expertise on all aspects including scenario creation and to provide a route map for others on how co-creation can be enacted in this space.
Five focus groups were carried out. Two with patients, (N=10 participants), one with educators, (N=6), one with learners, (N=4), and one with SP’s, (N=5). The data was analysed thematically according to Braun and Clarke [1], with two team members independently coding each transcript before shared final themes generation. One member of the team then ensured all final themes were reflected in each individual’s coding and in each manuscript. Themes were also engaged with via the generation of I-Poems [2]. A reflexive log was kept throughout. Final themes were shared with participants at a co-production event for veracity checking.
Shared concerns across the focus groups included:
1. A desire for realistic scenarios that reflect illness complexity (“GP’s need to look at us holistically” [patient]), whilst recognising the tension between this and standardisation for learners,
2. The desire to improve representation (“we try not to lean into unhelpful stereotypes” [educator]), whilst balancing the importance of pattern recognition for junior trainees, and,
3. A greater emphasis on simulation for improving communication (“body language matters” [SP]).
Differences of opinion arose regarding:
1. How patients can best contribute to simulation practice (scenario creation versus debriefing learners versus briefing actors), and,
2. Concern from educators and trainees about the practicalities and risks of patient involvement (“There’s a danger their personal experience completely confounds everything else” [learner]).
The focus groups surfaced key tensions in current simulation practice with important questions of who is simulation for and what does meaningful safe engagement for all involve rising to the surface? These questions were the starting point for a subsequent co-production workshop with all stakeholders. While neat answers are beyond a single study, our work has advanced the naming of some key considerations for researchers and educators entering simulation co-production.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Braun V, Clarke V. Thematic Analysis: A Practical Guide. SAGE Publications; 2021.
2. Edwards R, Weller S. Shifting analytic ontology: using I-poems in qualitative longitudinal research. Qual Res. 2012;12(2):202–17.
This study was funded by the Association of Simulated Patient Educators (ASPE).
Merry Patel 1, Christopher Kowlaski 1, 2, Susannah Whyte 1, Emma Flint 1, J. L. Knight 3
[1]
[2]
[3]
Keeping children safe - by identifying safeguarding risks and taking prompt action - is part of all healthcare professionals’ roles [1]. However, practitioners experience numerous internal and external barriers to acting on suspected neglect - thereby delaying initial safeguarding conversations with parents [2,3].
Traditional safeguarding training is largely theoretical in nature - focusing on protocol, professional roles, and the law. Given the complexity of situations when neglect occurs, practical skills in early engagement of parents in safeguarding conversations are essential for safer outcomes for children, as is supporting practitioners to identify barriers to action. This study explored participants’ experience of, and the learning acquired from, a multi-agency simulation training on early childhood neglect.
Practitioners (n=34) from Health, Education, Local Authority and Voluntary Sector services attended a one-day simulation course - ‘Strengthening Practice Around Early Neglect’ (SPAEN). This ran four times (May-July 2024).
Scenarios engaged a simulated parent and a baby manikin and demonstrated increasing levels of physical, emotional, medical and educational neglect over several months.
Course evaluation data was collected with pre-and post-questionnaires - exploring knowledge, confidence and attitudes - and an online evaluation form. Semi-structured interviews were conducted three months post-course.
Analysis of quantitative data was conducted using SPSS Statistics for Windows (v29), and themes and subthemes within the qualitative data were identified using thematic analysis.
Quantitative data (n=34) demonstrated statistically significant (p<0.05) increases in: knowledge of neglect assessment tools; strategies for initiating safeguarding conversations; and confidence in explaining the Early Help process to parents. Online evaluation (n=27) confirmed high levels of engagement in both simulation training (4.96/5, average Likert scores) and multi-agency discussions (4.92/5).
Three overarching themes were identified from the semi-structured interviews (n=6), Figure 1: Impact on personal and team safeguarding practice; Perception of simulation-based learning; and multi-agency learning opportunities. Sustained learning was reported, as were actions being taken to address gaps in practice across agencies following the training.
Multi-agency simulation training is an invaluable tool for exploring uncomfortable conversations around early neglect. Study data demonstrated increasing practitioner knowledge, confidence and attitudes for this complex work and may support earlier conversations around safeguarding concerns. Ongoing opportunities for experiential training of this kind, both at undergraduate and postgraduate levels, is needed to further improve safeguarding practice. These should remain multi-agency in nature wherever possible.
Future involvement of parents and young people would complement course design, bringing greater understanding of parents’ perspectives of uncomfortable safeguarding conversations.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. HM Government (2023). Working together to safeguard children 2023: a guide to multi-agency working to help, protect and promote the wellbeing of children. London: Crown.
2. Lines L, Hutton A. Constructing a Compelling Case: Nurses’ Experiences of Communicating Abuse and Neglect. Child Abuse Review 2021;30:332–46
3. Solem L, Diaz C, Hill L. A study of serious case reviews between 2016 and 2018: what are the key barriers for social workers in identifying and responding to child neglect? Journal of Children’s Services. 2020; 15(1):1–14.
This study was part-funded by an ASPiH 2024-2025 research grant.

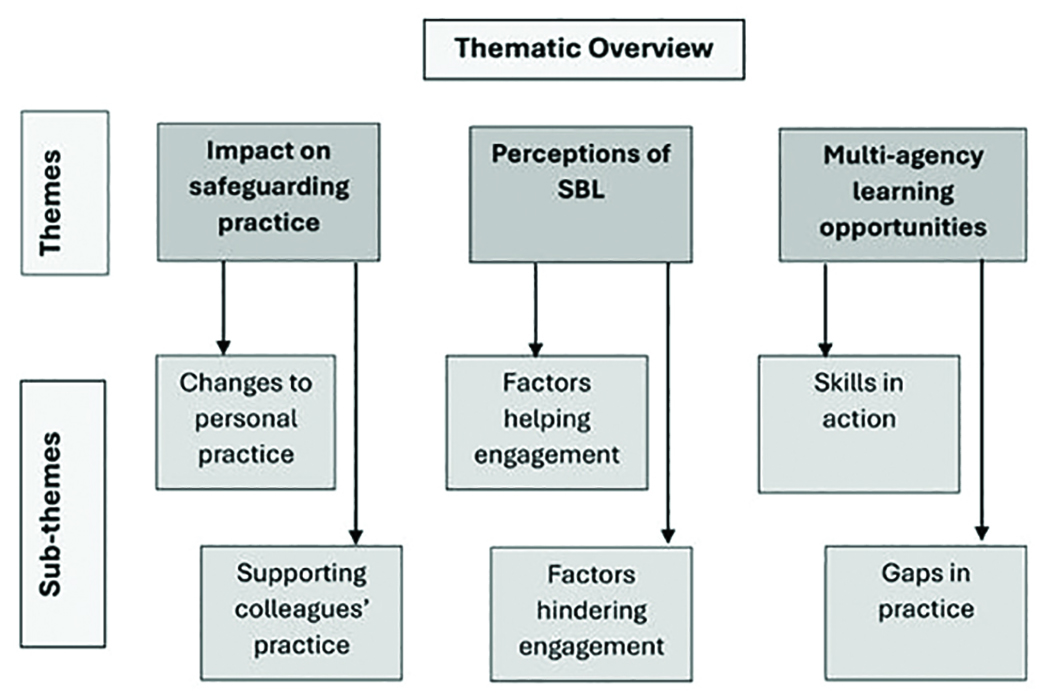
Semi-structured interviews: themes and subthemes.
Rebecca Ramsay 1, Sabah Hussain 1, Annabel Copeman 1
[1]
Simulation is a widely acknowledged method of training for healthcare practitioners often with a focus on improving safety and awareness of human factors [1]. Low fidelity in-situ simulation is an efficient way of improving performance [2] and is well established within our NHS trust, with a 30-minute session delivered fortnightly for resident paediatric doctors. Feedback identifies the majority of resident paediatric doctors across the deanery have some, but limited, opportunity to participate in simulation, with a learning gap regarding how to deliver these sessions themselves.
A two-hour session was held for 42 senior resident paediatric doctors to emphasise the value of simulation and teach them how to establish and deliver their own in-situ simulation sessions. This was both lecture-based teaching and a demonstration on how a simulation scenario was run and debriefed. Following this, participants had the opportunity to create their own scenarios in small working groups using a framework to address key points in crisis resource management and technical factors in simulation delivery. A pre- and post-course questionnaire was done to assess confidence in devising, delivering and debriefing simulation sessions using a 5 point Likert Scale from ‘not at all confident’ to ‘extremely confident’.
Pre-course data showed limited exposure to in-situ simulation with 62% of participants having occasional or rare involvement. We also identified reduced confidence levels across creation, delivery and debriefing of simulation. Post-course evaluation demonstrated a significant increase in overall confidence levels reported by 96% of participants. Our results also showed increased confidence of participants in all the specific areas evaluated. Participants rating extremely confident or very confident increased from 12% to 60% in devising, 17% to 68% in running, and 19% to 64% in debriefing an in-situ simulation session.
This highlights the impact a simple teaching session can have on empowering resident doctors with the knowledge to implement simulation practices in their own workplaces. Continuing to address this learning gap at resident doctor level, by providing ongoing teaching in simulation practices, will hopefully continue to improve confidence in delivering and increase use of in-situ simulation training throughout paediatric departments within the deanery, forwarding a culture of change in education practices to benefit a larger cohort of future resident paediatric doctors throughout their training. Our post-course evaluation also identified the need for additional teaching in the art of debrief and therefore has allowed us to plan a further teaching session to cover this.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Aggarwal R, Mytton OT, Derbrew M, et al Training and simulation for patient safety. BMJ Quality & Safety 2010;19:i34-i43
2. Norman G, Dore K, Grierson L. The minimal relationship between simulation fidelity and transfer of learning. Medical Education. 2012;46:636–647.
Pooja Kamath 1, Ritu Gupta, Shveta Kajal, Gemma Cash
[1]
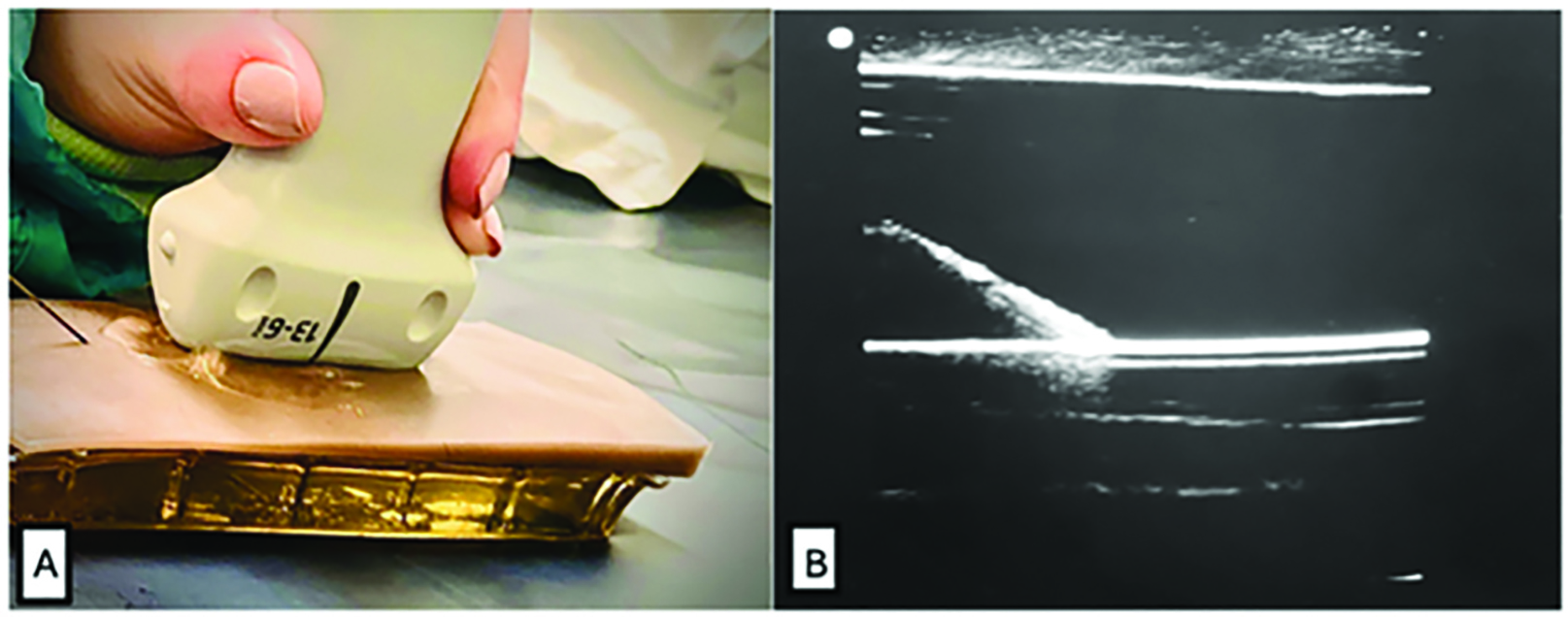
Ultrasound (USS) guided regional anaesthesia is a core skill in anaesthetic training. However, access to high-fidelity phantoms is often restricted by cost. Simulation-based training is well recognised for improving clinical performance [1] and low-cost phantoms offer significant educational value [2]. We developed an affordable, realistic, and reusable gelatine-based phantom in collaboration with the simulation team at our hospital. We evaluated its effectiveness through user feedback across different training levels.
The aim of our project was to assess the educational value, realism and usability of a low-cost USS Needling phantom that we developed in-house, amongst anaesthetic trainees and consultants. The phantom was made using gelatine, glycerine, silicon tubing (to simulate nerves or vessels), and a silicone skin to mimic anatomical realism as seen in Figure 1. It was used in a hands-on training workshop conducted in October 2024 with anaesthetic trainees (ST1-7), clinical fellows and consultants. Post workshop feedback was collected through surveys with questions focusing on realism, needle feel, ultrasound clarity and overall training value.
Our gelatine models were successfully used for ultrasound imaging and needling practice for cannulation and nerve blocks. Feedback was given by anaesthetists across on clarity, realistic resistance and educational value, with 96% (25/26) of respondents rating the model as a useful tool for needling practice. The selected combination of ingredients resulted in a model with excellent needle visibility, minimal track mark retention, and ease of ultrasound use, all while maintaining structural integrity and durability. The total cost of consumable materials for a single model was under £40, making it an affordable training tool. Additionally, our models are reusable and can be stored in the freezer for up to six weeks, then thawed for reuse without compromising quality.
Over the past decade, USS has become an indispensable tool in anaesthesia and intensive care, with NICE guidelines recommending its use for procedures such as central venous cannulation and peripheral nerve blocks. However, gaining competency in USS imaging and needle visualisation can be challenging.
Our model is an affordable, reusable, durable, and high-functional fidelity alternative to both existing gelatine models and expensive commercial phantoms. It provides a practical solution for ultrasound training in anaesthesia and critical care, and other junior trainee doctors in various specialities, ensuring accessibility without compromising educational value. The model also aligns with national curriculum goals on USS proficiency [3]. Feedback from trainees and experienced clinicians highlights its strong educational impact.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. McGaghie WC, Issenberg SB, Cohen ER, Barsuk JH, Wayne DB. A critical review of simulation-based medical education research: 2003–2009. Med Educ. 2010;44(1):50–63.
2. Walsh CD, Ma IWY, Eyre AJ, et al. Implementing ultrasound-guided nerve block in the emergency department: A low-cost, low-fidelity training approach. AEM Educ Train. 2023;7(5):e10912.
3. Royal College of Anaesthetists. 2021 Curriculum: Learning syllabus – Stage 3: Regional Anaesthesia.

Stephen Ojo 1
[1]
Simulated patients (SPs) are widely used in healthcare professions education (HPE) to enhance experiential learning, support assessment, and provide realistic, safe environments for developing clinical and communication skills [1,2]. Despite the acknowledged value of SPs in simulation-based education, there is limited consensus on what constitutes effective SP training [3]. The absence of standardised curricula raises concerns about consistency, educational outcomes, and quality assurance. This scoping review sought to explore: What does current literature reveal about the content, methods, and gaps in SP training within HPE?
A systematic scoping review was conducted following the PRISMA-ScR guidelines. Six electronic databases (MEDLINE, PubMed, CINAHL, Scopus, Web of Science, Cochrane Library) and grey literature were searched for English-language studies published up to May 2023. Studies were screened for relevance using pre-defined inclusion/exclusion criteria. Eligible sources reported on SP training in HPE. Data were extracted and analysed thematically to identify trends, gaps, and key training components.
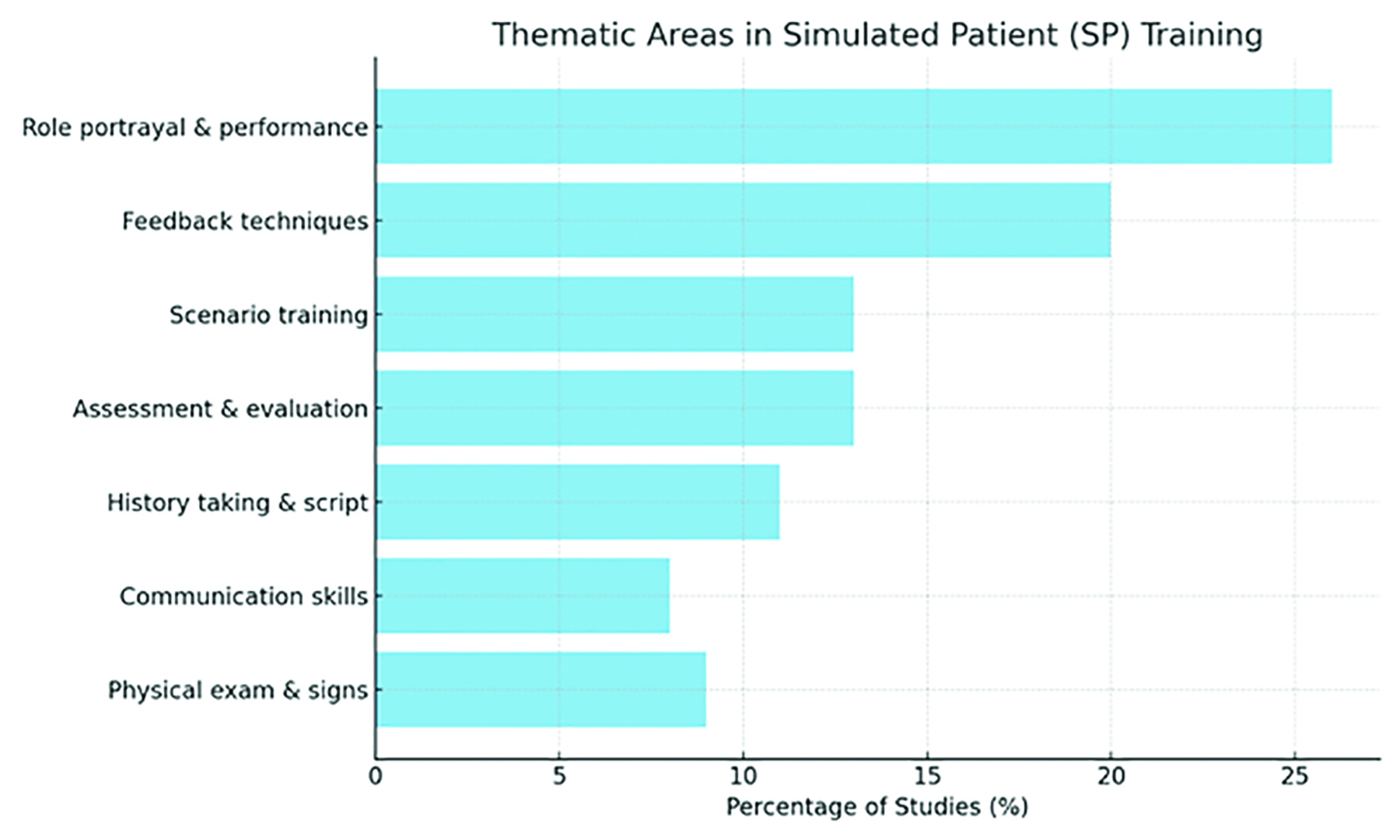
Of the 886 records screened, 25 studies met the inclusion criteria. Thematic analysis identified seven key areas of SP training (Figure 1): role portrayal and performance (26%), feedback techniques (20%), scenario engagement and patient interaction (13%), assessment and evaluation (13%), history taking and scripting (11%), communication skills (8%), and physical examination and signs (9%). Five categories of training methods emerged: structured training sessions, scripted briefs, technology integration, group activities, and observational feedback. Considerable variation in duration, content depth, and assessment methods was noted across studies. No universal framework for SP training was identified.
This review reveals broad variability in how SPs are prepared for simulation roles across institutions. While common training domains exist, there is a lack of standardised curricula, structured assessment tools, and reporting on long-term training outcomes. This variability may limit fidelity, learner experience, and inter-institutional benchmarking. Findings suggest an urgent need for evidence-informed, consensus-driven guidelines to improve SP training quality, consistency, and scalability across HPE.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Cleland JA, Abe K, Rethans JJ. The use of simulated patients in medical education: AMEE Guide No 42. Med Teach. 2009;31(6):477–486.
2. Nestel D, Bearman M. Simulated patient methodology: theory, evidence and practice. Wiley-Blackwell; 2014.
3. Greene G, Gough S. Train-the-simulated-patient programme: a UK evaluation. Clin Teach. 2015;12(6):403–407.

Michelle Holmes 1, Gary Francis 1, Claire Nadaf 1, Matt Lofthouse 1, Edit Bertalan 2, Jess Burt 2
[1]
[2]
The social care workforce must evolve to meet the changing needs of an ageing population, including increasing demand and delivery of homecare. Current training for home care workers is often theory-based, with homecare workers often feeling underconfident and lacking skills in some areas. Although simulation is widely used in healthcare for skill enhancement, it is underutilised in homecare training. This project aimed to explore the use of simulation-based education to upskill homecare workers to identify risks they may encounter in a client’s home.
This study was a pre-post mixed-methods study. Two high-fidelity simulations were undertaken, one for home care workers and another for home care managers. The simulation sessions were conducted in an activity of daily living suite. Both simulations were pre-briefed, recorded and debriefed using the STOP 5 hot debrief model [1]. Pre- and post-questionnaires included demographics, the 10-item General Self-Efficacy Scale, a bespoke measure on confidence with caring and communicating with clients, and the Student Satisfaction and Self-Confidence in Learning questionnaire [2]. Descriptive statistics were undertaken on pre and post surveys, the debrief was transcribed verbatim and analysed using thematic analysis alongside open-text comments from the questionnaires [3].
12 carers and 8 care managers took part in the simulation sessions. Four themes were developed across the quantitative and qualitative findings. Two themes focused on the use of simulation within home care: “Is Aggie okay?” – Risk Identification and client care, and “We’re in for it here” – Showcasing the challenges and difficulties of care. The other two themes focused on participants’ views on simulation as a training method: “Understanding the proper role of a carer” – Benefits of simulation in training, and “Obviously, we’re in a role play situation” – Challenges in engaging in simulation.
Simulation helped promote client-centered thinking, critical reflection, and peer discussion. It was seen as a useful complement to theoretical training, especially in preparing new carers. However, challenges such as suspension of disbelief, stress, and organisational barriers impacted engagement. To enhance effectiveness and minimise learner anxiety, the study highlights the importance of realistic scenarios, pre-briefing, and debriefing to ensure psychological safety and skill transfer.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Walker CA, McGregor L, Taylor C, Robinson S. STOP5: a hot debrief model for resuscitation cases in the emergency department. Clinical and experimental emergency medicine. 2020;7(4):259–66.
2. Pence P. Student satisfaction and self-confidence in learning with virtual simulations. Teaching and Learning in Nursing. 2021;17.
3. Braun V, Clarke V, Hayfield N, Terry G. Thematic Analysis. In: Liamputtong P, editor. Handbook of Research Methods in Health Social Sciences. Singapore: Springer Nature; 2019. p. 843–60.
Ghaniah Hassan-smith 1, 2
[1] Aston Medical School,
[2] Queen Elizabeth Hospital Birmingham,
Virtual reality (VR) simulation is emerging as a transformative tool in medical education, offering immersive, clinical experiences on demand. In neurology, VR and augmented reality have been shown to enhance learning of complex concepts such as neuroanatomy [1]. Additionally, immersive simulation paired with structured debriefing can uncover discipline-specific knowledge gaps otherwise difficult to identify [2]. However along with addressing educational needs, limitations including logistic expertise required in deploying VR sessions at scale require further work to demonstrate pragmatic utility of this technology in educating medical students. The work presented here therefore highlights a potential role for use of VR in medical education.
We integrated VR simulation into the undergraduate MBChB curriculum. Over 250 medical students in years 3&4 completed a VR scenario focused on acute bacterial meningitis management using Oculus Quest 2 headsets and Oxford Medical Simulation (OMS) software. Sessions included a structured debrief using the PEARLS framework. Faculty and facilitator reflections were also gathered.
High student engagement and positive feedback supported VR’s feasibility at scale. Year 3 students (n=48) reported strong satisfaction (83%) and alignment with learning outcomes (93%). They noted confidence gains in A–E assessment, escalation, and prescribing. Year 4 students (n=28) reported similar gains, though slightly lower satisfaction (75%). Both groups praised the immersive, user-friendly nature of the technology. Students valued improvements in prioritisation and structured clinical thinking. Suggested improvements included greater realism and more detailed pre-briefing and careful analysis re: authenticity when considering the role of VR compared to clinical placements.
Facilitators described the debrief as a vital opportunity for guided reflection, uncovering cohort-wide gaps in reasoning and task prioritisation. Notably, consistent deficits in neurologically-focused knowledge - notably in neuroanatomy, interpreting papilloedema and and recognising raised intracranial pressure signs as well as understanding CSF flow pathways - emerged across all groups but particularly notable in year 3.
Without cohort-wide exposure to such an immersive case, followed by focused debrief, such discipline-specific gaps would have been harder to detect at scale using traditional small-group simulation methods.
This project demonstrates that VR simulation can simultaneously strengthen clinical reasoning in neurology and serve as an effective diagnostic tool for educational gaps [3]. Operational strategies (including careful hardware planning, scheduling, and facilitator preparation) were crucial for success. These findings support wider adoption of immersive VR approaches to improve experiential learning and curriculum design in medical education, notably when covering complex topics like Neurology.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Sandrone S, Carlson CE. Future of neurology & technology: virtual and augmented reality in neurology and neuroscience education. Neurology. 2021;97(15):740–744.
2. Salik I, Paige JT. Debriefing the Interprofessional Team in Medical Simulation. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023.
3. Ryan GV, Callaghan S, Rafferty A, et al. Learning outcomes of immersive technologies in health care student education: systematic review of the literature. J Med Internet Res. 2022;24(2):e30082.
Philippa Beaumont 1
[1]
Simulation within physiotherapy education, is effective in developing many essential clinical and professional skills [1]. Standardised patients (SPs) help create high fidelity scenarios reflecting real-world environments, enabling students to practice person-centred care, communication skills and empathy, alongside hands-on clinical techniques [1]. The cost of hiring external actors, however, is one of the biggest barriers faced by Higher Education faculty staff [2]. While peer-peer simulation has been shown to be effective [1], our own experiences demonstrated a reluctance for many students to take on a performance role. Collaborative discussions with the university Acting programme highlighted several mutual benefits if the non-medically trained acting students were able to portray realistic patients and the physiotherapy students could ‘buy into’ character age differences. Maintaining psychological safety was also a priority.
This phenomenological study aimed to explore students’ perceptions of simulated learning, and the impact acting student SPs had on the learning experience. As qualitative methodologies are poorly represented in physiotherapy education simulation literature, a second aim was to add depth to our current knowledge.
70 physiotherapy students undertook a day of simulated learning in the University simulation wards. In groups of 6, students either led or observed 2 scenarios. 4 SPs of varying ages and medical presentations were portrayed by student actors, none of whom had previously been involved in simulation. A short training seminar helped the actors with clinical presentations. Following the simulation, all students were invited to participate in online focus groups. Thematic analysis was used to analyse data [3].
13 students participated in 3 focus groups. Physiotherapy participants reported the simulation supported the development of many skills including clinical reasoning, independent thinking, problem solving and teamworking. Although stressful, the simulation felt safe. It was an enjoyable and valuable learning experience. The acting students’ realistic portrayal of patients enhanced the session, and the physiotherapy students reported quickly ‘buying into’ patient characters, irrespective of the acting students’ age. Patient perspective feedback was particularly helpful, even though acting participants reported they found this aspect challenging. Acting participants also felt the simulation experience enabled them to create different, emotional characters and use improvisation skills to challenge the physiotherapy students as the scenarios developed (Table 1).
Results of this study add depth to the literature on simulation in physiotherapy education. It supports the use of acting students as SPs, offering an effective and cost-effective alternative to professional actors.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Lowe CM, Heneghan N, Herbland A, Atkinson K, Beeton K. KNOWBEST: The KNOWledge, BEhaviours and Skills required of the modern physiotherapy graduate including the future role of practice based learning. Chartered Society of Physiotherapy; 2022.
2. O’Shea O, Mulhall C, Condron C, McDonough S, Larkin J, Eppich W. A qualitative study of physiotherapy educators’ views and experience of practice education and simulation-based learning. 2023. International Journal of Healthcare Simulation. https://ijohs.com/article/doi/10.54531/HKOI8650
3. Braun V, Clarke V. Thematic Analysis: A Practical Guide. 7 ed. Los Angeles: Sage Publications; 2022.

| Physiotherapy students’ perceptions of the simulated learning experience | |
|---|---|
| Themes | Participant quotes |
| Simulation helped develop professional skills | “I had to really actively think on my feet” (P4) “It was great to collaborate with other people” (P1) “We had to problem solve” (P7) |
| Emotional aspects of sim | “It was amazing” (P4) “I was a bit more scared actually because it was more real” (P5) “A real confidence booster” (P7) |
| Environmental fidelity increased learning | “It was a fantastically safe space” (P1) “As close to a real clinical setting as it could be” (P2) “My first real experience of a hospital ward” (P3) |
| Simulation as an educational/ learning experience | “So many things were learnt” (P8) “The point was to learn and that was clear” (P6) “I did get valuable learning from watching” (P1) |
| Physiotherapy students’ perceptions of acting students portraying SPs | |
| Skills of acting students in portraying patients | “The acting was absolutely incredible and far exceeded what I was expecting” (P2) “The acting students were taking their roles really seriously” (P9) “I found very easily that I slipped into looking at him as though he was an 82-year-old” (P11) |
| Enhanced learning experience | “Actors made it feel real” (P4) “It immediately put you in that professional frame of mind” (P2) “Looking at patient care, patient-centred care and how we’re actually treating the patient” (P5) |
| Comparisons with peer-on-peer scenarios | “If you do like mess up and you’re working with a friend, it’s like, yeah, OK we’ll give you a little bit of help” (P4) “There was a sense of realism from the acting patients that maybe we wouldn’t have got from like our peers” (P10) |
| Acting student opinions of the simulation experience. | |
| Simulation as a learning experience for actors | “I found it harder to criticise them” (P12 “It was certainly different to things I’ve done in the past” (P13) “I couldn’t overdo it, but I couldn’t underplay it either” (P12) “I found being that vulnerable quite difficult, even though it was fake” (P12) |
| Professionalism of physiotherapy students | “There was a lot of trust involved, but there wasn’t any point where I felt I wasn’t safe with it” (P12) “I didn’t feel like I needed that safety net of the lecture” (P13) “They all did brilliantly” (P12) |
| Actors reacting to changing situations | “Ohh, this is too easy for them. And so I made it more difficult” (P13) “I made it harder in the afternoon” (P12) |
Sophie Jones 1, Caroline Storey 1
[1]
Medical students at University Hospitals Dorset have an 8-week placement in Paediatrics, where they are expected to develop their skills in history taking and examination of children. Previously these skills were introduced through lectures, prior to students commencing placement, where they would be expected to practice their new skills on patients. Informal feedback showed that students found this daunting. Literature on this topic shows that students find an abrupt transition from theory to practice with real patients to be challenging [1]. To address this, we designed a simulation session to occur prior to clinical placements, where we gave students the opportunity to practice their skills in a safe and low-pressure setting.
1) To increase student understanding of paediatric history taking and examination. 2) To increase student confidence assessing children prior to clinical placements.
29 students attended a simulation session covering common paediatric presentations, including wheeze, reduced oral intake and abdominal pain. Students could take a history from a simulated parent and examine the paediatric manikin. The scenarios were designed to be slow-paced, with opportunity to ask the group or faculty questions throughout, to prioritise problem-solving in a psychologically safe manner. A learner-led debrief was then followed by relevant micro-teaching by a consultant Paediatrician.
After the session, 100% of students agreed that simulation was a useful way to learn paediatric history taking and examination. 100% of students also felt more prepared to clerk patients during their placement after practicing their skills during simulation. When surveyed again at the end of their placement, 92% agreed that their confidence in seeing patients was improved as a result of participating in this session. Informally, staff working in the department reported they observed increased willingness for the students to see patients themselves early in the placement when compared to previous cohorts who did not have this intervention.
Simulation is a learning tool that embodies experiential learning theory, whereby students learn through a cycle of experience, reflection and experimentation [2]. Feedback from students and staff showed that simulation was a valuable method of teaching the skills of paediatric assessment, and that it prepared students well for their upcoming placement by increasing their confidence and willingness to assess real patients. This project could be enhanced with formal data collection around staff experiences of working with students who have had early exposure to simulation in contrast to traditional methods of teaching.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Dornan T, Bundy C. What can experience add to early medical education? Consensus survey. BMJ [online]. 2004;329(7470):834. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC521574/ Accessed 16 April 2025.
2. Kolb, DA. Experiential learning: Experience as the source of learning and development. 2nd ed. New Jersey: Pearson Education; 2015.
Jack Brown 1, Aonghas Michie 1, Jhiamluka Solano-Velasquez
[1]
Early and appropriate use of Non-Invasive Ventilation (NIV) reduces patient mortality [1]. Simulation-based multidisciplinary education enhances realism, teamwork, and clinical preparedness in acute care settings [2]. Embedding Critical Care Outreach (CCOT) teams into simulation training mirrors real-world escalation pathways and strengthens clinical decision-making. However, resident doctors often report low confidence and high anxiety when managing NIV, primarily due to limited formal training - a pattern seen in the UK [2]. Addressing this gap is essential to optimise acute patient care. We collaborated with CCOT and peer-led teaching initiatives to deliver simulation-based sessions focused on recognising suitable patients, setting up, and initiating NIV [3]. We aimed to evaluate the benefits of interdisciplinary, CCOT-integrated simulation in developing skills for managing respiratory failure.
A quasi-experimental pre- and post-test study involved 16 participants, including foundation doctors, internal medicine trainees, and specialty registrars. All doctors attending the sessions were eligible to participate. The intervention comprised a simulation-based workshop delivered with CCOT, using real NIV equipment. Participants assessed a simulated patient using case-based vignettes, set up and initiated NIV pressure settings, and reassessed therapy effectiveness. CCOT actively guided escalation protocols, clinical decision-making, and team communication throughout the scenarios, providing real-time feedback. Data were collected before the programme and two weeks after the simulation. An 8-point Likert scale assessed self-rated confidence, and the Six-Item State Anxiety Scale (SAS) measured anxiety. Ethical approval was not required as the project was part of service improvement.
Among participants, 91.7% had not received previous formal NIV training. Baseline confidence averaged 2.7/5, improving to 4.2/5 post-simulation, Table 1. Anxiety scores decreased from 16/24 to 11.7/24. Overall, confidence increased by 56% and anxiety reduced by 27%, exceeding initial targets. Notably, 93.8% of participants reported that CCOT input benefited their learning experience, describing it as pivotal for understanding effective escalation processes, multidisciplinary communication, and the practical application of NIV management.
Embedding Critical Care Outreach into simulation-based education significantly improved resident doctor confidence and reduced anxiety in managing NIV. Positive feedback regarding CCOT involvement highlights the value of incorporating real-world multidisciplinary escalation pathways into training. Adopting this model could enhance national NIV training standards, strengthen acute care teamwork, and improve patient safety. Limitations include the small sample size and short follow-up period; however, immediate educational impacts were significant. Integration into local postgraduate teaching is planned to sustain and expand the benefits observed.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Plant PK, Owen JL, Elliott MW. Early use of non-invasive ventilation for acute exacerbations of chronic obstructive pulmonary disease on general respiratory wards: a multicentre randomised controlled trial. Lancet. 2000 Jun 3;355(9219):1931–5. doi: 10.1016/S0140-6736(00)02323-0.
2. Hare A, Simonds A. Simulation-based education for non-invasive ventilation. Breathe (Sheff). 2013 Dec;9(5):366–74. https://breathe.ersjournals.com/content/9/5/366
3. Moerer O, Harnisch LO, Herrmann P et al. Patient-ventilator interaction during noninvasive ventilation in simulated COPD. Respiratory Care. 2016;61(1):15–22. doi: 10.4187/respcare.04141.

| Outcome Measure | Pre-Simulation | Post-Simulation | Change |
|---|---|---|---|
| Confidence Score (mean,/5) | 2.7 | 4.2 | +56% increase |
| Anxiety Score (mean,/24) | 16.0 | 11.7 | -27% reduction |
| Participants with prior formal NIV training (%) | 8.3% | — | 91.7% without prior training |
| Participants finding CCOT input beneficial (%) | — | 93.75% |
Raymond Effah 1, Ramnauth Ramkrishna 1, James O’Brien 1, Phoebe Rivers 1, Oscar Atkinson
[1]
Point-of-care ultrasound (POCUS) is increasingly becoming an integral component of healthcare due to its capability for swift diagnosis, aiding management plans and improving accuracy and decreasing complications of bedside procedures. POCUS training has advanced over recent years with many centres now offering accredited courses and implementing structured training to improve clinician’s ultrasound skills. According to the literature, frequent barriers to accreditation include lack of supervisors and lack of time to complete supervised scans [1], by running a “Introduction to POCUS” course it was our aim to reduce these barriers.
We organised a monthly “Introduction to POCUS” session for resident doctors to teach how to use ultrasound using simulation via Bodyworks Eve and SonoSim. Residents were taught how to use an ultrasound probe, perform ultrasound guided cannulation and were shown different pathologies involving heart, lung, and abdomen.
Several sessions were held between 2022 and 2024 for interested resident doctors. In total 45 participants attended. The majority were FY1 and FY2 doctors (97%), with most having no previous ultrasound experience (67%). Participants were asked to rate their confidence in carrying out bladder scanning, ultrasound guided cannulation, and diagnosing DVTs and lung/abdomen pathology. 33 doctors completed both the survey before and after the session, with all showing statistically significant improvements (p < 0.01) in all measured parameters using the paired t-test. Interestingly, doctors cited access to probes, supervision, and their lack of practical knowledge were the main barriers to being able to use or learn ultrasound.
Our study has shown that early exposure to ultrasound may be beneficial for doctors in improving their clinical practice and development of new skills. All participants that participated believed they were more likely to use ultrasound in their clinical practice going forward. The use of ultrasound guided cannulation may also reduce the burden on departments such as vascular access or the anaesthetics, that may be asked to assist during difficult cannulation. We are hoping to reduce the barriers to accessing ultrasound and practising the skills residents have learned over the next coming months by implementing more informal monthly sessions where doctors will be given access to use the simulation equipment. Lastly, we will arrange future accreditation courses in focussed acute medical ultrasound, to allow them to take the first steps to becoming accredited.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Tan MZ, Brunswicker A, Bamber H, Cranfield A, Boultoukas E, Latif S. Improving lung point-of-care ultrasound (pocus) training and accreditation - A multidisciplinary, multi-centre and multi-pronged approach to development and delivery using the Action Learning Process. BMC Medical Education. 2024 Jul 2;24(1). doi: 10.1186/s12909-024-05653-2.
Naomi Shiner 1, Kacper Badyn 1, Emma Edwards 1, Derek Chebsey 1, Charlotte Gebbett 1
[1]
Student radiographers must be proficient in appraising diagnostic images for clinical manifestations and taking appropriate action [1]. Chest X-rays (CXR’s) are the most frequently performed imaging examinations in the UK [2]. presenting complex anatomy and numerous pathologies that challenge students. Simulation-based education, particularly gamification, has shown promise in enhancing engagement and achieving learning outcomes [3]. This study evaluates the effectiveness of a co-produced, creatively designed simulation in improving CXR proficiency among third-year radiography students.
Ethical approval was obtained from the university’s Faculty of Medicine and Health Sciences ethical committee. This study involved the development and implementation of CXR RadPath, co-produced and led by a student radiographer, academic supervisor, and the faculty simulation team. The tool was designed to enhance CXR interpretation through gamification. Encompassing the use of QR codes to access and explore various radiographic images, six key categories related to CXR interpretation which would be a skill required in clinical practice, and an element of competition. The game pro-actively promoted students to work collaboratively and learn together. Participants completed pre- and post-simulation assessments to measure improvements in proficiency and confidence. Quantitative data were collated and evaluated using descriptive statistics to assess changes in image analysis competence. Qualitative data were thematically analysed to evaluate students’ perceptions of gamification and its effectiveness in supporting radiographic education.
Students demonstrated significant improvement in CXR interpretation proficiency after using the gamified version of reporting images in clinical practice. Significant changes were noted following its use with 83% of students progressing from “Moderately Confident” to “Very Confident” in their ability to interpret CXR’s. A further 67% of students improved in identifying abnormalities on CXR’s with a mean score improvement of 31%. Qualitative themes found the simulation to be engaging, effective, and beneficial for enhancing systematic radiographic analysis skills, fostering creativity, and promoting a culture of collaborative learning.
The use of a co-produced and creatively designed gamified version of reporting chest X-rays significantly improves students’ confidence and accuracy in CXR interpretation. Co-production allowed the simulation design pedagogy to be taught while aligned to student motivations. This collaborative approach ensured that the educational strategies were not only pedagogically sound but also engaging and relevant to the students, thereby enhancing their learning experience and outcomes. These significant outcomes have led to further development of this student-led project, expanding into other areas of image interpretation (axial and appendicular skeleton) and being implemented with other cohorts.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Health Care and Professions Council. Standards of Proficiency: Radiography [Internet]. 2023. Available from: https://www.hcpc-uk.co.uk/globalassets/standards/standards-of-proficiency/reviewing/radiographers---new-standards.pdf
2. Gefter WB, Post BA, Hatabu H. Commonly Missed Findings on Chest Radiographs: Causes and Consequences. Chest. 2023;163(3):650–661.
3. D’Amore A, James S, Mitchell EKL. Learning styles of first-year undergraduate nursing and midwifery students: A cross-sectional survey utilising the Kolb Learning Style Inventory. Nurse Educ Today. 2012;32(5):506–515.
Sawsan AlMukdad 1, Aya Elhage 1, Lily O’Hara 2, Mohamed Izham Mohamed Ibrahim 1, Banan Mukhalalati 1, Alla El-Awaisi 1
[1]
[2]
Interprofessional education (IPE) equips health profession students for collaborative practice [1]. Simulation-based IPE allows students from different professions to learn together in simulated scenarios, enhancing teamwork and patient care [2]. This study aims to conduct a comprehensive evaluation of a simulation-based IPE activity focused on disaster preparedness and management for health profession students [3].
An IPE simulation focused on disaster preparedness and management phases (mitigation, preparedness, response, recovery) was conducted for undergraduate health profession students. Students, assessors, and standardized patients (SPs) participated. Data was collected from students using the Team Perception of Collaborative Care, from assessors using the Modified McMaster-Ottawa Scale, and from SPs using the Standardized Patient Team Evaluation Instrument.
Thirty-three students, 13 assessors, and 8 SPs participated. Students self-reported positive perceptions of teamwork, with over 90% agreement across all domains. Assessors’ ratings corroborated these findings, with over 80% of students scoring at or above expectations in all domains. While not statistically significant, a trend towards improved performance across cases suggested a learning curve effect. Students with prior IPE experience demonstrated significantly better performance, with a mean score of 2.42 (95% CI: 2.24-2.60) compared to 2.06 (95% CI: 1.80-2.33) for students without prior IPE experience. Similarly, students who completed a practice placement achieved a higher mean score of 2.48 (95% CI: 2.30-2.65) compared to 2.12 (95% CI: 1.86-2.37) for those who did not. SPs evaluations aligned with these positive trends, with over 70% strongly agreeing or agreeing on positive interprofessional practice behaviors.
This study provides evidence supporting the integration of IPE into health profession curricula to enhance disaster preparedness and interprofessional collaboration.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Centre for the Advancement of Interprofessional Education. What is Interprofessional Education? [Internet]. 2006 [cited 2025 Apr 27]. Available from: https://www.caipe.org/about
2. World Health Organization. Framework for Action on Interprofessional Education & Collaborative Practice [Internet]. 2010 [cited 2025 Apr 27]. Available from: https://www.who.int/publications/i/item/framework-for-action-on-interprofessional-education-collaborative-practice
3. Alfred D, Chilton J, Connor D, Deal B, Fountain R, Hensarling J, et al. Preparing for disasters: education and management strategies explored. Nurse Educ Pract. 2015;15(1):82–9.
Alice Churchill 1, Lissa Darby 1, Lisa Cottenham 1, Stephen Downey 1
[1]
Simulation training is a teaching method which uses a controlled environment to “recreate a clinical experience without exposing patients to the associated risks” and allows students to practise skills and gain confidence in clinical scenarios [1]. Simulation training is highly effective at enhancing the learning and clinical competency of individuals working in a healthcare setting [2]. Over the past year we, a group of FY2 doctors, delivered “virtual on-call” sessions for final year medical students and foundation doctors, providing them with bleeps and a simulation of an on-call shift.
Teaching sessions were run for groups of up to 18 students/foundation doctors. Feedback was gained before and after the sessions both verbally and with a written form. Three cycles were completed, using feedback to make adjustments and optimise the delivery of virtual on-call teaching. Sessions were delivered to 1 cohort of 31 new FY1 starters, and to 5 different cohorts of 64 final year medical students across the year. All 12 sessions were run in a single centre (a rural district general hospital).
The number of students feeling confident about on-calls increased after all teaching sessions (Figure 1), with a more than 50% overall increase in subjective confidence. With the addition of a contactable ‘med reg’, there was also a significant increase in confidence using SBAR handovers and escalating to seniors. The overall feedback was overwhelmingly positive with comments such as “Would love more sessions like this”, “Really great, please do more of these sessions”, and “The best teaching session we’ve had during med school”.
Virtual on-call simulation teaching is a very valuable resource for developing confidence on-call in final year medical students and new foundation doctors. Learning from feedback is crucial to improving the quality of the teaching and producing better outcomes for the students. Key components that increased students’ confidence included providing the opportunity to bleep for advice, instead of simply verbalising that intention, as well as adding facilitated elements to enable direct feedback. Developing a structured introduction to the sessions helped them to run smoothly and the students to get the best out of the experience. With the incredibly positive feedback for these teaching sessions being noticed by the medical school we are in the process of making this part of the final year curriculum for all medical students at Exeter Medical School.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Maran NJ. Glavin RJ. ‘Low- to high-fidelity simulation – a continuum of medical education?’. Medical Education. 2003:22–28.
2. Elendu C, Amaechi DC, Okatta AU, Amaechi EC, Elendu TC, Ezeh CP, et al. The Impact of simulation-based Training in Medical education: a Review. Medicine [Internet]. 2024;103(27):1–14. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC11224887/
We would like to thank Dr Timothy Mason, who first introduced the concept and whose consistent support and enthusiasm encouraged us to develop the sessions. We also thank the whole NDDH Medical Education team and the Enhance team for providing resources and logistics help. We are also very grateful for those who have volunteered their time to help facilitate sessions over the year.

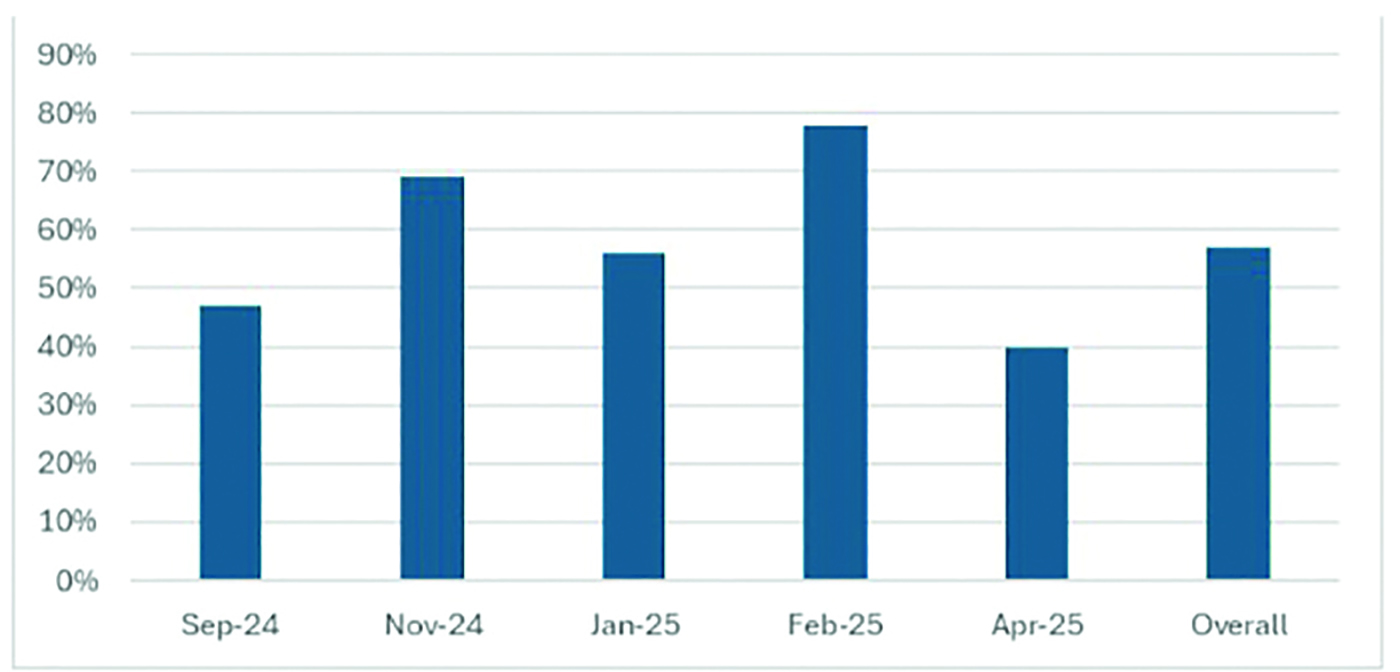
Graph showing percentage increase in number of students feeling confident for on-calls from pre- to post-session, in each 'block' of sessions and overall.
Giuseppe Leontino 1, 2
[1]
[2]
The rapid expansion of simulation-based education (SBE) in UK nursing curricula has been driven by factors like the pandemic, updated NMC standards and placement shortages. Furthermore, financial constraints, supply chain issues and technological advances, are reshaping the way simulation is planned and delivered, hindering, at times, SBE implementation. Henceforth, it is imperative to deliver high-quality simulation for impact to ensure the current workforce is prepared to face the challenges of the future [1].
Improvement science methodologies could represent a scalable solution as they offer structured, evidence-based approaches to planning and delivering simulation programmes, ensuring sustainability, operational resilience and simulation effectiveness [2].
This abstract presents the application of improvement science tools to the planning and delivering of an SBE project, aiming to increase awareness and pave the way for a future-proof roadmap to sustainable and impactful SBE.
Different methods for improvement were employed to plan, deliver and evaluate a four-week simulated placement for around 40 undergraduate nursing students, Table 1.
Evaluation focussed on students’ perceived competence and confidence on specific clinical skills, including the use of EPR systems. A mixed-method pre-/post-design was employed, and data were collected using anonymised questionnaires, debriefs and informal discussions to capture emergent issues and insights. T-test, Analysis of Variance (ANOVA) and Statistical Process Control (SPC) were used to analyse quantitative data. Ethical approval was obtained for the study.
The application of the Model for Improvement (MFI) allowed the team to plan and evaluate the project which resulted in data-driven decisions and successful outcomes [3]. In fact, results showed:
Confidence in learning improved to 97% from 68% post/pre-test
Statistical significance p<0.05 for perceived competence was detected across 6/11 proficiencies tested and for 7/7 EPR systems parameters investigated in the Before/After groups
Overall post-test competence was higher than pre-test across all proficiencies.
Table 1 shows the application some of the tools employed and their benefits.
Embedding improvement-science into SBE offers an evidence-based guidance that ensures rigour, effectiveness and a learner-centred focus. Thus, leading to enhanced planning accuracy, educational impact, and operational resilience. Widespread uptake of improvement science in SBE will drive more effective, sustainable, and responsive simulation programmes, ultimately improving nurse preparedness and potentially patient care.
Future work should focus on:
Scoping the current application of the MFI in simulation programmes
Integrating the MFI into SBE more systematically
Evaluating faculty’s experience in using the tools
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable
1. Dalwood P, Haig A, Sykes M, Eaton J. Simulation fidelity and nursing performance: a systematic review. Nurse Educ Pract. 2018;31:72–77.
2. Langley GJ, Moen R, Nolan KM, Nolan TW, Norman CL, Provost LP. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. 2nd ed. San Francisco: Jossey-Bass; 2009.
3. Reed JE, Howe C, Doyle C, Bell D. Simple rules for evidence translation: insights from the SHIFT-Evidence framework. BMJ Qual Saf. 2018;27(8):672–680.

| Tool | Adoption | Benefits |
|---|---|---|
| Process Mapping (PM) | • Collection of data • Students’ sign in process • Day to day running of the simulation • EPAD completion • Faculty upskilling |
Process control Implemented for all the main workstreams to promote process visualisation, encouraging comprehension, facilitating discussions, elimination bottlenecks and redundant steps. |
| Action Effect Method (AEM) | • Kit and equipment required • Learning resources needed • Tracking and monitoring • Critical interventions to PDSA • Programme evaluation |
Resources and requirements Linked aims to required actions and resources needed, allowing the team to identify elements to implement and critical aspects warranting related testing cycles. |
| PDSA | • Scenario development • EPR system integration • Attendance • Evaluation completion • Proficiency tracking |
Responsiveness and effectiveness Cycles enabled rapid cycle testing of changes evaluating their immediate impact, and refining the simulation environment in near real-time |
Aruchana Maheswaran 1, Colette Davidson 1, Hannah Cheney Lowe 1, Joanna Morley 1, Stephen Hamshere 1
[1]
In situ simulation improves participants’ ability to respond to high-stress situations, increases confidence, and enhances interprofessional communication [1]. Simulation has increasingly been recognised by senior medical leadership as a valuable tool in enhancing patient safety. However, our experiential understanding showed that ad hoc simulation sessions across wards were often subject to cancellations and last-minute changes. Additionally the use of generic scenarios did not always reflect the specific clinical challenges faced by individual teams. These issues prompted a reassessment of our approach. We aimed to explore whether embedding a collaborative, ward-specific in situ simulation course would improve engagement, reduce cancellations, and better meet learning needs.
We selected one cardiology ward (6D) to pilot a focused, 6-week in situ simulation programme. A multidisciplinary working group was formed, including members of the simulation team, the ward manager, the practice development nurse (PDN), and a consultant cardiologist. Together, we conducted a targeted learning needs analysis and co-designed six bespoke simulation sessions. A fixed time and location were agreed upon in advance to ensure consistency and support from the ward. Simulations were run every 2 weeks over a 3-month period. Key learning points and safety issues identified during debriefs were compiled in a patient safety report and shared with the wider team. In parallel, we continued to run single, one-off simulation sessions on seven other wards, scheduled at the ward’s most suitable time by corresponding ward managers.
Our dedicated 6D programme achieved a 0% cancellation rate, with strong and consistent attendance across multidisciplinary team (MDT) members, Figure 1. In contrast, the ad hoc sessions across other wards experienced a 57% cancellation rate, with reasons including staffing shortages, lack of available space, or staff being committed to other teaching. Attendance records also showed a greater number of staff and spread of the MDT trained on 6D when compared to the rest of the hospital. Subjective feedback demonstrated that in general all staff recognise the benefit of in situ sim education to the clinical team and were willing to take part finding it both “useful” and “exciting”.
This project demonstrates that co-designing simulation with stakeholders leads to better attendance, fewer cancellations, and more bespoke learning. Structured, ward-integrated simulation not only enhances engagement but also supports a culture of continuous learning and safety. Moving forward, we aim to evaluate whether this approach contributes to sustained behavioural change within ward teams, using the Kirkpatrick evaluation model.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Manggala SK, Tantri AR, Sugiarto A, Sianipar IR, Prasetyono TOH. In situ simulation training for a better interprofessional team performance in transferring critically ill patients with COVID-19: a prospective randomised control trial. Postgraduate Medical Journal [Internet]. 2022 Aug 1;98(1162):617–21. Available from: https://pmj.bmj.com/content/98/1162/617
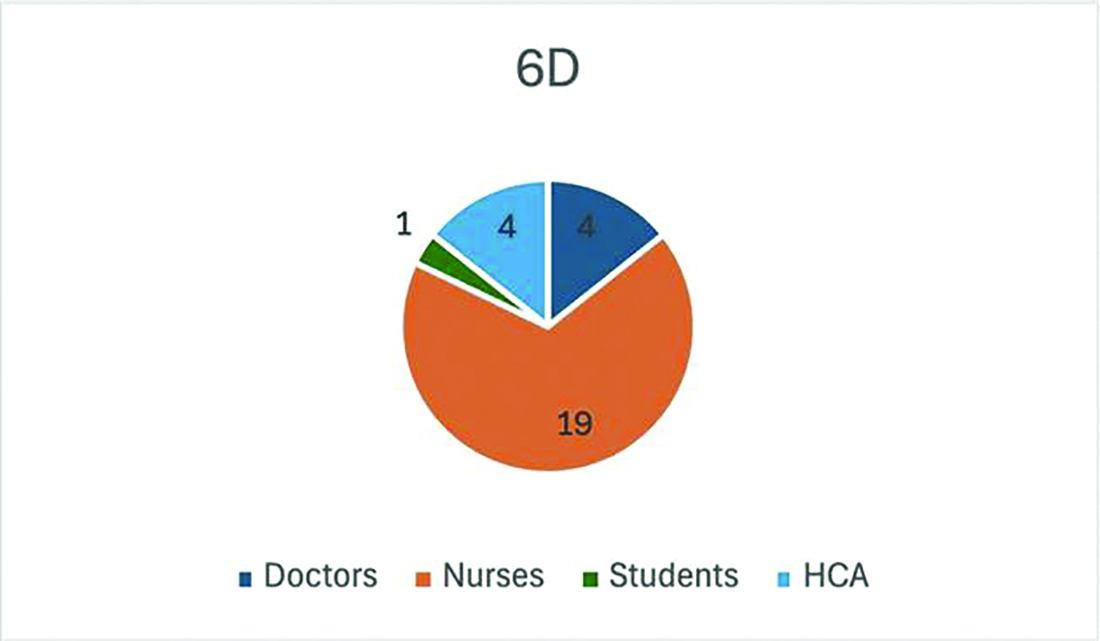
Julia Pasztorova 1, Saifullah Mohamed 1, Adrian Levine 2, Emma Low 1
[1]
[2]
The number of knife crime-related serious injuries is growing across the UK [1]. Our questionnaires demonstrated that even senior clinicians lack confidence in managing chest wall trauma and making a time-critical decision to perform a resuscitative thoracotomy. We have piloted the Resuscitative Thoracotomy course designed by C.A.R.E. (Cardiac Advanced Resuscitation Education LLC), to train the frontline multidisciplinary team of ED doctors, surgeons, intensivists, anaesthetists and senior nursing staff. Candidates learn to perform bilateral thoracotomy, resuscitative thoracotomy, pericardiotomy, internal cardiac massage, internal defibrillation, and to manage underlying injuries.
Our first pilot course in October 2024 involved four hours of e-learning, followed by a half-day in-person course. The in-person course involved five high-fidelity simulation moulages delivered in an ASPiH-accredited simulation centre, interspersed with small-group clinical skills training. Candidates completed a self-assessment questionnaire, where they rated their confidence in performing six key clinical skills using a five-point Likert scale [2]. This was completed before commencing the pre-course e-learning, and repeated after completing the course.
We revised the course structure and content to reflect the feedback from candidates. Our second course in April 2025 was extended to a full-day course with seven moulage scenarios with an increased simulation fidelity. A practical wet lab station was introduced with a hands-on element of managing trauma on porcine heart and lung blocks. All candidates were involved in practical skills sessions with medical meat led by cardiothoracic surgeons. Pre and post-course self-assessment questionnaires were completed as described above, in addition, candidates were asked to assess their confidence with relevant non-technical skills using a Likert scale.
Feedback was collected from twenty-four candidates across two courses. The feedback from candidates revealed a recognition of a lack of necessary skills to perform clamshell thoracotomy, despite previous experience managing penetrating injuries amongst the cohort. Candidates reported improved confidence in performing the core technical skills in all six domains (Table 1). Candidates attending the April course also reported increased confidence in all four key non–technical skills (Table 1).
Our overall aim is to improve access to focused training for frontline clinical staff who are increasingly likely to encounter patients with chest trauma. The high-fidelity simulations aim to empower senior clinicians and equip them with the necessary skills to deliver time-critical and potentially life-saving interventions. We are committed to the continuous evaluation and improvement of the simulation activity delivered within the course, in line with ASPiH standards [3].
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Allen G, Wong H. Knife crime statistics. commonslibraryparliamentuk [Internet]. 2025 Jan 27;CP4304(SN4304). Available from: https://commonslibrary.parliament.uk/research-briefings/sn04304/
2. Sullivan GM, Artino AR Jr. Analyzing and interpreting data from likert-type scales. J Grad Med Educ. 2013;5(4):541–542. doi: 10.4300/JGME-5-4-18
3. Diaz-Navarro C, Laws-Chapman C, Moneypenny M, Purva M. The ASPiH Standards - 2023: guiding simulation-based practice in health and care. Available from: https://aspih.org.uk

| October 2024 (pilot) N=8 |
April 2025 N=16 |
|||
|---|---|---|---|---|
| Skill | Pre-course | Post-course | Pre-course | Post-course |
| Knowledge of existing guidance for chest wall trauma (blunt/penetrating) | 2.75 | 4.5 | 2.69 | 4.56 |
| Performing chest wall thoracostomy | 3 | 4.25 | 2.56 | 4.44 |
| Performing clamshell thoracotomy | 2.13 | x | 2.19 | 4.38 |
| Performing pericardiotomy | 2.13 | 4 | 1.94 | 4.25 |
| Performing internal cardiac massage | 2.88 | 4.13 | 2.38 | 4.43 |
| Dealing with underlying heart/vascular injury | 2.38 | 4.13 | 1.88 | 4.06 |
| Performing internal defibrillation | 2.88 | 4.13 | 2.06 | 4.31 |
| Ability to team lead | 2.69 | 4.25 | ||
| Act as a resource coordinator | 2.31 | 4.38 | ||
| Ability to work in a team to expedite the time-critical transfer of an unstable patient | 3.5 | 4.6 | ||
| Ability to work collaboratively to facilitate opening a chest within 5 minutes of an arrest | 3.19 | 4.75 | ||
Jaime Riley 1, Renee Gordon 1
[1]
Across the globe, healthcare systems are experiencing rapid transformation, driven by advances in technology, increasing patient acuity, and evolving professional standards [1]. These shifts have elevated the expectations placed on newly graduated nurses, particularly in their ability to demonstrate critical thinking and clinical judgment. This shift has highlighted the need for innovation in clinical education. Recognizing these challenges, a Faculty of Nursing in Canada saw the opportunity to fundamentally reimagine its approach to clinical education through the intentional development and implementation of an innovative simulation program. The goal was to transition from sparse, ad hoc use of simulation to the comprehensive use of high-quality multimodal simulation to promote clinical judgment and critical thinking.
A simulation program was developed and integrated across the undergraduate nursing curriculum. The program incorporates three simulation modalities: in-person simulation, immersive virtual reality simulation, and screen-based virtual simulation. Informed by the International Nursing Association for Clinical Simulation and Learning’s Healthcare Standards of Best Practice [2], the design is grounded in progressive complexity, aiming to create coherent and scaffolded learning experiences. The faculty engaged in detailed curriculum planning to support the development of consistent simulation experiences throughout all program years. Collaboration and iterative feedback informed implementation.
The completed program provides students with over 100 simulation experiences throughout the undergraduate curriculum. These simulations expose learners to diverse clinical contexts mirroring global health priorities and challenges. The program’s standardized design has fostered faculty development and enhanced alignment across courses, promoting a more cohesive and integrated clinical curriculum.
This initiative offers a replicable model for institutions seeking to modernize nursing education and better prepare students for the complexities of contemporary healthcare. The deliberate integration of multimodal simulation into the undergraduate nursing curriculum has transformed clinical education at this institution.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable
1. Gordon R, Riley J, Dupont D, Rogers B, Witherspoon R, Day K, Horsley E, Killam L. Facilitator development for pre-registration health professions simulation: A scoping review protocol. JBI Evid Synth. 2025;23(4):812–21. doi: 10.11124/JBIES-24-00130.
2. Watts PI, Rossler K, Bowler F, Miller C, Charnetski M, Decker S, Molloy M, Persico L, McMahon E, McDermott D, Hallmark B. Onward and Upward: Introducing the Healthcare Simulation Standards of Best Practice. Clin Sim Nurs. 2021;58:1–4. doi: 10.1016/j.ecns.2021.08.006.
Alice Epps 1, Hajnalka Huszka, Elias Badin
[1]
Ultrasound-guided cannulation shown to be safer and more efficient than landmark-guided cannulation [1]. But it is a skill many resident doctors lack confidence in. We developed an ultrasound-guided cannulation course which aimed to give healthcare workers an opportunity to learn this skill in a safe simulated environment. We evaluated its impact on confidence ratings immediately and 3 months after the course.
Following a needs assessment, a 3-hour course was developed. The course had 3 small group stations: tips and tricks to learn one handed cannulation; basics of ultrasound to understand how to identify peripheral veins on an ultrasound image; followed by an ultrasound guided cannulation station. Candidates had the opportunity to practice on either ADAMgel or commercially available phantoms/models. The course was open to all doctors and allied healthcare professionals in the trust. In total 93 candidates were trained between August 2023 and August 2024.
Confidence in ultrasound guided cannulation was assessed with 7 point Likert scales as part of the needs assessment, immediately after the training sessions and 3 months after the courses.
Data was analysed using Dwass-Steel-Critchlow-Flinger pairwise comparison tests with Jamovi software.
There were 112 responses to the initial questionnaire, 88 to the post-course and 36 for the 3-month questionnaire. Mean confidence in ultrasound guided IV access was 2.70 (SD 1.795) initially. This increased to 5.75 (SD 0.913) following the course and decreased to 5.08 (SD 1.180) at the 3-month time point. Dwass-Steel-Critchlow-Flinger pairwise comparison showed statistically significant increase in confidence rating between the initial questionnaire and both the post-course and 3-month time point. There was a decrease in confidence rating between the initial post-course and 3-month point but this was not statistically significant.
In a large cohort of healthcare professionals, we have shown a significant improvement in confidence in ultrasound-guided cannulation following attending ourcourse. This supports wider roll out of such courses to empower practitioners to confidently gain peripheral IV access using ultrasound guidance. From anecdotal evidence we believe this potentially has reduced referrals to anaesthetics for difficult cannulations in our trust. We aim to quantify this more objectively over the coming months.
The observed decrease in confidence 3 months after the course suggests a booster course may help to refresh skills. Given confidence was still greater than at baseline, this may only need to be a single station to practise the procedure.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable
1. García-Carpintero E, Naredo E, Vélez-Vélez E, Fuensalida G, Ortiz-Miluy G, Gómez-Moreno C. Phantoms for ultrasound-guided vascular access cannulation training: a narrative review. Med Ultrason. 2023;25(2):201–207. doi: 10.11152/mu-3711.
We would like to thank all the faculty members who helped deliver the course.
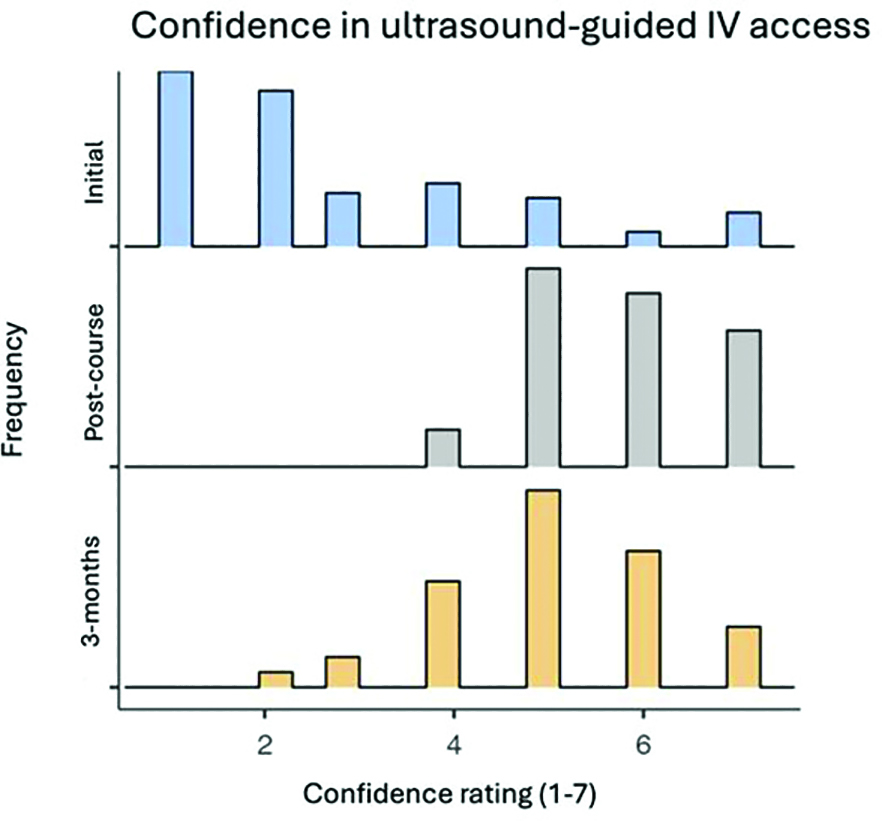
Rehana Dyson 1, Hannah Downing 1, Frankie Bevis 1, Vicki Currie 1
[1]
Birmingham Children’s Hospital (BCH) Emergency Department (ED) serves as the paediatric major trauma centre (MTC) for the West Midlands and Central England, managing the region’s most severely injured children. Due to the high acuity but low frequency of such cases, clinician experience and confidence are often limited [1].
This project aimed to design and implement a paediatric trauma simulation curriculum and assess whether this intervention can strengthen clinical skills, improve teamwork, promote adherence to guidelines, and improve clinician confidence [1,2].
A paediatric trauma simulation curriculum was designed collaboratively by education fellows and emergency medicine clinicians at BCH ED. The curriculum integrated evidence-based guidelines and included a variety of paediatric trauma scenarios, such as haemorrhage control, penetrating and blunt trauma, and resuscitation. The simulation curriculum was designed using the principles of a spiral curriculum, allowing clinicians to revisit core concepts at increasing levels of complexity over time with simulation repetition [3].
High-fidelity multidisciplinary simulations were conducted approximately bi-weekly over six months. Each session included a pre-simulation briefing, in-situ simulation, and debriefing focused on technical and non-technical skills.
Structured surveys collected feedback on simulation relevance, usefulness, and self-reported confidence. Based on participant feedback and faculty reflection, the curriculum was continuously refined to meet evolving learning needs.
Over seven months, 73 participants—including students, nursing staff, advanced nurse practitioners, and doctors of varying seniority—participated in the programme.
Key findings include:
92% of participants agreed or strongly agreed that the simulations were useful and relevant.
96% agreed or strongly agreed that the sessions were interactive.
93% reported improved confidence in managing paediatric trauma cases, with an average increase of 29% in self-reported confidence. Participants with initially lower confidence levels experienced a higher-than-average confidence boost of 37%.
However, 8% of participants felt their understanding of underlying theory and principles did not improve, indicating areas for further curriculum development.
This structured simulation curriculum significantly enhanced participants’ confidence and competence in paediatric trauma management, particularly among those with initially lower confidence. These results suggest regular, in situ high-fidelity simulation training effectively addresses knowledge gaps and enhances clinical and non-technical skills.
As informed by participant feedback, future curriculum modification will focus on strengthening theoretical components and providing post-simulation resources to consolidate learning.
Overall, this programme reinforces the critical role of simulation in preparing ED teams for the high acuity but low occurrence of paediatric polytrauma care.
1. Jensen AR, McLaughlin C, Wong CF, McAuliff K, Nathens AB, Barin E, Meeker D, Ford HR, Burd RS, Upperman JS. Simulation-based training for trauma resuscitation among ACS TQIP-Pediatric centers: Am J Surg. 2019 Jan;217(1):180–185. doi: 10.1016/j.amjsurg.2018.06.009. Epub 2018 Jun 18. PMID: 29934123; PMCID: PMC7169990.
2. Harden RM. What is a spiral curriculum? Med Teach. 1999;21(2):141–3. doi: 10.1080/01421599979752. PMID: 21275727.
3. Thim S, Henriksen TB, Laursen H, Schram AL, Paltved C, Lindhard MS. Simulation-Based Emergency Team Training in Pediatrics: A Systematic Review. Pediatrics. 2022 Apr 1;149(4):e2021054305. doi: 10.1542/peds.2021-054305. PMID: 35237809.
This project was supported by internal departmental funding from the Birmingham Children’s Hospital Emergency Department.
Serena Merchant 1, Sneha Gupta 1, Peter Springbett 1
[1]
Final-year medical students often report feeling unprepared for managing the responsibilities of on-call shifts as foundation doctors, particularly in prioritisation, escalation, communication, and prescribing tasks [1]. Responding to bleeps has been identified as a particularly anxiety-inducing element of starting clinical practice [2]. Addressing this gap in preparedness is crucial for ensuring a safer transition to postgraduate training. The Virtual On-Call (VOC) simulation was developed to provide a realistic, low-fidelity, psychologically safe environment for final-year students to practice core on-call competencies. We aimed to evaluate whether participation in VOC improved students’ self-reported confidence across key clinical domains and to explore student perceptions of the simulation’s realism and educational value.
We implemented a low-fidelity simulation across two hospital sites (Maidstone and Tunbridge Wells) between early 2024 and 2025. Groups of 3–4 students carried simulated bleeps and responded to a series of ward-based on-call tasks, such as fluid prescribing, patient reviews, and escalating deteriorations using SBAR. Tasks were accessed from designated ward envelopes, with no live patient interaction. Each session lasted one hour, followed by structured group debriefs. Six sessions were delivered. Students completed pre- and post-session surveys measuring confidence across six domains (prioritisation, prescribing, answering bleeps, note-taking, handover, and escalation) on a 5-point Likert scale. Free-text responses were collected to explore qualitative experiences. Descriptive analysis was performed.
Of the 27 students completing pre-session surveys, 20 completed post-session surveys (completion rate: 74%). Confidence improved across all domains. The greatest improvement was seen in answering bleeps, with the mean confidence score increasing from 1.8 to 3.8. Initially, 85% of students rated their confidence as low (scores 1–2), compared to 75% rating it as moderate-to-high (scores 3–4) post-session. Qualitative analysis identified themes of increased confidence, appreciation of the session’s realism, and the importance of practicing teamwork and escalation pathways.
Participation in the VOC simulation significantly improved final-year students’ self-reported confidence, especially in managing bleeps and prioritising tasks. Students valued the realism, safe environment, and practical application of multiple skills simultaneously. Our findings suggest that low-fidelity, accessible simulations can effectively enhance undergraduate preparedness for clinical practice, supporting previous literature on simulation-based learning [3].
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Illing J, Morrow G, Kergon C, et al. How prepared are medical graduates to begin practice? Final report. Newcastle: General Medical Council; 2008.
2. Monrouxe LV, Grundy L, Mann M, et al. How prepared are UK medical graduates for practice? Med Teach. 2017;39(1):38–43.
3. Motola I, Devine LA, Chung HS, et al. Simulation in healthcare education: a best evidence practical guide. Med Teach. 2013;35(10):e1511–30.
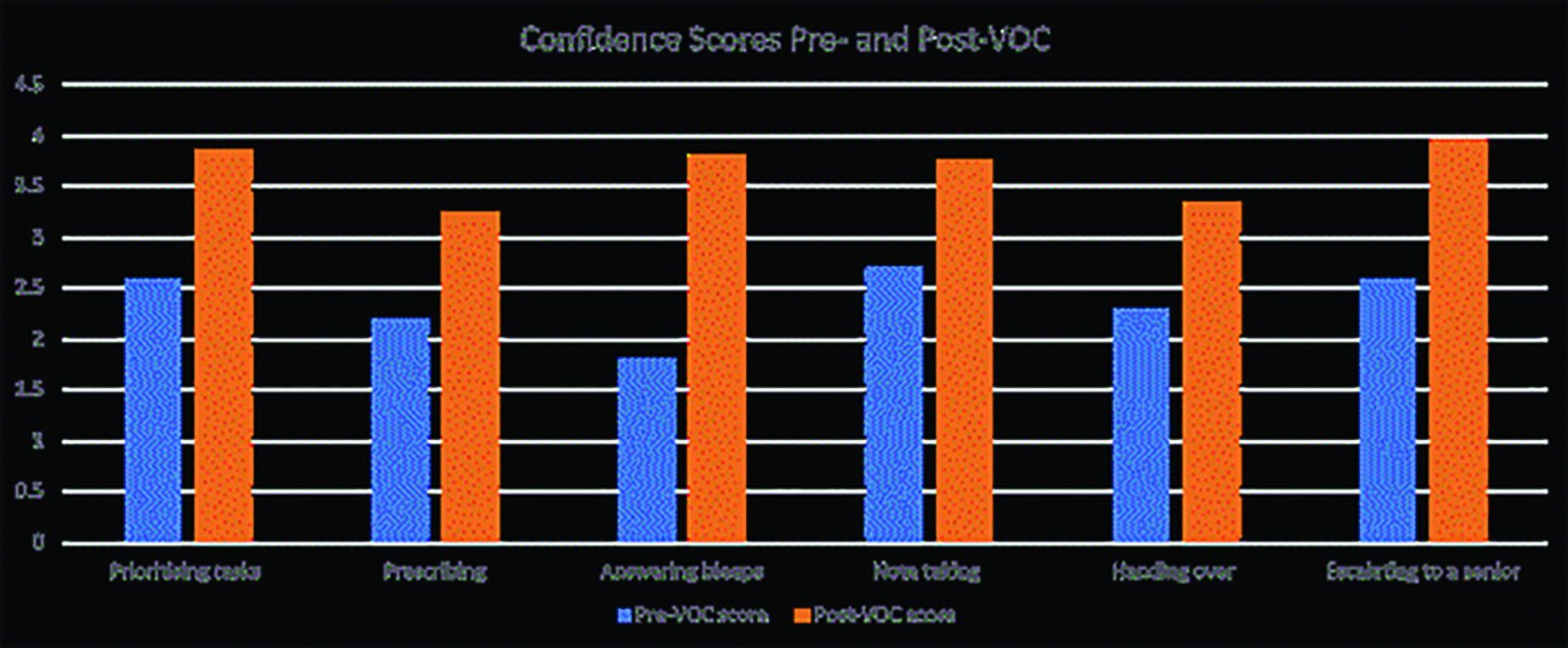
Rosie Byars 1, Jane Roome, Krishan Banot, Connor Thompson-Poole, Fernando Perez, Danny Bartlett, Jackie Knight
[1]
[2]
Recent reforms in undergraduate pharmacy education [1] mandate increased clinical exposure in primary care to support the development of prescribing competencies and consultation skills. However, capacity constraints in community care, driven by workforce shortages and service pressures challenge traditional placement models [2]. Observed simulation-based education offers a scalable and innovative solution. This pilot project explored the design and implementation of a virtual clinical experience (VCE) for third-year pharmacy students, using simulation to deliver standardised, high-fidelity, experiential learning. The aim was to implement and evaluate a hybrid simulation model that addresses placement shortages, reduces clinician burden, enhances student engagement, and supports interprofessional education.
Seventy-four third-year pharmacy students from the University of Brighton participated in a pilot VCE day comprising simulated GP consultations delivered via livestream. The day was structured into:
Prebriefing with defined learning outcomes
Live observation of two distinct GP-patient consultations with simulated patients
Facilitated debriefing sessions utilising experiential and social learning theories.
Half way through the day students were divided into subgroups with assigned observer roles focusing on clinical, communication, and patient-centred care dimensions. Supplementary workshops and a digital health session introduced prescribing workflows and electronic health records.
The simulation design was informed by Kolb’s Experiential Learning Cycle and Bandura’s Social Learning Theory, promoting active observational learning. With the midway changes, debriefing was adapted to deepen engagement. Directed observer roles transformed passive observation into purposeful participation, fostering critical thinking, reflective practice, and peer discussion [3].
84% of students reported increased confidence in consultation skills and rated 4.5/5 for enjoyment; Qualitative feedback highlighted the value of real-time observation and communication strategies. Educators rated the day 4.8/5; 100% agreed objectives were met. Identified challenges included time management and AV logistics; key improvements suggested included extended debriefs and clearer observer instructions from the start.
VCE provides a scalable, immersive solution for clinical learning in pharmacy education, addressing placement limitations while supporting high-quality, standardised experiences. The model’s success supports future iterations incorporating longitudinal simulated patient journeys to encompass the continuity of patient care in primary care. Expansion to other institutions and disciplines is feasible, promoting sustainability, and collaboration in simulation-based learning.
Future evaluations will explore the integration of learner-designed cases and interprofessional simulations across multiple institutions. This will assess long-term retention of consultation skills and model scalability, contributing to national pharmacy education reform.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable
1. General Pharmaceutical Council. Standards for the initial education and training of pharmacists [Internet]. London: General Pharmaceutical Council; 2021 Jan [cited 2025 Apr 20]. Available from: https://assets.pharmacyregulation.org/files/2024-01/Standards%20for%20the%20initial%20education%20and%20training%20of%20pharmacists%20January%202021%20final%20v1.4.pdf
2. Elley CR, Clinick T, Wong C, et al. Effectiveness of simulated clinical teaching in general practice: randomised controlled trial. Journal of Primary Health Care. 2012;4(4):281–7.
3. Bethards ML. Applying Social Learning Theory to the Observer Role in Simulation. Clinical Simulation in Nursing. 2014;10(2):e65-e69
Zainab Zahran 1, Aby Mitchell 1, John Brooks 1, Leanne Dolman 1, Victoria Clemett 1
[1]
Peer Evaluated Simulation (PES), embedded in a final-year undergraduate nursing module, enables students to enact clinical scenarios and receive formative feedback from peers. In simulation-based learning, peer evaluation can be a powerful formative assessment tool. Creating a rubric for peer evaluation in simulation is a structured approach that provides students with clear guidelines and criteria to assess their peers’ performance accurately and constructively [1,2]. A well-designed rubric standardises feedback, reduces subjective bias, and encourages reflective practice. The key concepts within this PES are related to Shared Decision Making (SDM), which is a neglected component of existing simulation rubrics. Therefore, this study outlines how these components are conceptualised and developed into the rubric to enable students to critically analyse each other’s performance in a constructive, respectful manner.
A co-design educational approach, underpinned by a descriptive qualitative design was adopted. Three one- hour focus groups were conducted with final year nursing students, and standardised patients at a large UK university from February to June 2024 to iteratively co-design the content and implementation of the rubric. Focus groups were held over the MS-Teams platform and recorded. Thematic analysis was used to identify key aspects of SDM that informed and refined the rubric and its integration into a pre-registration nursing course. The study was guided by established programme theory on shared decision making [3].
Several recurring themes emerged that informed the creation of the rubric: (1) patient-centred care and engagement; (2) communication skills; (3) team dynamics and interprofessional collaboration; (4) cultural competence and self-awareness; and (5) openness to learning. The co-development of this rubric ensured content validity for peer evaluators to rate and provide feedback on student’s shared decision-making behaviour in the simulation setting. Students positively evaluated the rubric’s clarity and relevance but highlighted the need for improved usability, clearer descriptors, and scenario specific alignment.
Findings demonstrate the feasibility and value of co-designing a SDM focused rubric for use in simulation-based nurse education. Involving students and patients in the design ensured alignment with authentic clinical experiences. Early introduction of the rubric into the curriculum, along with structured opportunities to practice giving feedback, were identified as essential. The rubric shows promise for supporting formative assessment and developing reflective practitioners. Future research should examine its reliability, potential for adaptation across settings, and integration into summative assessment strategies.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Lertsakulbunlue S, Kantiwong N. Development of a peer-assessment rubric for nursing students in simulation-based learning. Journal of Nursing Education and Practice. 2024;14(2):10–16. doi: 10.1186/s41077-024-00301-7.
2. Panadero E, Jonsson A. The use of scoring rubrics for formative assessment purposes revisited: A review. Educational Research Review. 2013; 9:129–144. doi: 10.1016/j.edurev.2013.01.002.
3. Waldron T, Carr T, McMullen L, Westhorp G, Duncan V, Neufeld SM, Bandura LA, Groot G. Development of a program theory for shared decision-making: a realist synthesis. BMC health services research. 2020 Dec; 20:1–7. doi: 10.1186/s12913-019-4649-1.
Funding: Florence Nightingale Faculty of Nursing, Midwifery & Palliative Care SeedCorn funding.
Acknowledgments: We wish to thank all the participants in our study.
Rowena Rickson 1, Karina Catley 1, Diane Laverty 1, Jodie Grace 1, Natalie Nabunya 1, James Roberts 1
[1]
Ambulance services are seeing an increase in PEoLC patients electing to remain at home, with a focus on supportive care [1]. A challenge exists in how to suitably equip and empower ambulance services to adapt their culture, shifting from survival focussed care to supportive care for this patient group. Addressing this need through the implementation and development of simulation workshops, which are proven to be effective [2], aims to explore the impact on clinicians and consider the potential for further programme development.
Simulation workshops with professional actors were facilitated by the service’s PEoLC team in partnership with Advanced Paramedic Practitioners in Urgent Care (APP-UC). The programme was developed over a two-year period; feedback and reflections on year 1 informed the design of year 2. Scenarios each year were designed based on current themes in local clinical practice including recent incidents. A total of 66 clinicians participated (42 in 2023 and 24 in 2024). They were asked to complete a contemporaneous and retrospective survey. Questions explored confidence and learner perceptions around how the course design and delivery influenced their educational experience.
Of 66 participants across two cohorts, contemporaneous survey results were gathered from 91%. Of the 42 participants in 2023 only 24% responded to the retrospective survey, of 24 participants in 2024 only 17% responded. This low response level is a limitation, alongside the subjective nature of recollections of educational experiences. Results demonstrate high levels of confidence sustained into practice across both participant groups (Figure 1).
The majority of participants (89% in 2023; 96% in 2024) felt that the simulation design, particularly the use of actors, contributed to the realism of scenarios.
Smaller groups were identified as an element influencing comfort when participating in simulation, with a 20% increase in participant comfort where this was implemented in 2024.
A high level of comfort participating in debriefs (86% in 2023; 96% in 2024) was reflected through the main theme of fostering a safe learning environment through a non-judgemental, non-assessment focussed approach. This seeks to transform education delivery beyond the current testing and assessment based approach [3].
Emergent themes from surveys and the delivery teams own reflections highlight the effectiveness of simulation in PEoLC education evidencing high levels of confidence, allowing clinicians to practice important and underutilised skills in a psychologically safe environment. Further development of the design and delivery, driven by feedback will allow for improved educational experiences.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Johansson T, Pask S, Goodrich J, Budd L, Okamoto I, Kumar R, et al. (Time to care: Findings from a nationally representative survey of experiences at the end of life in England and Wales. Research report. London (UK): Marie Curie. (September 2024). Available from: www.mariecurie.org.uk/policy/better-end-life-report
2. Elendu C, Amaechi DC, Okatta AU, Amaechi EC, Elendu TC, Ezeh CP, et al. The Impact of simulation-based Training in Medical education: a Review. Medicine [Internet]. 2024;103(27):1–14. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC11224887/
3. Abelsson A, Rystedt I, Suserud BO, Lindwall L. Learning by simulation in prehospital emergency care - an integrative literature review. Scandinavian Journal of Caring Sciences [Internet]. 2015 Aug 29;30(2):234–40. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1111/scs.12252

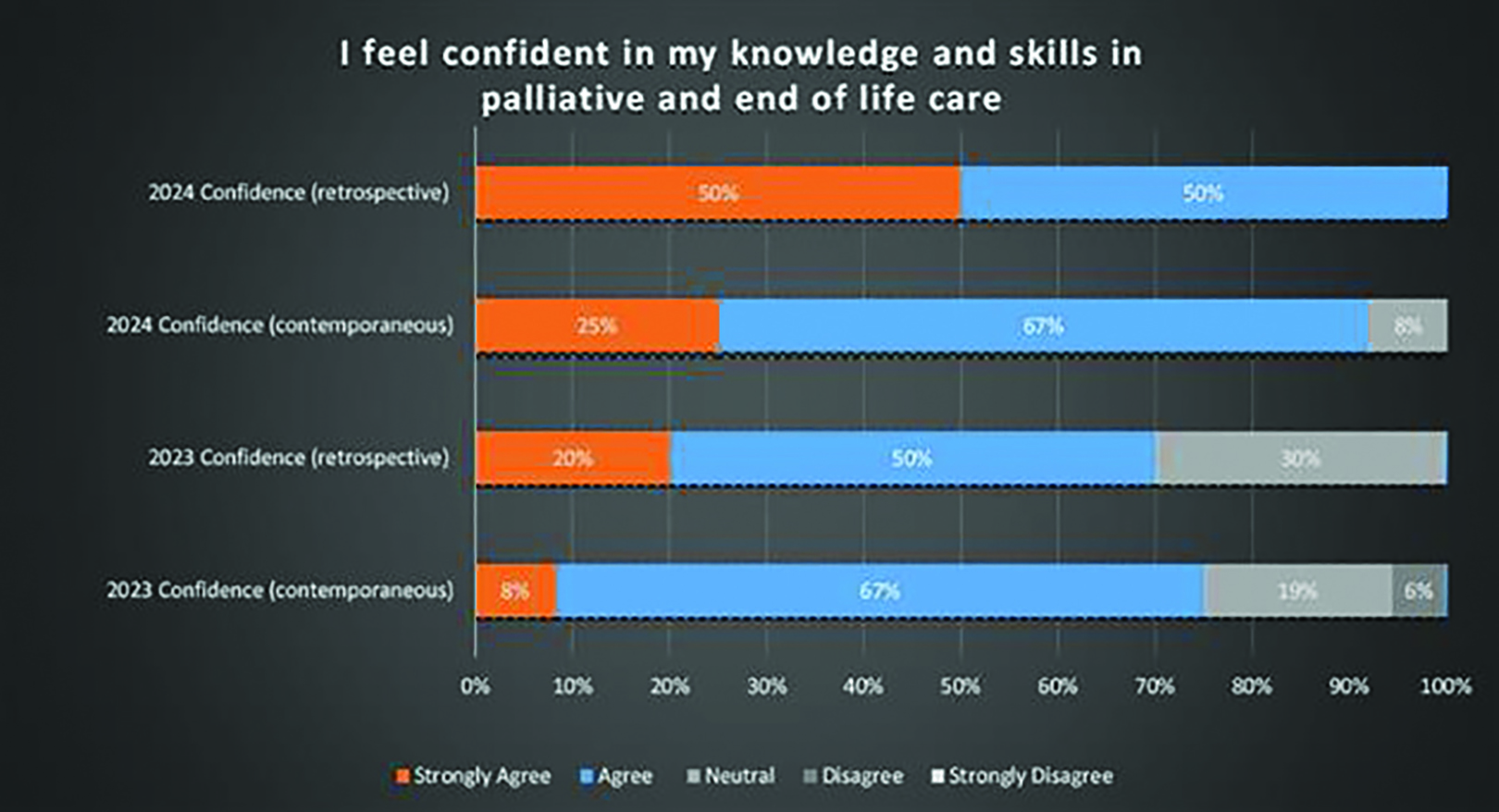
Emma Sang 1, Polly Clarke 1, April Glory 1, Helen Jarvis 1, Meril Labarge 1
[1]
This initiative aims to address the critical training gap in paediatric mental health services by implementing simulation-based education (SBE), with a focus on equipping healthcare professionals to respond effectively to mental and physical health emergencies. Simulation-based education is well-established in acute and physical healthcare settings but remains underutilised in mental health services, particularly in paediatrics [1]. This gap persists despite evidence that simulation can enhance clinical confidence, interprofessional collaboration, and patient safety [2]. Within the new Simulation Strategy launched at BWCFT, the recognition of the need for both physical and mental health simulation support was paramount. The goal was also to begin growing expert faculty trained to deliver simulation-based education within our mental health setting.
A series of immersive simulations were conducted within our inpatient unit, combining physical and mental health scenarios such as respiratory/cardiac arrest following ligature incidents and severe hypoglycemic patients with eating disorders, alongside post-incident risk assessment. Sessions were delivered in-situ, with a flexible approach to environment and staff availability. Multidisciplinary team members, including those less confident in managing physical health emergencies, were actively encouraged to participate.
The simulations facilitated engagement from a broad range of staff, enhancing competencies in airway management, A–E assessment, advanced life support (ALS), escalation protocols, and secondary assessment. Participant feedback indicated improved confidence in recognising and managing physical deterioration, strengthened interprofessional communication, and a greater sense of preparedness for real-life emergencies. Staff specifically reported “a better understanding of checking for vital signs when completing physical observations and interacting with an unwell young person.” Another participant commented, “I really appreciated the training; it mimicked real scenarios that we encounter, particularly with decision-making under pressure,” highlighting the realism and relevance of the scenarios. The initiative also fostered a culture of continuous learning and collaboration within each ward, as this was completed through a multi-agency approach. The need for regular simulations has now been identified, and the growth of our core expert faculty has greatly supported this delivery.
Integrating simulation into paediatric mental health settings addresses a critical training gap, promoting holistic care that encompasses both mental and physical health emergencies. This approach not only enhances clinical skills but also strengthens team dynamics and patient safety. The success highlights the potential for simulation to drive cultural change and improve outcomes in mental health services. Future directions include expanding the range of scenarios and conducting longitudinal evaluations to assess the impact on clinical practice and patient care.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable
1. Attoe C, Hegarty J, McKenna H, et al. Managing medical emergencies in mental health settings using an interprofessional in-situ simulation training programme: A mixed methods evaluation study. Nurse Educ Today. 2017;59:103–109.
2. Hasson F, McKenna H, Keeney S, et al. Interprofessional simulation training for community mental health teams: Findings from a mixed methods study. J Interprof Care. 2018;32(3):346–353.
Matthew Bowker 1
[1]
Honour-based abuse (HBA) is a form of domestic abuse motivated by perceived ‘dishonour’ to family or community. Often involving multiple perpetrators from family networks, HBA centres around controlling behaviours and beliefs. Healthcare professionals frequently miss identifying victims. Simulation-based education offers an effective training method for sensitive topics but requires careful design to avoid stereotyping cultural contexts [1]. This project aimed to develop authentic simulation scenarios through co-production with survivors.
Five HBA survivors participated in interviews focusing on their disclosure experiences with healthcare professionals. These interviews informed two simulation scenarios for final-year medical students. The initial scenario addressed HBA within a South Asian Muslim context. When role-play providers lacked staff from appropriate cultural backgrounds, a second version was created focusing on universal aspects of abuse disclosure, with honour dynamics addressed in debriefing. Both scenarios incorporated survivor quotations and emotional insights. Survivor narratives provided authentic language that enriched scenario scripts with direct quotes about disclosure barriers, shame, and familial pressure. The second scenario was delivered to 39 UK medical students, emphasising recognition of disclosure cues, sensitive communication, safety planning, and referral pathways. All students received an email notification of the content a week prior to the simulation, in addition to usual prebriefing and debriefing.
Feedback from 16 participants using a 5-point Likert scale showed high ratings for usefulness (4.94/5), understanding (4.94/5), confidence (4.81/5), relevance (4.94/5), and potential to change practice (4.88/5). Qualitative feedback highlighted increased awareness of disclosure opportunities and improved confidence. One student noted: “I learned about patients giving ‘crumbs’ of details as an opportunity to open up or gauge if they can trust the healthcare professional”. Students valued the survivor-informed approach, with feedback highlighting how authentic scenarios prepared them to “ask the difficult questions.”
Co-production created authentic scenarios but revealed issues regarding diverse representation among simulated participants (SPs). The lack of SPs from South Asian Muslim backgrounds necessitated adapting the simulation, raising questions about authenticity in cultural representation. Despite these challenges, survivor-informed content remained powerful, with verbatim quotes providing authenticity that resonated with students. The adaptation process demonstrated the value of teaching universal disclosure principles when facing representational constraints. This experience underscores the need for greater diversity within SP pools while highlighting how co-production with survivors can promote cultural humility [2] and meaningfully represent lived experiences.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Vora S, Dahlen B, Adler M, et al. Recommendations and Guidelines for the Use of Simulation to Address Structural Racism and Implicit Bias. Simul Healthc J Soc Simul Healthc. 2021;16(4):275–284.
2. Foronda C, Prather S, Baptiste DL, Luctkar-Flude M. Cultural Humility Toolkit. Nurse Educ. 2022;47(5):267–271.
Rebecca Akehurst 1, Emma Lillie, Mia King, Emma Tagliavini, Megan Martin-Wharfe, Karen Bradley, Charlotte Harper
[1]
Effective management of critically unwell children demands seamless interprofessional collaboration, rapid clinical decision-making, and a high degree of confidence among healthcare providers. However, many professionals across disciplines report low self-efficacy in paediatric emergencies, due to limited exposure and lack of interprofessional training opportunities outside paediatric tertiary centres [1].
This abstract outlines the development, facilitation, and outcomes of a targeted interprofessional simulation-based education (IPSE) course. Designed to enhance confidence and competence in managing acutely unwell paediatric patients, the course, delivered over one day and attended by a range of candidates from differing disciplines across the trust including Nurses, Critical Care Doctors, Emergency Doctors, Anaesthetist and Operating Department Practitioners. The course was designed using a learner-centred approach blending different strategies of teaching to encourage interaction and engagement among the candidates. The learning objectives were informed by current paediatric emergency guidelines, institutional training needs, and participant feedback from previous sessions. The course combined skills stations prior to facilitating three high-fidelity simulation scenarios, with structured debriefing and reflective practice discussions. Scenarios included paediatric sepsis, status epilepticus and infant respiratory failure. Facilitators, emphasised teamwork, communication, clinical skills and clinical decision-making under pressure.
Pre- and post-course surveys assessed participant confidence, while qualitative feedback captured candidates’ attitudes to the importance of IPSE. Results showed a statistically significant improvement in self-reported confidence across all professional groups.
The candidates highlighted the value of learning alongside other disciplines, noting improved understanding of each other’s roles and enhanced trust in collaborative care delivery. Key challenges in course facilitation included coordinating multi-disciplinary attendance and ensuring equitable engagement across roles during scenarios. These were addressed through role modelling of the inter-professional faculty, careful scenario design and use of inclusive language. This course demonstrates that well-structured interprofessional simulation can significantly enhance healthcare professionals’ confidence in managing the care of the critically unwell child. We advocate for the integration of IPSE into routine paediatric emergency training curricula to foster confident, collaborative, and competent healthcare teams.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. World Health Organization. Framework for action on interprofessional education and collaborative practice. Geneva: World Health Organization; 2010.
Sue Baron 1, Angela Paget 1, Emma Greenwood 1, David Biggins 1, Jakob Rossner 1
[1]
Empathy enhances healthcare professionals’ understanding of the experiences, perspectives, needs and feelings of patients and colleagues [1]. It is fundamental to professionalism, therapeutic relationships and person-centred care. Empathy improves patient wellbeing, satisfaction and clinical outcomes [1] and reduces the risk of healthcare staff experiencing stress and burn-out. Importantly, empathy is an antecedent to cultural competence and enables caregivers to respond appropriately, and without prejudice to the needs and expectations of patients and colleagues, several of whom will come from diverse backgrounds and/or vulnerable and groups. Approximately 15% of patients admitted to hospital have a communication disability that affects their ability to speak with and/or understand the staff who care for them [2].
A review of 27 studies identified that ‘…vulnerable patients with communication disabilities (i.e. impairments of body structure or function that impact upon speech, language, or communication function) face a three-fold increased risk of sustaining preventable and harmful patient safety incidents’ [2, p502]. Some of the most commonly reported factors include i) ‘being in hospital with no way to gain the attention of or communicate with hospital staff’; ii) ‘…staff who are not always attentive even when patients raised the alarm’; iii) ‘advocacy failure’; and iv) ‘failing to listen, or to recognise complaints of pain or symptoms of distress’ [2, p509].
A collaborative approach to co-production of digital educational resources (videos and e-simulation) involving people with first-hand experience that aimed to:
DRAW ATTENTION to the risks faced by people with a communication disability when accessing healthcare
RAISE AWARENESS of nurses’ and healthcare workers’ legal and professional duty to identify, record and act on every patient’s communication needs
PROMOTE EMPATHY as a vital component of professionalism, and a skill and competency that can be learned by healthcare staff through education and practice
DEVELOP an educational resource that could be readily accessed and used in healthcare education and practice
Since production, Helen’s story videos and Empathic Care of a Person with Cerebral Palsy: E-Simulation Toolkit have been embedded in pre-registration nursing curricula, shared with other health professional programmes, and the University of Technology, Sydney, Australia in the Virtual Empathy Museum’s Simulation Room. Student evaluations have shown these resources help to raise awareness, address stereotypical and judgemental views, enhance empathy, and strengthen vital knowledge and understanding that enables the delivery of safe, person-centred practice for people who have a disability and complex communication needs.
Co-produced digital resources offer powerful, practice-based tools for empathy education. Lived experience enhances authenticity and challenges bias in healthcare learning. Students report improved understanding of empathy, communication needs and person-centred care. Resources support critical reflection on practice, helping learners avoid blame and explore influencing factors. Their integration into curricula and global platforms highlights broad educational impact.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Petrucci C, La Cerra C, Aloisio F, et al. Empathy in health professional students: A comparative cross-sectional study. Nurse Education Today. 2016;41:1–5.
2. Hemsley B, Georgiou A, Hill S, Rollo M, Steel J, Balandin S. An integrative review of patient safety in studies on the care and safety of patients with communication disabilities in hospital. Patient Education and Counseling. 2016;99:501–511.
The authors gratefully acknowledge Helen Ross for her lasting legacy to healthcare education. Helen sadly passed away in 2018. We also thank Professor Tracey Levett-Jones (University of Technology Sydney) for her support and inclusion of this work in the Virtual Empathy Museum. Further thanks to Fabi Duprés, John Moran and Keith Pretty (Bournemouth University) for their contributions to video production and project support.
Resident doctors are expected to have the knowledge and skills required to manage common medical emergencies. Medical students report anxiety and under-preparedness for such situations [1]. There is a lack of understanding as to why this is and how students could be better prepared for this transition. This study aims to evaluate the educational impact of a simulation-based educational curriculum in a novel cohort of medical students from multiple year groups and two universities.
Sessions were offered weekly for 30 months (over 120 sessions) in a non-clinical teaching space and included the management of curriculum-based emergency presentations. Each session involved initial pre-teaching simulated scenario(s), followed by a teaching session (a blended approach with workshops, quizzes, didactic teaching and small group working) and concluded with further simulated scenarios to consolidate the learning. Specific skills training was embedded throughout (e.g., interpretation of ECGs, X-rays, lab results and prescribing). These sessions were open to all students on placement in Causeway Hospital (a rural District General Hospital) and included students from Queens University Belfast and Ulster University. Sessions were evaluated in a voluntary, anonymised, online post-course questionnaire.
An average of sixteen students (8–24) attended each week with a 75% feedback response rate. Data was collected on over 3600 individual simulation encounters. Students consistently reported increased confidence in the assessment, recognition and management of unwell patients. Students particularly enjoyed the opportunity for ‘hands-on’ skills acquisition reporting that this helped to contextualise their learning and addressed potential gaps in their knowledge base. The blended approach to teaching using simulated scenarios at the beginning and end of sessions was rated extremely highly as students felt they left the sessions having consolidated their learning. Students felt the scenarios were highly realistic and could see the relevance to their imminent role as a resident doctor. Students spoke positively of the psychological safety created in the sessions and this was attributed at least in part to the consistency of faculty members skilled in simulation-based education. Students also viewed the opportunity to engage in simulated scenarios with students from other year groups and university positively as they felt this reflects the ‘real world’ where teams are made up of individuals with different skills and knowledge bases.
This program provides a safe, highly-valued educational experience for participants and has been highlighted amongst the student body as being an example of excellence in simulation-based education in the Northern Ireland.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Monrouxe L, Grundy L, Mann M, John Z, Panagoulas E, Bullock A, et al. How prepared are UK medical graduates for practice? A rapid review of the literature 2009–2014. BMJ Open. 2017;7:e013656. doi: 10.1136/bmjopen-2016-013656.
Carrie Hamilton 1, Victoria Aldridge 2, Paula Dawson 2, Zoe Broughton 2, Caroline Tomkins 1, Kirsten Howson 1, Nichola Martin 1
[1]
[2]
Effective communication remains a cornerstone of compassionate healthcare, closely linked to patient experience and care outcomes [1]. In 2022, the Comprehensive Communication Skills Training (CCST) course was developed at a medium-sized trust, in response to feedback from bereaved families and frontline staff, aiming to improve communication in emotionally complex scenarios [2]. Preceding the creation of the course, the facilitators attended a two-day training in experiential learning. Since its inception, the course has been refined; a Patient Advice and Liaison Service (PALS) component, produced through a listen-create-reconnect exercise with relatives with lived experience, has been added. This development helps attendees understand how to respond to complaints in the moment and highlights the function of PALS as a key support service for patients and families.
The training uses immersive simulation, with actor role players enacting authentic patient and family encounters. This encourages deep emotional engagement and reflection. Participants follow the journey of an elderly inpatient, and his wife, encountering pivotal communication challenges during his final hospital stay.
The effectiveness of this training is credited with the collaboration; scenarios and debrief content, which are shaped by the real stories of patients and bereaved relatives, whose voices are woven throughout the training. This ensures the course content remains both emotionally resonant and grounded in lived experience, a hallmark of meaningful communication education [3].
Approximately 300 trust staff have participated, all describe an increased confidence in managing difficult conversations. The newly introduced PALS module has been a welcome addition with participants reporting a better understanding of the role of PALS in supporting patients. Participants have highlighted the value of the emotional realism, the protected space for self-reflection, and the power of hearing service user stories in their own words.
In 2023/2024 poor communication was indicated as the primary theme in 100% of the complaints made in relation to end of life care. Current complaints data for the trust shows a significant reduction related to this theme, attributable to just 22% (1 April 2024 – 31 December 2024).
By blending experiential learning with patient-informed narrative and structured reflection, participants reconsider how they listen, respond, and empathise. CCST builds confidence, strengthening trust between staff and patients and attendees feel directly connected to the experiences. The simulation-based transformative I’s [4], involvement, inclusion and influence underpin this programme. CCST’s growing reputation is leading to the embedding of the training in multi-professional induction and continuing education.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Wilkinson S, Perry R, Blanchard K, Linsell L. Effectiveness of a three-day communication skills course in changing nurses’ communication skills with cancer/palliative care patients: a randomised controlled trial. Palliative Medicine. 2008;22(4):365–375.
2. MacLean H. Comprehensive Communication Skills Training (CCST) for Ward Staff. International Journal of Healthcare Simulation. 2022;2(Suppl 1):A67.
3. Gilligan T, Coyle N, Frankel RM, Berry DL, Bohlke K, Epstein RM, Baile WF. Patient-clinician communication: American Society of Clinical Oncology consensus guideline. Journal of Clinical Oncology. 2017;35(31):3618–3632.
4. Weldon SM, Buttery A, Spearpoint K, Kneebone R. Transformative forms of simulation in health care – the seven simulation-based ‘I’ s: a concept taxonomy review of the literature. International Journal of Healthcare Simulation. 2023.
Jonathan Davies 1, Wright Sally 1, Alison Devine 1, Alice McCloskey 1, Ali Walker 1
[1]
Identification and prevention of cardiovascular disease (CVD) was identified as the single biggest area where the NHS can save lives in the NHS Long-term plan [1]. The NHS Health Check screening aims to assess a person’s risk of developing CVD, type 2 diabetes and dementia and offer advice to help people maintain or improve their health [2]. Student-led health check clinics have been implemented in other universities, proving to be a viable mechanism to deliver Experiential Learning, while providing health services to an underserved population [3]. A robust training programme was required, ensuring students to develop skills whilst also demonstrating competence to deliver the service.
A bespoke training package was collaboratively designed by practitioners, simulation faculty and practice partners to support skill development and demonstration of competence.
Alongside a programme of traditional teaching (incorporating clinical and consultation skills) and mandatory training, two half-day in-person simulation sessions were used to consolidate learning and allow for exploration of key concepts prior to launch of the service. In the first of these two sessions, an AI-enabled manikin was utilised to allow students a safe opportunity to undertake a full protocol-based CVD screening assessment. In the second session, standardised patient actors were used to provide students an opportunity to combine both clinical and consultation skills.
Following the simulated events, assessment of student competence was conducted. Using standardised patients in a controlled environment, students were tested against a nested Entrustable Professional Activity (EPA), encompassing key components of the health check.
All 153 students passed the competency assessment following the training.
A University-based health check service for staff and students led by pharmacy students under supervision by qualified practitioners was subsequently launched. Student-led CVD screening in the community will commence from the 25–26 academic year, in collaboration with a local primary care network.
Evaluation is ongoing, focussing on student views of the training. Initial responses suggest the simulated placements were well situated in terms of wider taught content and that, following completion of the training programme, students felt able to safely perform an NHS Health Check.
Development and implementation of a comprehensive training package, incorporating traditional and simulated learning methodologies, has successfully facilitated the establishment of a student-led health check service within the University. Student performance and initial student feedback regarding their perceived competence to safely perform the service highlights the effectiveness of this approach in preparing future pharmacists for expanded roles in preventative healthcare.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. NHS. The NHS long term plan. 2019. Available from: https://www.longtermplan.nhs.uk/. Accessed 24 April 2025.
2. Public Health England. NHS Health Check Programme Standards: A framework for Quality Improvement. July 2020. Available from: https://www.healthcheck.nhs.uk/seecmsfile/?id=1507. Accessed 24 April 2025.
3. Maughan E, Richardson C, Nazar H. A cross-sectional investigation of a mobile health clinic run by undergraduate pharmacy students providing services to underserved communities. Int J Clin Pharm. 2024 Dec;46(6):1546–1551. doi: 10.1007/s11096-024-01783-1.
Akshay Doshi 1, Arthur Foster 1, William Adeboye, Cameron Niven
[1]
High-Fidelity (Hi-Fi) Simulation is essential in medical education, offering realistic clinical training in safe environments. However, the intensive resource requirements of specialised equipment, dedicated simulation suites, and trained instructors frequently limit students’ hands-on participation [1]. Many learners consequently spend most simulation sessions as passive observers. This study examines whether active participation in Hi-Fi Simulation leads to better performance in subsequent emergency scenarios compared to observation alone, while also investigating knowledge retention over time.
A longitudinal study was conducted with seven final-year medical students at a district general hospital. Participants first completed four emergency scenarios (DKA, sepsis, hyperkalaemia, major haemorrhage), actively managing one case while observing peers in others. Three months later, all students repeated the same scenarios using immersive VR technology. Performance was assessed through a validated scoring system evaluating clinical knowledge, procedural skills, decision-making, teamwork and time management.
Active participants consistently outperformed observers by an average of 20% in VR simulations. The most significant differences appeared in time critical decision making and complex clinical reasoning. Active learners also demonstrated superior procedural accuracy and showed greater confidence during VR scenarios. These benefits persisted across the three-month interval between sessions.
Our findings strongly support prioritising active participation in simulation training, even if this means covering fewer scenarios. This perhaps highlights a limitation in traditional Hi-Fi Simulation, with students spending more time in observational learning than participating. Using simulation as a tool meets the need of undergraduate students by increasing their knowledge and confidence during active participation. Future research should investigate the translation of simulation performance gains to real clinical outcomes.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Issenberg SB, McGaghie WC, Petrusa ER, et al. Features and uses of high-fidelity medical simulations that lead to effective learning: a BEME systematic review. Med Teach. 2005;27(1):10–28. doi: 10.1080/01421590500046924.
Nicholas Eames 1, Natalie Rowe 1, 3, Ghaniah Hassan-Smith 1, 2
[1]
[2]
[3]
Foundation doctors are expected to perform key ward-based tasks from the outset of clinical practice. However, clinical attachments alone may not provide consistent opportunities for skill development. Simulated ward rounds (SimWR) offer a standardised educational experience to supplement clinical placements. Previous literature highlights potential benefits of simulated ward activities, but call for further high-quality evidence [1]. Building on prior work [2], we developed an expanded SimWR programme, evaluating its impact on final-year medical students’ confidence with presenting cases – testing prescribing and both verbal and written documentation skills.
SimWR sessions were conducted in a newly-opened, 10-bed simulation ward on campus. Educational learning objectives were aligned with GMC and medical school undergraduate curricula requirements. Students were presented with an overnight completed clerking based on core medical conditions and were tasked to:
Present the patient to a senior decision-maker (role-played by consultants/ ST-level (post-MRCP) faculty members),
Document the simulated ward round encounter
Complete appropriate prescribing activities.
Each session concluded with structured debriefing focused on the three tasks. Initial learner confidence was assessed pre- first session, with post- questionnaires after subsequent SimWR. Confidence was rated using Likert scales. All participants self-selected for involvement; no exclusion criteria.
Ethical approval for this study was granted by the Research Ethics Committee, College of Health and Life Sciences (HLS), Aston University (REC ID: HLS21212).
Pre- and post-intervention questionnaires demonstrated significant improvement in reported confidence (see Figure 1):
Confidence in documentation and prescribing rose from 60% pre-intervention to 100% following two SimWR sessions.
Confidence in presenting to seniors increased from 77% after the first session to 100% by simulations 3&4.
These improvements were sustained across the remainder of the programme.
SimWR meaningfully enhanced final-year students’ confidence in core ward tasks, supporting their preparedness for clinical roles. Although limited by small sample size and self-selection for participation, the findings contribute to growing evidence supporting the integration of SimWR into undergraduate medical curricula. Future work should explore objective measures of performance and scalability to broader student cohorts.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Le K, Fagerlund AJ, Peacock O, Mercer SJ, Bissett I. The impact of simulated ward rounds on the clinical education of final-year medical students: a systematic review. Int Med Educ. 2024;3(1):100–115.
2. Hassan-Smith G and Rowe N. Simulated Ward Round (SimWR) for Final Year Medical Students. Presented at: ASPiH Annual Conference; 2024 Nov 3–5; Edinburgh.

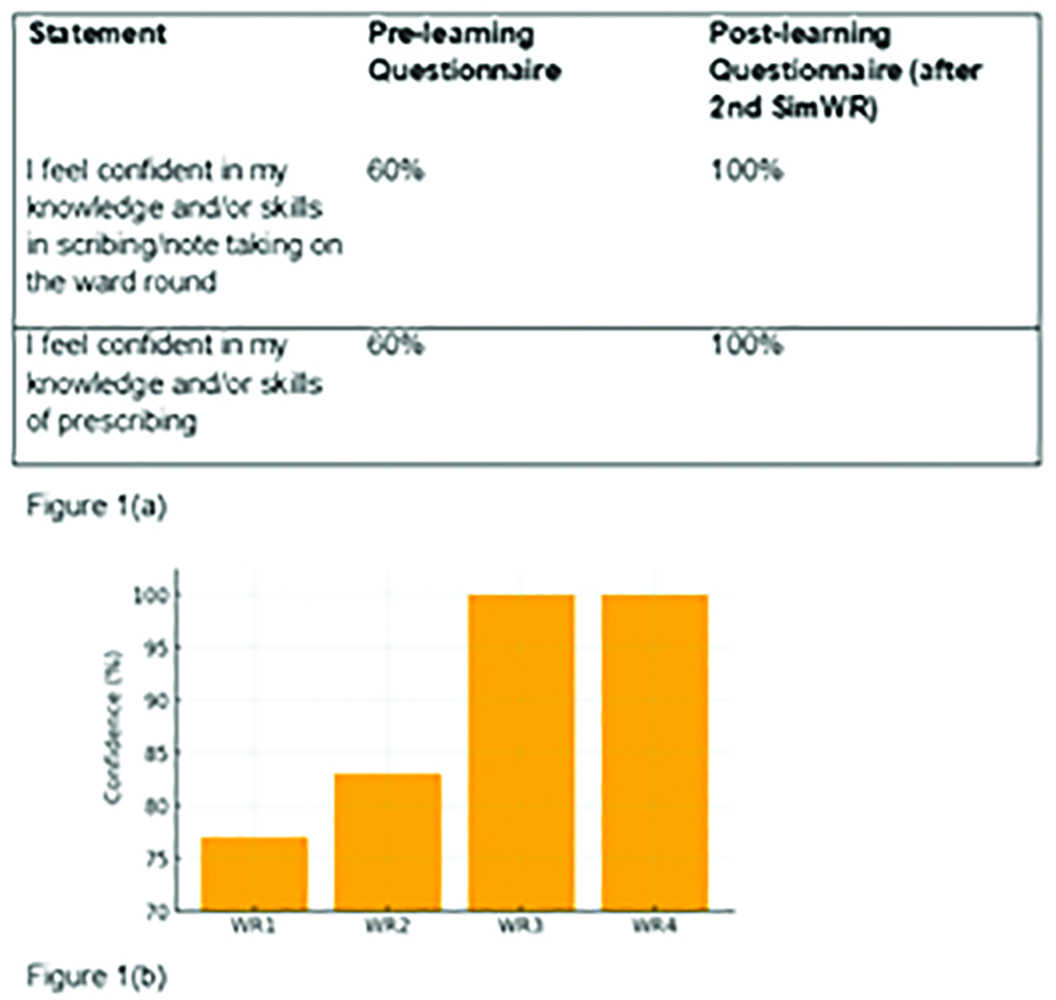
Confidence improvements in core ward tasks following SimWR sessions. 1(a): Confidence in scribing and prescrlibing. 1(b): Confidence with presenting to seniors over the course of SimWR sessions.
Matthew Bowker 1, 2, Alakh Konjengbam 1, 2, Deepta Churm 1, 2
[1]
[2]
Autism is characterised by lifelong differences in communication, behaviour, and social interaction [1]. Despite growing recognition of autistic individuals in healthcare professions [2], little is known about supporting autistic learners in simulation-based healthcare education (SBHE). This scoping review aimed to identify existing research on autistic learners in SBHE, map the current evidence base, and identify gaps to inform future research and educational practice.
We conducted a formal scoping review following PRISMA-ScR guidelines in May 2024 [3]. A comprehensive search strategy was developed with assistance from a research librarian, and the protocol was prospectively registered with the Open Science Framework on 12 April 2024. Eligibility criteria included studies involving autistic learners in simulation-based healthcare education contexts. We searched multiple databases between 1 January 2000 and 15 May 2024, identifying 1457 potentially relevant articles.
Despite a thorough search, no studies met our inclusion criteria, revealing a significant gap in the literature regarding autistic learners in SBHE. Through synthesis of related evidence from autism in higher education and healthcare settings, we identified potential challenges autistic learners may face in SBHE: sensory over-responsivity [1], difficulties with interpersonal communication underpinned by the ‘double empathy problem’ [3], imagination differences affecting suspension of disbelief, and distinct information processing patterns including weak central coherence.
We suggest adapting the Autistic SPACE framework [2] - originally developed for supporting autistic patients - to address the needs of autistic learners in SBHE. This approach emphasises considerations for Sensory needs, Predictability, Acceptance, Communication, and Empathy, providing structured recommendations for creating more inclusive simulation environments. Further research directly examining the experiences of autistic learners in SBHE is urgently needed to develop evidence-based support strategies.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Tavassoli T, Miller LJ, Schoen SA, et al. Sensory over-responsivity in adults with autism spectrum conditions. Autism. 2014;18(4):428–432.
2. Doherty M, McCowan S, Shaw SC. Autistic SPACE: a novel framework for meeting the needs of autistic people in healthcare settings. Br J Hosp Med. 2023;84(4):1–9.
3. Milton DEM. On the ontological status of autism: the ‘double empathy problem.’ Disability & Society. 2012;27(6):883–887.
Ashraya Harish 1, Rachel Farrelly 1, Olaoluwa Bolujoko 1
[1]
The role of the surgical multidisciplinary team (MDT), particularly surgical resident doctors and nurses, extends far beyond the confines of the operating theatre. The peri-operative ward environment presents unique clinical and communication challenges that demand a distinct skillset to manage complications in unpredictable, high-pressure situations. Formal team training in peri-operative complication management can lead to increased confidence among healthcare professionals, improved team cohesiveness, and positively impact on patient care [1]. Despite this, structured training for MDT members in managing such scenarios is limited. Simulation-based education provides a safe, reflective environment for healthcare professionals to develop these skills without compromising patient safety [2]. Recognising a gap in peri-operative simulation training for surgical MDTs, we developed a targeted programme to address this need.
A structured simulation-based teaching programme was implemented at Newham University Hospital, within Barts Health NHS Trust. The programme was designed for the surgical MDT, with particular focus on resident doctors and nursing staff. Scenarios were based on the CCriSP (Care of the Critically Ill Surgical Patient) framework and aligned with the surgical portfolio’s learning outcomes. Scenarios focused on common peri-operative challenges, including clinical deterioration, communication breakdowns, and ethical dilemmas. Participants completed pre- and post-session confidence surveys using Likert scales, analysed using a paired T-test. Qualitative feedback was collected anonymously via an online feedback form.
Thirteen MDT members (12 surgical residents and 1 student nurse) participated in the simulation sessions. Of these, four submitted feedback forms. Preliminary analysis showed a statistically significant increase in self-reported confidence in managing peri-operative scenarios, rising from 50% pre-session to 95% post-session (p=0.0182). All respondents found the sessions and debriefs beneficial to their learning, and 75% expressed interest in receiving post-session summaries. Logistical barriers, especially concurrent clinical commitments, limited attendance during working hours. The small number of nursing participants also highlighted the need for broader MDT engagement.
Initial findings suggest that simulation is an effective educational method for improving confidence and preparedness in managing peri-operative complications among surgical MDT members. Despite the small sample of formal feedback, positive trends and qualitative responses indicate this model fills a critical gap in surgical education. Barriers to attendance and limited nursing involvement prompted plans to transition to in-situ simulation delivery within clinical areas. This shift aims to increase realism, reduce simulation artefact, and facilitate greater MDT participation. Ongoing evaluation will support iterative improvements and inform integration into broader surgical education frameworks.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable
1. Gillespie BM, Chaboyer W, Murray P. Enhancing communication in surgery through team training interventions: a systematic literature review. AORN J. 2010;92(6):642–57. doi: 10.1016/j.aorn.2010.02.015.
2. Elendu C, Amaechi DC, Okatta AU, Amaechi EC, Elendu TC, Ezeh CP, et al. The impact of simulation-based training in medical education: A review. Ann Med Surg (Lond). 2024;85:103958. doi: 10.1016/j.amsu.2024.103958. PMID: 38968472; PMCID: PMC11224887.
Robyn Stiger 1, Rachel Bloodworth Strong 1, 2
[1] School of Heath Science and Technology,
[2]
Virtual reality (VR) immersive technologies are an emerging area in healthcare education involving a digital representation of a 3D environment and a head-set to “block out the real world” [1]. They allow for controlled, standardised and repeatable interactions [2] promoting equitable access to high-fidelity learning. Successful implementation necessitates collaboration with learners, to inform development of the product. The session aim was to create a platform for Occupational Therapy (OT) students to develop skills and knowledge with people experiencing suicidal ideation. This module was new for the OT programme.
A half-day session was designed for 53 OT 2nd year prequalifying students at Brookes University Oxford. The VR module was entitled “The mental health practitioner” developed by Bodyswaps™, A preceding on-boarding session had been organised to familiarise students with the Bodyswaps™ platform. Students rotated in groups into a skills lab set up with the VR headsets but joined together in a classroom for a pre-briefing on ground rules, using VR headsets and psychological safety. Students interacted with a virtual patient experiencing suicidal thoughts, choosing responses to her statements and receiving feedback. The experience allowed for self-reflection, students assuming the role of the patient, listening to their own responses embodied by a chosen ‘avatar’. A debrief session was followed by a theory-based seminar on suicide.
Students completed an evaluation with Likert scales and free text questions. The session was overall well rated. 20/26 (77%) scored the session at least 7 out of 10. 65% indicated 7 or more out of 10 (10 being strongly agree) that the session helped them improve skills in relation to mental health practice. Some students preferred VR to live simulation while some felt it was artificial. There was a prominent theme around more time, privacy and space.
The session allowed students to practice difficult conversations in a low-risk immersive environment, through reviewing their own responses and appreciating the patient’s perspective, increasing preparedness for placement and future practice. Faculty staff could use the feedback to develop the module as an alternative to more familiar live-actor simulation. The debrief and theory session supported reflection and theoretical understanding. Feedback indicates a demand for more VR-based mental health training in the future and scope to develop this further for OT teaching.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Lie SS, Helle N, Sletteland NV, Vikman MD, Bonsaksen T. Implementation of Virtual Reality in Health Professions Education: Scoping Review. JMIR Medical Education. 2023;9:e41589.
2. Elendu C, Amaechi DC, Okatta AU, Amaechi EC, Elendu TC, Ezeh CP, Elendu ID. The impact of simulation-based training in medical education: A review. Medicine. 2024;103(27):e38813.
Valentina Zaccarini 1, Emma Smith 1, Laura Halpin 1
[1]
IMG (International Medicine Graduate) doctors play a key role in the NHS and in Children’s Services they account for approximately one third of the medical workforce [1]. Despite this, the support they receive when starting to work in the United Kingdom is often suboptimal, making the transition extremely challenging [2]. This is often reflected in the higher number of referrals to the GMC (General Medical Council) compared to UK trained colleagues [3]. We explored the feelings of IMGs around the time they were newly employed in the NHS and the option of tailored simulation scenarios as a key tool to help them integrate.
A survey was distributed to IMGs working in the KSS (Kent, Surrey and Sussex) Deanery with the goal of establishing how challenging they found it to start working in the NHS, whether they felt targeted simulation sessions would be useful, the best time for these to be offered and what topics would be most beneficial to cover.
We collected a total of 32 responses: 90% of respondents reported having found it challenging to start working in the NHS, with nearly a third of them stating it was an extremely stressful time. All respondents felt that targeted simulation sessions would be helpful, with just under half preferring these to be incorporated into their induction and the remaining shortly after this. Communication was felt to be the biggest challenge by 30 out of 32 respondents, shortly followed by how to escalate and ask for help (27 out of 32 respondents), cultural aspects and hand overs (24 and 23 out of 32 respondents respectively). Approximately two thirds of the interviewed would like to see ‘How to deal with difficulties within the team’ to also be addressed. 85% of the respondents who had attended simulations before felt this would be a suitable tool to help IMGs settle into the NHS.
Our survey confirmed that IMGs that are newly employed by the NHS face significant stress and need more support, especially with regards to communication, asking for help and escalating concerns, and cultural aspects related to the job.
Simulation has been widely recognised to be an excellent tool for training in healthcare and tailored scenarios have been designed and implemented in the Paediatric KSS Deanery to support newly joining IMGs integrating into the NHS.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. General Medical Council Data Explorer, General Medical Council. Available from: www.gmc-k.org/doctors/register/search_stats.asp. Accessed 29 September 2024.
2. Lane J, Nitin Shrotri, Somani BK. Challenges and expectations of international medical graduates moving to the UK: An online survey. Scott Med J. 2024;69(2):53–58. doi: 10.1177/00369330241229922.
3. Jalal M, Bardhan KD, Sanders D, Illing J. International: Overseas doctors of the NHS: migration, transition, challenges and towards resolution. Future Healthc J. 2019 Feb;6(1):76–81. doi: 10.7861/futurehosp.6-1-76.
Anurag Bhatnagar 1, Chris Simcox 1, Lok Chau 1, Katie Davies 1
[1]
Virtual Reality (VR) has emerged as a promising tool in healthcare education, offering immersive experiences to support learning and professional development. At Sheffield Hallam University, VR was integrated into the BSc Physiotherapy curriculum to enrich simulated placement experiences. The initiative targeted key educational domains such as Equality, Diversity, and Inclusion (EDI), human anatomy, and soft skills. This study investigates the impact of VR on student engagement, learning, and skill application using the Kirkpatrick Evaluation Model [1].
The study employed a mixed-methods evaluation of VR integration across three modules—Anatomy VR, Travelling While Black, and BodySwaps. Data were collected through student feedback surveys and reflections, focusing on the four levels of the Kirkpatrick Model: Reaction, Learning, Behaviour, and Results. Additional insights were gathered from the VR facilitation team and reviewed alongside supporting literature to inform improvements [2,3].
Reaction: 36% of students responded positively to the VR sessions, while another 36% remained neutral, and 28% reported dissatisfaction. Technical issues and discomfort, particularly with BodySwaps, were common concerns.
Learning: Travelling While Black and Anatomy VR sessions were effective in promoting EDI awareness and anatomical understanding, respectively. BodySwaps yielded limited success in enhancing communication and active listening.
Behaviour and Results: While 48% of students reported confidence in applying VR-acquired skills to clinical placements, 36% did not, highlighting inconsistencies in perceived transferability of learning.
Preliminary Recommendations: Pre-briefings, content alignment with real-world scenarios, and improved accessibility are expected to enhance future VR effectiveness.
VR holds significant potential to augment physiotherapy education by fostering experiential learning and addressing EDI and communication competencies. However, to maximise impact, sessions must be better tailored to learners’ needs and technological limitations addressed. The mixed reception to BodySwaps indicates the importance of context and clarity in simulation design. Future work will assess the impact of the proposed recommendations on student outcomes and engagement.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable
1. Kirkpatrick JD, Kirkpatrick WK. Kirkpatrick’s Four Levels of Training Evaluation. ATD Press; 2016.
2. Radianti J, Majchrzak TA, Fromm J, Wohlgenannt I. A systematic review of immersive virtual reality applications for higher education: Design elements, lessons learned, and research agenda. Comput Educ. 2020;147:103778.
3. Smith S, Hamilton A. The role of virtual reality in enhancing learning and engagement in health professional education: A review. Med Teach. 2021;43(3):300–307.
Sheffield Hallam Tech team (TORS)
Emily Lyness 1, Emer Forde 1, Simon Phillips 1, Matthew Turner 1, Adam Fraser 1, Aurelia Butcher 1, Clare Wedderburn 1
[1]
GPs are increasingly expected to manage acutely unwell patients presenting in the community setting1. Evidence suggests that simulation-based training (SBT) for the management of the deteriorating patient is valuable for qualified GPs 2,3. GPs in training rotate through hospital posts so are likely to have had recent exposure to acutely unwell patients, so we wanted to know would a similar approach using SBT be valuable to GPs in training?
We surveyed a cohort of GPs in their final training year about their experiences of managing common emergencies in hospital and in primary care settings. We also asked them to rate their confidence in the theoretical and practical management of emergencies in the primary care setting. Participants then engaged with a SBT on the management of eight common emergencies. This took place in a classroom, but participants were asked to consider their current GP workplace and only equipment obtainable in this setting was available in the SBT. Following the session, participants re-rated their confidence in the management of emergencies and provided free-text comments.
The pre-training survey revealed participants had some experience of managing emergencies in hospital; but very few had experience in the GP setting. Our before and after training demonstrated an increase in confidence in both the theoretic (av. 27%) and practical (av. 49%) management of all scenarios. When asked what they found most valuable, participants’ comments gave an insight into why and how their confidence had been enhanced; “practical skills - setting up nebs machine, giving IM adrenaline, making up antibiotics”. Participants particularly valued the SBT approach; “role play helped in visualising the situation in primary care”, “it’s really good to have actual clinical scenarios rather than just slides and to see actual stuff in real life”.
These findings echo studies evaluating SBT for qualified GPs and support the notion that SBT is valuable, but also highlights organisational and equipment issues which have the potential to delay life-saving treatment in medical emergencies [1-3]. By providing this SBT to GPs in their final year of training it is anticipated that this will facilitate a more confident primary care workforce, however, we advocate, as others have, that regular SBT would be beneficial to maintain safe management of time critical emergencies in the community [2,3].
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable
1. Gauznabi S. Impact of emergency simulation training in primary care: a rapid review. Journal of Primary Health Care. 2024 June.
2. Maloney A, Field PE. In situ simulation training for management of emergency situations and deteriorating patients in GP surgeries. BMJ Simul & Technol Enhan Learn. 2018;4(2):A32–33.
3. Forde E, Bromilow J, Jackson S, Wedderburn C. Managing emergencies in primary care:does real-world simulation-based training have any lasting impact? BMJ Simul Technol Enhanc Learn. 2018 Nov 29;5(1):57–58.

| The practical management of emergencies in primary care; evaluation of a brief simulation-based teaching for GPs in training. | ||||
|---|---|---|---|---|
| SBT Emergency Scenario theme | % of participants with experience of managing emergencies in hospital (n=25) | % of participants with experience of managing emergencies in a GP setting (n=19) | % improvement in self-rated confidence in the theoretical management of emergencies after SBT | % improvement in self-rated confidence in the practical management of emergencies after SBT |
| Acute coronary syndrome | 84% | 47% | 22% | 33% |
| Cardiac arrest | 80% | 0% | 21% | 31% |
| Hypoglycaemia | 80% | 11% | 27% | 52% |
| Seizure | 72% | 0% | 53% | 72% |
| Anaphylaxis | 24% | 5% | 29% | 45% |
| Severe asthma | 84% | 32% | 31% | 49% |
| Sepsis | 100% | 63% | 5% | 40% |
| Meningitis | 6/25 | 0% | 29% | 71% |
Tara Cusack 1, Siobhan Brereton 1, Lara Gillespie 1
[1]
Ireland’s clinical education capacity for health and social care faces pressure, exacerbated by a 33% vacancy rate across healthcare profession posts. With the government aiming to increase healthcare students in the education system there is a need for innovative clinical education models.
The aim of this project was to co-design technology assisted interdisciplinary learning and simulation, with key stakeholders, to improve sustainable clinical education.
A World Cafe methodology was used to co-design interdisciplinary simulation education for graduate entry physiotherapists, dieticians and graduate nurses specialising in cardiology. This was achieved with students from each discipline, patients, academics, clinicians and educational technologists. Three key themes emerged: (1) The Importance of communication, (2) Straight forward information sharing, (3) A Patient-Centred approach. These themes underpinned the development of two simulation scenarios. The simulations were rolled out and evaluated using the Simulation Effectiveness Tool (SET) [1] and the Interprofessional Collaborative Competencies Attainment Survey (ICCAS) [2].
Seventy students participated in small interdisciplinary groups (25 graduate entry physiotherapy students, 24 Graduate entry dieticians and 21 Cardiac Care Nurses). Fifty-five students responded to SET. The key findings are as follows: 89% (49) of students strongly agreed they were better prepared to respond to changes in their patients’ conditions based on the simulation scenario, with 82% (45) of the students strongly agreeing they felt more confident in communicating with their patient. 48 (87%) students strongly agreed the debriefing session provided opportunities to self-reflect on their performance during the simulation.
Fifty students responded to ICCAS. The following key findings were noted, before participating in the simulation only 17% (9) of students felt very confident they were able to address team conflict in a respectful manner, whereas 68% (34) felt very confident post-simulation. Before participating 40% (21) of students strongly agreed they were able to actively listen to the perspectives of interprofessional (IP) team members, compared to 84% (46) after the simulation. 70% (35) of the students felt very confident using an IP team approach to assess the patient’s health situation, compared to only 13.5% (7) prior the simulation.
The findings of this interdisciplinary simulation project illustrate that students achieved the learning outcomes identified for this module which were: creating a better understanding of roles and responsibilities of colleagues; empowering students to navigate and negotiate the clinical setting while working effectively with other disciplines to improve patient care and improving student knowledge and understanding of patient care.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable
1. Leighton K, Ravert P, Mudra V, Macintosh C. Updating the Simulation Effectiveness Tool: Item Modifications and Reevaluation of Psychometric Properties. Nurs Educ Perspect. 2015 Sep-Oct;36(5):317–23. doi: 10.5480/15-1671. PMID: 26521501.
2. Archibald D, Trumpower D, MacDonald CJ. Validation of the interprofessional collaborative competency attainment survey (ICCAS), Journal of Interprofessional Care. 2014;28(6):553–558. doi: 10.3109/13561820.2014.917407.
This project was funded by the National Forum for the Enhancement of Teaching and Learning in Higher Education Strategic Alignment of Teaching and Learning Enhancement (SATLE) Fund.
Kieran Hardern 1, Hannah Parker 2
[1]
[2]
The IMT Stage 2 curriculum, introduced in 2022, emphasised simulation-based education with a focus on human factors to progress at ARCP [1]. Existing simulation for Medical Registrars remains limited and rarely integrates these elements [2,3].
We developed a one-day simulation course for ST4-5 registrars, embedding human factors into each scenario to meet curriculum needs. To enhance realism and observer engagement, we also created a web-based patient record enabling faculty-controlled access to documentation and results.
The course, GIM-Sim:3, was piloted in March 2025. Eight scenarios were developed, each with a distinct human factors theme and integrated clinical case, mapped to the IMT Stage 2 curriculum. Clinical topics were selected to differ from earlier courses in the series and aimed to support ARCP requirements for Stage 2. Candidates completed a pre-course questionnaire to identify knowledge or portfolio gaps, enabling pre-allocation of scenarios aligned to their goals.
A “Simulated Electronic Patient Record” (Sim-EPR) was created to enhance the scenario experience and ensure equal access to information for observers. This mobile-optimised web platform provided access to notes, results, and guidelines—controlled by faculty via the interface. Candidates could access results and protocols as in practice, while observers viewed the same information in real-time, and embedded faculty could realistically “look up” information when delegated.
All candidates found the simulations interesting, with clear and effective delivery. All reported that learning from the day would impact their practice and said they would recommend the course to other trainees.
Participants rated each scenario for clinical relevance and human factors relevance (1: not at all relevant, 5: highly relevant). Every scenario averaged above 4.5 in both areas, with no rating below 4 (Figure 1).
Eighty per cent of candidates felt the electronic patient record enhanced their experience, and none rated it negatively.
Our high-fidelity simulation courses allow candidates to browse notes and guidelines, request tests, and view results. However, observers often struggle when results are visible only to active candidates. We developed the Sim-EPR to enhance fidelity—reflecting the longstanding use of electronic records in the UK—and to give observers access to the same information, improving engagement and learning.
This system was piloted alongside our new high-fidelity human factors course, addressing a key gap in the IMT Stage 2 curriculum. Scenarios were designed primarily around human factors, with clinical cases developed to fit, ensuring full integration and realism within NHS practice.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Joint Royal Colleges of Physicians’ Training Board. Internal Medicine Stage 2 Training Curriculum [Internet]. 2022 [cited 2025 Apr 14]. Available from: https://www.thefederation.uk/sites/default/files/Internal%20Medicine%20(Stage%202)%202022%20curriculum%20FINAL%20200522_0.pdf.
2. Abildgren L, Lebahn-Hadidi M, Mogensen C, et al. The effectiveness of improving healthcare teams’ human factor skills using simulation-based training: a systematic review. Adv Simul. 2022 May 22;7(1):12. doi: 10.1186/s41077-022-00207-2.
3. Tipton A, Chatfield S, Waterhouse E. A100 A novel simulation course for GIM (General Internal Medicine) registrars, which fulfils the new GIM stage 2 curriculum simulation requirements. J Healthc Simul. 2024 Nov;4(Suppl 1). doi: 10.54531/FDRV1134.
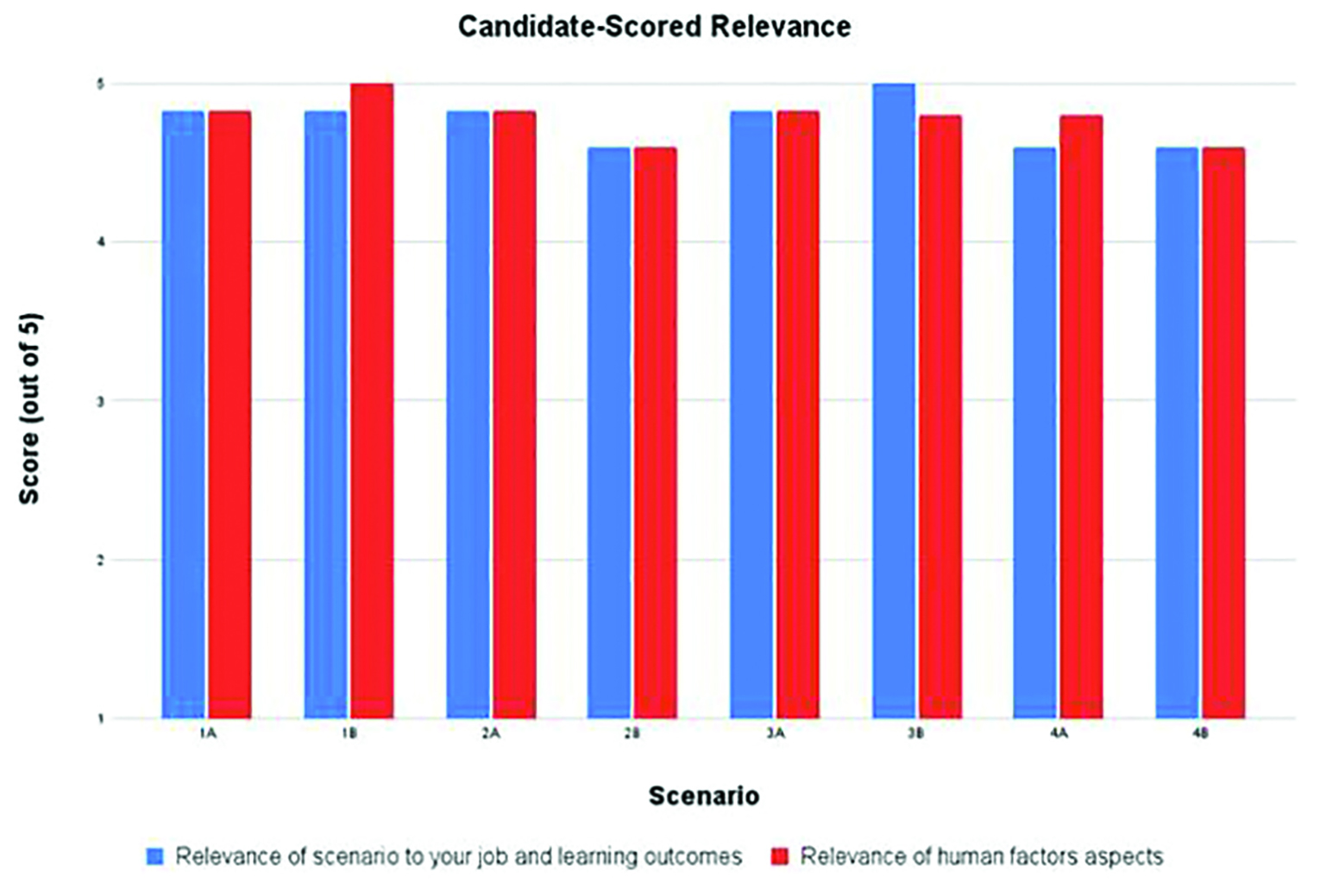
Richard Buckley 1, Barry Featherstone 1, John Coombes 1
[1]
It was identified in our hospital trust that emergency paediatric intubations were infrequently encountered by staff across the year, resulting in low levels of confidence in management. With winter approaching, it felt pertinent to design and deliver teaching on this topic, simulating the preparation for intubating a bronchiolitic baby. The learning objectives were to increase confidence and knowledge, and also signpost candidates to relevant guidelines [1]. The aim was to capture as many anaesthetic and theatre staff as possible, utilising tea-trolley simulation to allow for multi-disciplinary (MDT) candidates to attend each session.
The session-design discussed a simulated case of an ex-premature bronchiolitic baby requiring intubation. Permission was gained from theatre matrons to deliver this in the main-theatres of the trust’s 2 acute sites across 4 days. Both anaesthetists and theatre practitioners were invited to attend. Candidates completed a pre-session questionnaire regarding confidence in management, clinical knowledge and awareness of guidelines. The session lasted 45 minutes, using table-top discussion to talk through the scenario in a learner-led way, with a facilitator present. A post-session candidate questionnaire was then completed.
A total of 73 staff attended as candidates. 46.6% were theatre practitioners and 53.4% anaesthetists of different grades. The post-session questionnaire reported an increase in confidence levels in; equipment preparation (41.1% - 84.8%); drug preparation (32.9% - 73.8%); ventilator set up (19.1% - 67.7%). A comparison of the findings, including verbal feedback, is summarised in Table 1.
The results demonstrate a clear improvement in confidence levels in knowledge of all topics covered relating to the preparation for intubating a bronchiolitic baby, as well as an almost complete download of the relevant guidelines. It is testament to the effectiveness of low-fidelity table-top simulation as a means to facilitate effective and relevant education. By delivering this ‘tea-trolley style’ intervention in main theatres on each site, it enabled far greater capture of the target candidates, avoiding the barriers often encountered when learners have to attend a remote location, whilst also utilising the shared learning of an MDT. A limitation of this intervention was that it only focussed on one topic, and candidate feedback requested a wider range of topics to be covered. Feedback did however recognise the relevance of this topic, therefore planning is underway to embed this as an annual educational intervention within the trust, ensuring staff remain upskilled in dealing with these acute presentations.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Lillie J, Lambert J. Paediatric Critical Care, Severe Bronchiolitis [Internet]. Place of publication: GTi Clinical Guidance Database and Evelina London Website. 2022 Sept 14th. [Cited 2025 Mar 31]. Available from: https://www.evelinalondon.nhs.uk/resources/our-services/hospital/south-thames-retrieval-service/Severe-bronchiolitis.pdf

| % Confident/Very confident in airway equipment preparation | % Confident/Very confident in drug preparation | % Confident/Very confident in ventilator setup | % Download of correct guidelines | |
|---|---|---|---|---|
| Pre-session questionnaire | 41.1% | 32.9% | 19.1% | 63% |
| Post-session questionnaire | 84.8% | 73.8% | 67.7% | 97% |
| Verbal feedback | “Great exposure to small paeds, all of session was massive learning experience” | “Very helpful to drill through the scenario and practise the calculations that we don’t do frequently” | “Walking through the kit. De-mystified elements” | “Having a variety of people with different skill level to give opinions” |
Sanni Lahti 1, Sherin Samuel 2
[1]
[2]
The Nursing & Midwifery Council (NMC) now mandates nursing students to replace 600 clinical hours with simulated practice learning (SPL) [1]. While Higher Education Institutions (HEIs) are incorporating this shift into curricula, aligning simulation with clinical competencies remains a challenge. Traditional skills training is often hands-on but lacks realism and practical transferability [2].
To bridge the gap between theoretical knowledge and clinical application, we developed a procedural simulation model that embeds clinical skills training within structured simulation scenarios. This model aligns with NMC standards and best practice guidelines, supporting the development of core nursing competencies in realistic settings that are replicable in practice.
This study evaluates the model’s effectiveness in enhancing students’ clinical competence, knowledge, and skills while meeting SPL requirements.
The procedural simulation model was embedded within the curriculum to align with NMC proficiencies for each academic year [1]. Procedural Simulation (Pro Sim) sessions included hands-on practice with equipment and high-fidelity mannequins, scenario-based learning, and structured debriefing with facilitators [2].
Pro Sim was delivered during the first two days of each SPL week, with students grouped by field of practice. To accommodate individual learning styles, students participated in small-group simulations reflecting real-life clinical scenarios [2]. Each three-hour session included a theoretical overview, tutor-led demonstrations, supervised hands-on practice, and debriefing to support reflective learning and knowledge retention.
Informal feedback from students highlighted significant improvements in clinical skills competence and confidence as independent practitioners following Pro Sim sessions. Evaluation data also indicated enhanced communication skills, stronger teamwork abilities, and improved responses to real-life clinical situations, with a noticeable reduction in anxiety about clinical placements.
For example, feedback on the Medication Management Pro Sim reflected these overall positive outcomes (Figure 1). Additionally, the Pro Sim model fostered a supportive, culturally competent, and inclusive learning environment.
The Pro Sim model integrates simulation into traditional instructional methods, strengthening existing simulation-based education by allowing students to practice, evaluate, and refine their clinical competencies [1]. A comprehensive plan is in place to collect both qualitative and quantitative data to evaluate the model’s sustained impact on students’ clinical practice.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Holt P. Simulated practice learning in pre-registration nursing programmes [Internet]. 2024 [cited 2025 March 26]. Available from: https://www.nmc.org.uk/globalassets/sitedocuments/simulated-practice-learning/reports/2024/evaluation-of-simulated-practice-learning-in-pre-registration-nursing-programmes.pdf
2. Gent D, Kainth R. Simulation-based procedure training (SBPT) in rarely performed procedures: a blueprint for theory-informed design considerations. Adv Simul. 2022;7:13. doi: 10.1186/s41077-022-00205-4
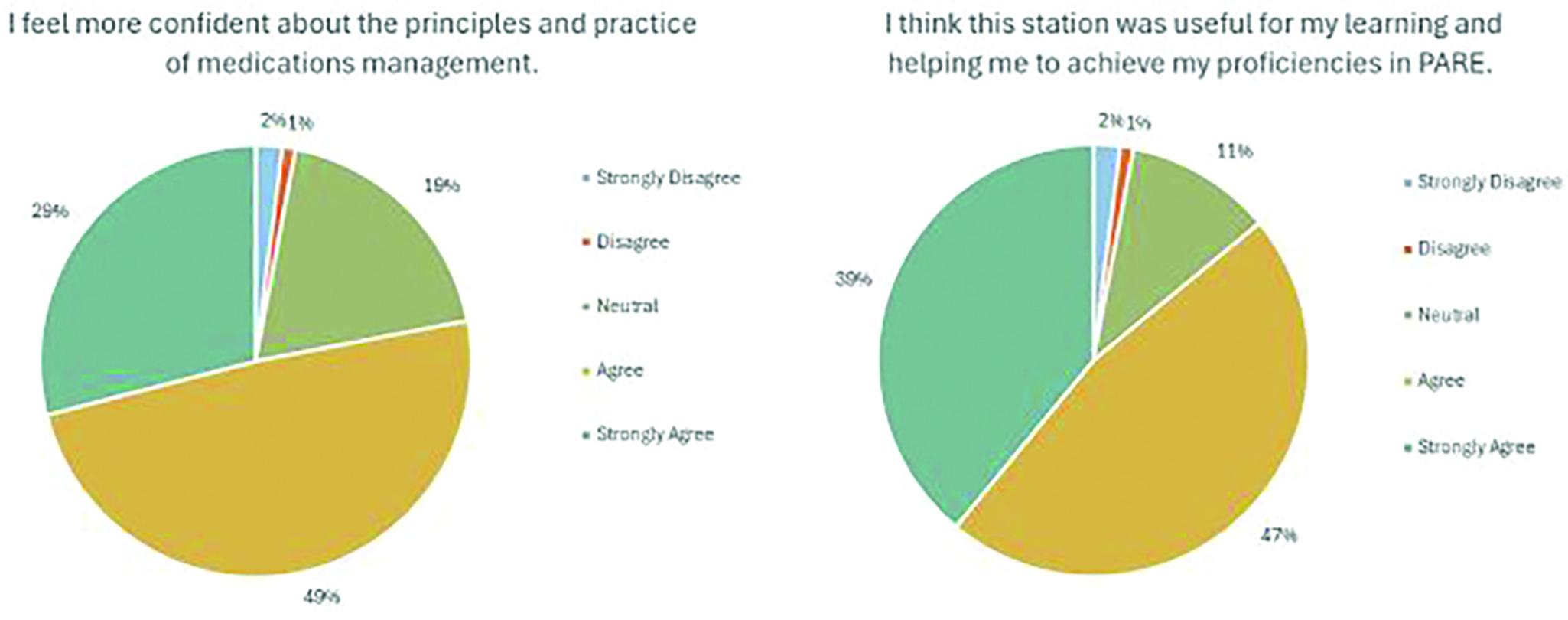
Una Brosnan 1, Charlotte Mutton 1, Debbie Holley 1, Jakob Rossner 1
[1]
Over 500 interdisciplinary healthcare students from Bournemouth University’s Faculty of Health & Social Sciences took part in a two-day interprofessional simulation event, simulating a major incident: an alien invasion causing organised chaos in an underground car park. Students from multiple healthcare disciplines (Adult, Mental Health, and Children’s and Young People’s Nursing, Paramedic Science, Physician Associates, and Physiotherapy) collaborated with makeup artists from Arts University Bournemouth to create high-fidelity injuries, practicing triage, emergency care and teamwork in a controlled, immersive setting.
The NHS Long Term Workforce Plan highlights simulation as a key strategy to modernize healthcare education, supporting interprofessional education (IPE) and exposure to rare and complex scenarios [1]. Higher Education Institutions (HEI) play a vital role in preparing students to deliver safe, effective and innovative care.
Simulation fosters essential communication, collaboration and decision-making skills, while major incident simulations enhance both technical and non-technical abilities to improve emergency readiness [2]. By promoting IPE, these experiences help build a resilient healthcare workforce equipped to handle major incident events and deliver high-quality patient care [3].
Drawing on our faculty’s interprofessional expertise, we designed clear scenarios with learning objectives, intending to integrate students’ theoretical knowledge and practical skills. Recognizing the potential for emotional responses, we integrated wellbeing staff and hot and cold debriefings. Central to the design was the establishment of a formative, psychologically safe environment, prioritizing participant growth and emotional safety. Planning involved careful consideration of learning objectives and support structures to allow learners to engage fully. This comprehensive approach facilitated reflection, iterative improvements and a supportive environment for learning from challenging experiences (Figure 1).
An educational evaluation, using thematic analysis of student feedback, demonstrated that this major incident simulation offered valuable realism, hands-on experience and promoted teamwork. Identified challenges, including noise and equipment issues, will inform improvements centred on scenario variety, multidisciplinary collaboration, and optimised resources. The limitation of primarily discipline-specific teams will be addressed through future focus on experiential learning to underpin and fully integrate IPE with the inclusion of the remaining disciplines in our faculty, for a more holistic, collaborative educational experience.
This evaluation demonstrates that a major incident simulation effectively builds key skills for interprofessional healthcare students. Realism was valued; noise levels and equipment access were challenges. Future improvements developed with our interprofessional partners will optimize debriefing and IPE, aligning with the NHS Long Term Workforce Plan [1].
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable
1. NHS. NHS Long Term Workforce Plan. NHS; 2023.
2. Ledbury J, Pike K, McLellan S, et al. Learning From Simulating Mass Casualty Events: A Systematic Search and a Comprehensive Qualitative Review. Disaster Med Public Health Prep. 2022;16(5):1897–1907.
3. Xavier J, Brown D. Interprofessional Education in a Simulation Setting. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.

Rachel Cichosz 1, Fateh Singh 1, Harjinder Kainth 1
[1]
Faculty development is imperative to delivering and maintaining high quality, impactful simulation-based education (SBE). The ASPiH guidelines outline key attributes of simulation faculty and encourage a culture of shared knowledge and expertise. [1] At The Royal Wolverhampton NHS Trust (RWT), we designed and implemented an innovative educational experience aimed at the novice SBE facilitator to ensure development of simulation faculty in keeping with ASPiH standards. The course is free and available to all RWT employees with an interest in becoming involved in SBE - from those hoping to develop their own departmental in-situ simulation programmes to those already having established roles within existing SBE. The full-day course includes workshops and simulated scenarios, with planned debriefs and meta-debriefs to optimise participant reflection and learning. The culture of the course is such that anyone from the wider multidisciplinary team (MDT) can attend, and peer observation and reflection is encouraged and facilitated.
The course was developed following identification of learning need during an upsurge in the amount of in-situ SBE activity within RWT. Market research revealed several other faculty development courses available within the region, however these all involved high costs for participants, with varying curricula. Course content was developed with inputs from established faculty members. A pilot course was delivered in April 2025 with 7 participants. Pre- and post-course surveys were conducted to assess impact and acceptability, and analysed using non-parametric statistical analysis. Free-text answers were evaluated using thematic analysis.
Participant confidence significantly improved in a range of areas, including their understanding of learning theory and how it relates to SBE (P=0.008), facilitating debrief sessions (P=0.03), managing a ‘difficult candidate’ (P=0.0004), and understanding of the terms ‘Human Factors’ and ‘Non-Technical Skills’ and their relevance to SBE (P=0.002). Free-text responses evaluated the course as ‘Clear objectives’, ‘Interactive’, ‘Very enjoyable’.
Feedback from our pilot course is significantly positive and we hope to deliver further this course routinely throughout the next 12 months, to ensure there is opportunity for all interested to attend and develop more robust data in terms of participant numbers. Participants enjoyed this course so much that many asked for a ‘part 2’ of this course which is currently under development. We hope that by sharing this success with the wider simulation community we may encourage a culture of collaboration and shared learning and expertise.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Diaz-Navarro C, Laws-Chapman C, Moneypenny M, Purva M. The ASPiH Standards - 2023: guiding simulation-based practice in health and care. Available from: https://aspih.org.uk
Rosalind Brown 1, Julia Hall 1
[1]
Our busy children’s emergency department sees a high turnover of Resident Doctors from a range of training pathways, many of whom have had limited exposure to paediatrics in their careers to date. In addition, there has been a growing nursing team over recent years and the department hosts a number of student nurses from local universities. Simulation has an ever-growing presence in many aspects of medical education, providing a safe environment for learners to build confidence and competence, particularly in high-stakes emergency scenarios [1]. Short, low fidelity simulation sessions were already regularly used in our department and we therefore elected to build on this premise to create a bespoke simulation-based study day aimed at junior colleagues to further enhance clinical practice.
With support from our simulation and education nurses, we created a simulation study day aimed primarily at junior medical and nursing staff. We aimed to cover a range of paediatric emergencies with medical and trauma presentations across a range of ages. Scenarios were either written specifically for the course or adapted from other locally used resources. The sessions were delivered in the hospital’s dedicated simulation suite using high fidelity child and infant simulators (Gaumard: Paediatric HAL and Super TORY). The scenarios can also be easily adapted to use lower fidelity mannequins in other centres. We ran the study day twice per six-month medical rotation from March 2024–March 2025 in order to maximise attendance opportunities. The course was adapted in response to feedback after each iteration.
We have had approximately 25 candidates attend the course thus far with questionnaires completed by 22 learners. The responses reflect the mix of attendees: 8 were from doctors working at ‘Senior House Officer’ level; 8 nurses (Band 5 and above); 3 healthcare assistants/associate practitioners (Band 4 and below); and 3 student nurses. Feedback was overwhelmingly positive: 20/22 (90.9%) reported their confidence improved following the course. Qualitative feedback identified key themes including a supportive learning environment, effective debriefs and a good range of scenarios covered.
We have been pleased with the reception of our new course and have taken steps to ensure the project’s longevity by ensuring permanent senior staff members in the department are involved in its ongoing organisation and delivery. We also plan to make our resources available as a free package for use in other emergency departments in the region or further afield.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Clerihew L, Rowney D, Ker J. Simulation in paediatric training. Archives of Disease in Childhood - Education and Practice 2016;101:8–14.
We would like to thank the following colleagues for their support with the project: Ehmendip Dulay, Marvi Kesinro & Aidan Wilson.
Yahye Mohamud 1, Andrew Gibson 1, Roshni Das 1, Shreeya Mehta 1, Yosha Pathak 1, Nia Williams 2
[1]
[2]
Sensory overload in children with autism spectrum disorder (ASD) poses considerable challenges within hospital environments, often resulting in heightened anxiety and behavioural disturbances [1]. Despite the increasing recognition of these needs, there remains a significant gap in research concerning the use of simulation-based education as a preparatory tool for healthcare professionals [2]. This review examines the impact of simulation training on paediatric staff managing sensory distress and aggression in children with ASD. In addition, the review will examine outcomes related to knowledge retention and practical skill development, while identifying barriers to the implementation of such training in clinical settings.
A rapid review design was employed to synthesise literature on simulation-based training for healthcare professionals managing sensory stressors in paediatric patients with ASD. Studies published from 2001 onwards were included, with searches conducted in Embase and Google Scholar. Search terms encompassed simulation training, paediatric medical staff, confidence, competence, and sensory overload. A PRISMA flow chart outlined the study selection process (Figure 1). Thematic analysis identified key themes related to training needs, barriers to stressor management, and simulation outcomes, while a narrative synthesis summarised intervention impacts and implementation challenges. Quantitative outcomes were presented using summary tables, bar charts, and bubble plots.
A total of 254 references were initially identified, 4 duplicates removed, 250 studies remained, of which 199 were excluded. 51 full-text articles assessed, 27 were excluded, 24 studies included in the final review. Simulation-based training significantly improved healthcare providers’ ability to manage sensory overload and behaviours in children with ASD. VR-based Behavioural Skills Training notably enhanced the accuracy of Functional Communication Training steps, while paediatric nurses reported increased confidence in handling ASD-related behaviours. Simulation exercises also improved diagnostic accuracy, communication, and clinical decision-making.
The findings of this systematic review highlight the transformative potential of simulation-based training in improving the skills, confidence, and competence of healthcare professionals managing sensory overload and behavioural challenges in children with ASD. Studies demonstrated significant improvements in diagnostic accuracy, communication, and critical thinking with technologies like virtual reality offering immersive and representative training experience. However, barriers such as small sample sizes, limited studies, and inconsistent reporting of difficulties faced by participants, particularly in VR were noted. Future efforts should focus on expanding current research inclusivity to improve patient care.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Hamdan SZ, Bennett A. Autism-Friendly Healthcare: A Narrative Review of the Literature. Cureus [Internet]. 2024 Jul 8;16(7). Available from: https://www.cureus.com/articles/270015-autism-friendly-healthcare-a-narrative-review-of-the-literature.pdf
2. Mitchell MJ, Newall FH, Sokol J, Williams KJ. Simulation-Based Education for Staff Managing Aggression and Externalizing Behaviors in Children With Autism Spectrum Disorder in the Hospital Setting: Pilot and Feasibility Study Protocol for a Cluster Randomized Controlled Trial. JMIR Research Protocols. 2020 Jun 4;9(6):e18105.
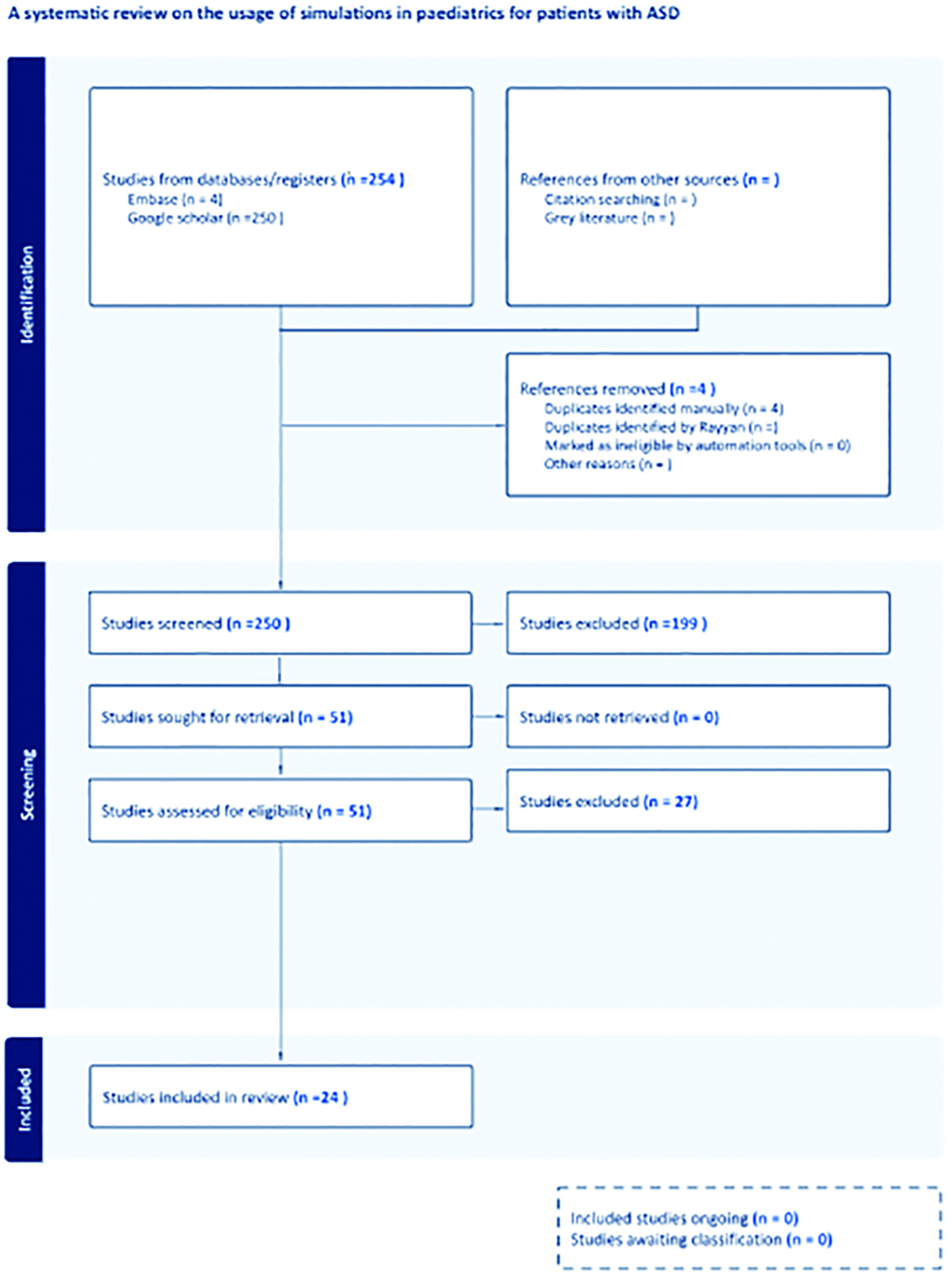
George Dykes 1
[1]
Peripheral venous cannulation is an essential practical skill for undergraduate medical students. The journey towards procedural competence can be challenging and stressful due to infrequent opportunity for practice and fear of failure on real patients. In clinical practice ultrasonography can aid clinicians performing difficult peripheral venous cannulation. Teaching on ultrasound has not previously been widely incorporated into UK medical undergraduate education with cost cited as a significant barrier [1]. The increasingly widespread availability of ultrasound equipment provides an opportunity to give students an introduction to ultrasound whilst simultaneously developing competence and confidence with peripheral venous cannulation. We aimed to develop a cost-effective ultrasound guided intravenous access course for medical students to bring together these two learning requirements.
A pilot course was designed for undergraduate 4th year medical students with prior experience of cannulating approximately 10 patients and with no experience of using ultrasound. Two experienced faculty members led small group sessions for ten students using five ultrasound probes with a focus on hands-on learning. Eight sessions were delivered over two days reaching over 80 students. The three-hour session was divided into ultrasound for beginners (including arterio-venous sonoanatomy) and ultrasound guided cannulation on vascular access models. In order to minimise costs homemade models were used consisting of balloons, turkey steak and gelatine, keeping consumable expenses to under £8 per student.
Post-course feedback was collated to assess the course delivery and its perceived usefulness. 100% of students described the course as “interesting” or “very interesting”, with over 95% recommending for the course to be delivered to other medical students. All students felt the vascular access model was useful for learning the procedure with 95% reporting the course “definitely” increased their confidence with ultrasound guided cannulation. In addition, 58% of students felt more confident with non-ultrasound guided cannulation.
Ultrasound guided peripheral venous cannulation is often perceived as an advanced skill only available to those working in high resource specialties such as anaesthesia. This pilot course has demonstrated that teaching this practical skill to undergraduate medical students using high fidelity simulation is both feasible and highly valued by students. For the majority of students using ultrasound improved confidence with basic cannulation skills possibly through improved procedural spatial awareness and anatomical understanding. Removing the need for commercially available vascular access models allows cost effectiveness and the possibility to scale up the course to a larger body of students.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. McCormick E, Flanagan B, Johnson CD, Sweeney EM. Ultrasound skills teaching in UK medical education: A systematic review. Clin Teach. 2023; 20(5):e13635. doi: 10.1111/tct.13635.
Sabah Hussain 1, Rebecca Ramsay 1, Annabel Copeman 1
[1]
In high-pressure clinical environments, fostering a culture that encourages reflection, learning, and emotional wellbeing is essential. Hot debriefing offers an immediate, structured opportunity for teams to reflect on critical events, strengthen communication, and embed psychological safety into regular practice [1]. This teaching session aimed to educate resident paediatric doctors on the importance of a hot debrief and introduce relevant models that supports cultural transformation by normalising reflective practice.
A multidisciplinary teaching session was delivered to 25 resident paediatric doctors, focusing on the practical application of hot debriefing. The session included a structured approach and a set of practical tools for initiating team-based hot debriefs. Through the use of videos and simulations we were able to embed principles of psychological safety, emotional recognition, and inclusive dialogue. In order to facilitate real-time feedback, gather the thoughts of the resident doctors and enable a collaborative environment we utilised Slido within this session. Pre- and post-session surveys were used to assess changes in experience and confidence, and to identify future training needs. Qualitative comments were collected to capture perceived cultural and emotional impact.
Pre-course data showed that 80% of participants had little or no prior experience with hot debriefing. Following the session, 84% reported feeling moderately or much more confident in asking for a debrief. Additionally, 84% expressed interest in receiving further training on how to lead debriefs. Qualitative feedback consistently highlighted a shift in attitude toward team communication and support, with participants valuing the normalisation of discussing emotional responses. Many viewed the session as a catalyst for change, helping to challenge existing cultural norms around silence after difficult events and learning from these.
The introduction of hot debriefing as both a concept and a structured practice contributed to a visible cultural shift within clinical teams. Rather than treating debriefs as optional or exceptional, the session repositioned them as integral to team-based care and resilience. By normalising immediate reflection, hot debriefing supports a compassionate, safety-oriented culture that prioritises emotional well-being alongside clinical outcomes. As healthcare organisations aim to address burnout, improve safety, and foster inclusive team dynamics, scalable interventions like hot debriefing can serve as foundational tools to drive cultural transformation from the ground up [2]. Going forward, we would like to deliver these sessions to all paediatric resident doctors and incorporate more simulation-based education within it to enhance a team culture that supports open communication, compassion, and continuous learning.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Leemon M, et al. The impact of debriefing on paediatric trainees. J Paediatr Educ. 2016;12(3):45–50.
2. Smith J, Doe A. Implementing debriefing practices in emergency departments. Clin Simul Nurs. 2019;15(4):200–6.
Gemma Cox 1, Charlie Davis, Ben Hester, Laura James
[1]
Elective withdrawal of non-invasive ventilation (NIV) in motor neurone disease (MND) is recognised as impactful on clinician’s mental health and well-being, presenting complex ethical, legal, and emotional challenges [1,2]. To reduce the emotional burden on staff, we designed and delivered an immersive simulation-based training day aimed at improving clinical confidence in managing elective NIV withdrawal and its holistic challenges.
Nine Palliative care registrars participated in a structured educational intervention combining classroom-based teaching with immersive simulation scenarios reflecting real-world cases. Participants self-rated their confidence in four key domains—ethical understanding, legal knowledge, practical implementation, and communication—at three intervals: before the session, after the classroom component, and post-simulation.
The simulation occurred in a high-fidelity immersive environment reflecting a domiciliary setting enhanced by high quality acting to support challenging conversations. A manikin was used which can display eye blinking, carotid pulse, chest wall movement, radial pulse, sub cutaneous administration of medicines.
Baseline confidence of “Not confident at all” was lowest in practical implementation (57%) and communication (14.3%). After the classroom session, “very confident” responses rose to 83.3% in ethical and 75% in legal domains, while practical and communication confidence saw modest increases. Following simulation, confidence in ethical, legal, and practical domains rose to 88.9%. Communication skills confidence rose to 66.7%, a 52.4 percentage point increase from baseline (Figure 1).
This blended educational approach—combining theoretical teaching with immersive simulation—significantly enhanced participant confidence in managing the elective withdrawal of NIV in MND than just classroom-based teaching alone. Simulation was particularly effective in reinforcing practical and communication skills, underlining its value in preparing clinicians for ethically complex, emotionally charged scenarios. It is hoped that this experience will positively impact clinician’s mental health and well-being for future ‘real life’ experiences.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable
1. Cox G, Davis C, Woodley J. A qualitative exploratory study into medical, nursing and allied health professional experiences of elective withdrawal of non-invasive ventilation in a motor neurone disease cohort. J Eval Clin Pract. 2024 Oct 18.
2. Association for Palliative Medicine (2024) Withdrawal of Assisted Ventilation at the Request of a Patient with Motor Neurone Disease: Guidance for Professionals.
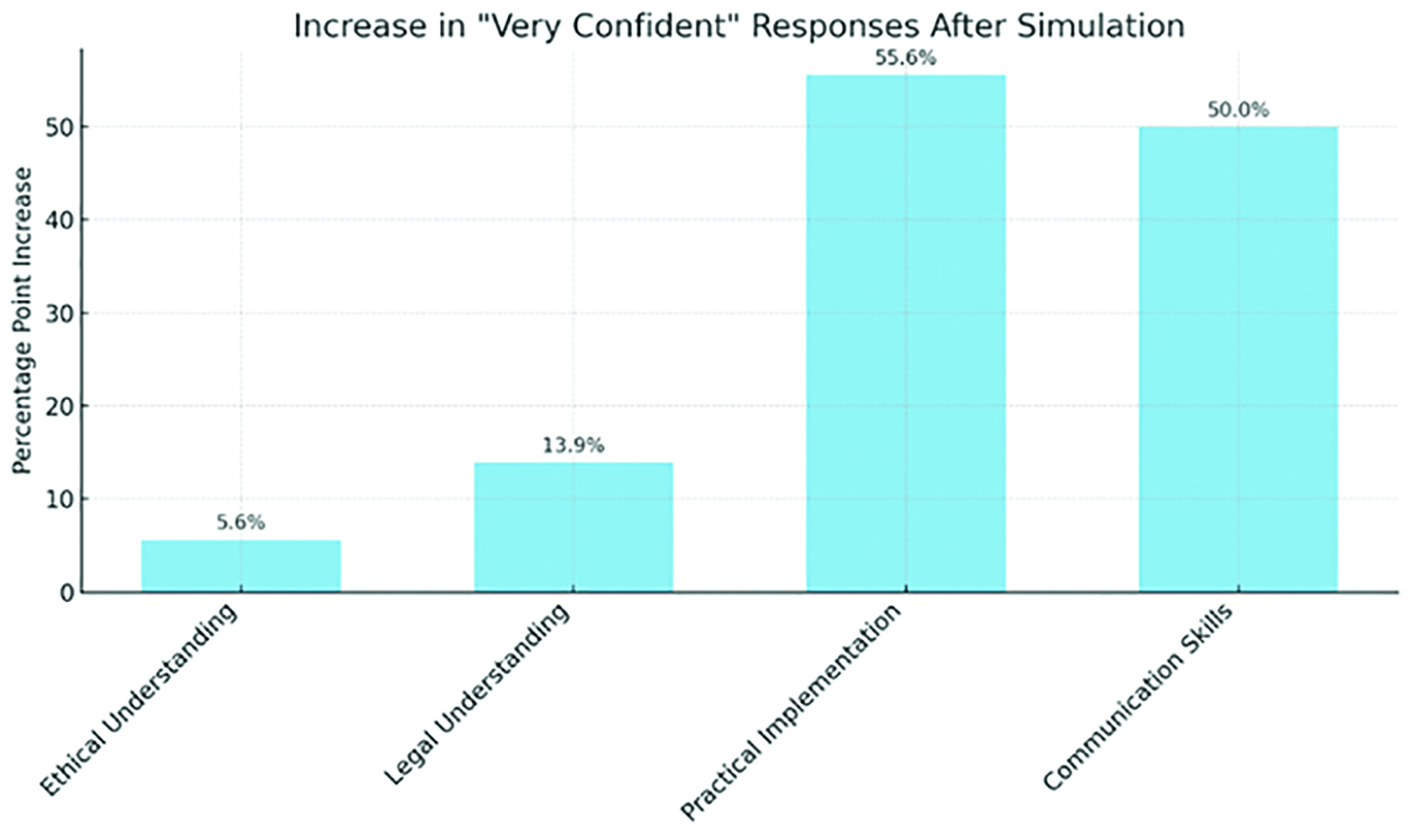
Ruth Willmott 1, Beth Tennant 1, Lydia Fletcher 1, Wint Mon 1
[1]
Patient involvement in medical education has traditionally been passive, often limited to experiential learning in clinical settings or illustrating clinical conditions, limiting the potential for impactful learning experiences [1]. Thus, research to date on their involvement in simulation education is sparse, with greater emphasis placed on the role of the simulated patient, a professionalised role subject to detachment from authentic patient experiences. In conditions such as obesity, where stigma and communication challenges often exist [2], a deeper understanding of the lived experience of our patients is vital to patient-centred care. Our Bariatric Emergencies Simulation Training (BEST) course reimagines patients not as passive subjects but as active partners in simulation education. Through co-production, we sought to authentically integrate the patient voice and demonstrate its value in shaping effective healthcare education.
BEST is a one-day simulation-based course bringing together anaesthetic and surgical residents, along with theatre and recovery staff. By design, it recognises the value of simulation in two ways: to rehearse the recognition and management of complications related to bariatric surgery, and to critically reflect on communication strategies regarding obesity-related risks and weight stigma. To ensure authenticity and impact, we adopted a co-production model involving an expert patient – an individual with lived experience of bariatric surgery – throughout the design and delivery process. As a result, the scenarios were grounded in their lived experience; they voiced the manikin during the simulations to enhance the authenticity of patient interactions, and participated in debriefing, alongside experienced facilitators and subject matter experts.
Data was collected via an anonymous pre- and post-course survey using Microsoft Forms. Participants reported that the most valuable aspect of the expert patient’s involvement was learning about appropriate language use (57%) and gaining a better understanding of the patient experience (29%). Overall, 63% of participants indicated they were ‘very satisfied’ with the course, while the remaining participants were ‘satisfied’.
As healthcare moves towards person-centred, collaborative models where patients are recognised as experts in their own care [3], educational approaches must evolve. BEST demonstrates how co-production in simulation can bridge the gap between assumed knowledge and lived experience, highlighting the value of expert patient involvement in educating healthcare providers on the complexities of communication and person-centred care in the context of obesity. By involving patients as education partners, we cultivate a culture of empathy and improved communication, ultimately impacting patient care and safety.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Dijk SW, Duijzer EJ, Wienold M. Role of active patient involvement in undergraduate medical education: a systematic review. BMJ Open. 2020 Jul 27;10(7):e037217.
2. Fulton M, Dadana S, Srinivasan VN. Obesity, Stigma, and Discrimination. 2025.
3. Kaba R, Sooriakumaran P. The evolution of the doctor-patient relationship. International Journal of Surgery. 2007 Feb;5(1):57–65.
Denise Brown 1, Malcolm Smith 2, Biju Jose 3, Amy Kennedy 4
[1]
[2]
[3]
[4]
The UK Foundation Programme Curriculum [1] requires understanding of patient safety and incident management. While the NHS Patient Safety Incident Response Framework [2] advocates a systems-based approach, training often emphasises non-technical skills without deeper exploration of system-wide factors. To address this gap, the Simulation Team at University Hospitals of North Midlands (UHNM) integrated human factors teaching into one of the three simulation sessions they provide for Foundation doctors. The goal was to equip trainees with the tools to analyse incidents and appreciate how changes to the wider work system can affect patient safety.
We created a course to enhance Foundation doctors’ understanding of human factors, with a focus on the SEIPS (Systems Engineering Initiative for Patient Safety) model [3] and Safety-II thinking. A mix of twelve Foundation year one and two doctors participated in each session, which included two interactive workshops and five simulation scenarios.
- Workshops: The first introduces systems engineering and Safety-II principles; the second focuses on the practical application of the SEIPS model.
- Scenarios: These span various clinical situations-from discharge errors to never events-each is designed with a specific human factor learning outcome. Debriefs emphasise how work systems might be improved rather than focusing on individual performance, differentiating this session from other sessions that consider clinical management.
To date, 107 of 160 Foundation doctors have participated, with full attendance by July. Preliminary feedback from those that have attended shows:
100% of participants reported understanding how to apply a systems-based approach to incident investigations.
100% felt confident using the SEIPS model to evaluate system changes.
100% stated the session would influence their clinical practice.
Qualitative feedback indicated increased awareness of human factors and their influence on patient safety.
The session received an average rating of 4.92 out of 5.
Detailed analysis will be conducted upon course completion.
This simulation-based approach centred around patient safety scenarios has enabled trainees to analyse errors through the lens of system design rather than individual fault. It has fostered reflective dialogue on patient safety issues and how work systems can be improved. It has highlighted the need for a stronger training of human factors amongst Foundation trainees. A follow-up of the longer-term impacts is planned for the current Foundation Year 1 doctors when they return for simulations in Foundation Year 2.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. UKFP. UK Foundation Programme Curriculum 2021. 2021. Available from: https://foundationprogramme.nhs.uk/curriculum/
2. NHS England. Patient Safety Incident Response Framework 2022. London, NHS England and NHS Improvement. 2022. Available from: https://www.england.nhs.uk/wp-content/uploads/2022/08/B1465-1.-PSIRF-v1-FINAL.pdf
3. Carayon P. Sociotechnical systems approach to healthcare quality and patient safety. Work. 2012;41 Suppl 1:3850–3854.
Joyita Saha 1, Bethany Turner 2, Amber Orr 2, James Turnbull 2
[1]
[2]
New graduate doctors often feel unprepared for decision making and communication in acute situations [1], and undergraduate medical students have limited exposure to acutely unwell children to develop these skills in a paediatric setting. Simulation-based education (SBE) offers learners a chance to practise these skills in a safe, controlled environment without risking patient safety. By replicating real-life scenarios, SBE enhances both technical and non-technical competencies, including decision-making, teamwork, and communication [2]. This project aimed to assess changes in undergraduate medical students’ self-reported confidence before and after participating in a simulation-based teaching session on paediatric emergencies.
A paediatric simulation-based teaching session was designed and delivered to two groups of six undergraduate medical students on their paediatrics placement between January and March 2025. Prior to the session, students completed a questionnaire rating their confidence on a 1–5 Likert scale in four domains: managing an unwell child, recognising when to escalate care, clinical reasoning, and handover communication. The session began with a briefing, discussion of intended learning outcomes, and introduction to the simulation environment and mannequin. Following this, students participated in three paediatric simulation scenarios in pairs, while their peers observed from a separate room. Each scenario was followed by a structured debrief involving all students. Upon finishing the session, students completed a post-session questionnaire reassessing the same four domains. Additionally, they were asked to rate the perceived usefulness and relevance of the session and provide feedback.
Of the 12 participants, only four (33%) had encountered an acutely unwell child during clinical placement. Students’ confidence significantly improved when comparing pre-session and post-session mean self-reported confidence levels across all four domains: managing an unwell child (pre-session 1.7, post-session 3.5, p<0.001), recognising when to escalate (pre-session 2.6, post-session 4.0, p=0.003), clinical reasoning (pre-session 2.4, post-session 3.7, p=0.001), and handover communication (pre-session 2.1, post-session 3.8, p<0.001). Students also rated the session as highly useful (mean=5.0) and relevant (mean=5.0) to their medical education.
Simulation-based teaching significantly improved medical students’ confidence across all assessed domains. These findings highlight the value of simulation as a supplement to clinical experience in undergraduate medical education. By offering a safe environment to practise critical skills, SBE enhances clinical reasoning and helps develop competent, confident future doctors.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable
1. Monrouxe LV, Grundy L, Mann M, et al. How prepared are UK medical graduates for practice? A rapid review of the literature 2009–2014. BMJ Open. 2017;7:e013656.
2. McGaghie WC, Issenberg SB, Petrusa ER, Scalese RJ. A critical review of simulation-based medical education research: 2003–2009. Med Educ. 2010;44(1):50–63.
Meherun Rahman, Emma Vickers, Nicola Watts, Louise Harmer
[1]
[2] Warwick Medical School,
Medical students repeatedly report a lack of confidence in their paediatric knowledge and clinical skills, which can adversely affect their learning experience [1]. Given the complexity and nuances of Paediatrics, coupled with limited placement exposure, creative and accessible teaching interventions are imperative [2]. This service evaluation aimed to assess whether delivering a dedicated Paediatric Knowledge and Skills Session (PKSS) early in training could improve student confidence and knowledge, while remaining sustainable and easily replicable.
This service evaluation was created and delivered by a multi-disciplinary team of clinical educators and immersive technology experts at a teaching hospital. The PKSS included gamification, simulation, interactive quizzes, and lecture-based teaching within a single-day, providing an engaging yet challenging experience. It was designed with sustainability in mind, using existing departmental manikins, donated clinical equipment (e.g., non-rebreather masks, blood bottles), and recycled or reusable materials for games with no ongoing costs. Quizzes were delivered electronically to minimise paper use. Sessions were facilitated by educators experienced in paediatrics or simulation, requiring minimal staff training resources. Students completed digital pre- and post-session MCQs, self-rated confidence surveys, and qualitative feedback forms.
Of the 28 participating students, data from 22 were analysed due to incomplete or unmatched responses. The 22 students showed significant improvement in confidence across all items, with 5 questions reaching extreme statistical significance (p <0.0001). Knowledge scores improved in 6 of 8 MCQs, reaching a statistical significance (p ≤0.0423). Simulation performance improved between attempts, as evidenced by checklist assessments. Qualitative feedback described the PKSS as an informative and enjoyable day, with students requesting more sessions like it.
The PKSS demonstrated significant improvements in both confidence and knowledge, as well as overall enhancement in simulation performance. Importantly, the session was delivered in a low-cost, sustainable format using existing resources, donated materials, and minimal paper. Once developed, it required minimal upkeep, making it an ideal teaching model for other institutions. While long-term impacts of the PKSS need to be reviewed, current results indicate that teaching specialist disciplines like Paediatrics can be revolutionised into an impactful, creative and environmentally conscious model in healthcare education.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Weinstein A, MacPherson P, Schmidt S, et al. Needs assessment for enhancing pediatric clerkship readiness. BMC Med Educ. 2023;23:188. doi: 10.1186/s12909-023-04167-7.
2. Morrissey B, Jacob H, Harnik E, Mackay K, Moreiras J. Simulation in undergraduate paediatrics: a cluster-randomised trial. Clin Teach. 2016;13(5):337–342. doi: 10.1111/tct.12442.
Clinical Simulation & Immersive Technologies Team
Ragittaran Jayakumar, Ren Estacio 1, Muniswamy Hemavathi
[1]
This teaching simulation aims to improve the team working and leadership skills of different members of the medical team in an acute scenario and allows them to understand the direct roles of each individual team member.
To assess the effectiveness and value of multi-professional simulation in increasing the awareness of roles within an interprofessional setting. To assess if multi-professional simulation increases confidence levels when managing emergency scenarios in a team-based setting.
The simulation consisted of six varied emergency scenarios common to the Accident and Emergency department, where the scenario would involve care of Addisonian Crises, Euglycaemic Diabetic Ketoacidosis, ACS leading into Heart Block etc.
The participants were all at varying levels of training and roles from Advanced Practitioners, Nurses, Senior and Junior Clinical Fellows. Nursing teams would be asked to do an initial assessment of a high-fidelity manikin, refer to their seniors and slowly the full medical team would be involved in handling the patient’s care.
Once all scenarios were completed, we collected one minute feedback forms from all participants which investigated how our simulation differed from traditional simulation provided in their training, what they learnt for their own clinical practice and the roles of other professions.
Out of the ten candidates, only two of them had previous simulation experience. They reported that the simulation blended acute scenarios well with hospital pathways and therefore felt realistic to their practice. Other comments praised the interactive elements and covering different hospital protocols.
Candidates received specific personal learning objectives tied to individual learning, but a highlight was that eight out of ten (80%) candidates felt that this learning improved their teamworking and leadership skills in emergency situations, with emphasis on communication between members of the team, their expertise and limitations.
High-fidelity multi-professional simulation enhanced awareness of team members’ roles and collaborative dynamics. Participants reported improvements in communication and confidence in emergency care delivery.
Broader implementation and further evaluation are needed to assess its impact across different healthcare settings.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
Emily Thorley 1
[1]
LLEAP (Laerdal Learning Application) by Laerdal Medical is the software used to control our interactive manikins during simulation. External courses are not specific to our technology, so the need for training and opportunities for practice in this area were evident. Since the COVID-19 pandemic, much training has moved online. The use of the cognitive apprenticeship model described by Collins, Brown and Newman [1] has proven to be effective in the delivery of online faculty development programs [2]. The aim of this blended learning approach was to increase the confidence of new faculty, using the same model to provide online software training followed by hands-on practice.
The digital aspects of training were two-fold; a screen-recorded video created using Microsoft Stream was distributed to relevant faculty via email, and an interactive screenshot was accessed through an online tool called ThingLink. The video covered features of the software relevant for our Foundation doctor simulation days. The interactive screenshot provided an opportunity for learners to explore at their own pace, answering questions along the way to articulate learning and build confidence. In-person training and live supported experience within simulation delivery followed to allow exposure of learners to all six methods described in the cognitive apprenticeship model [1].
After the training was complete, anonymous feedback questionnaires were distributed via Microsoft Forms to four new teaching fellows and six existing members of simulation faculty. This assessed the impact of the additional digital components on confidence and identified areas for improvement.
The questionnaire received seven responses. 86% (six respondents) strongly agreed that blended learning was a good approach to this training and that they felt more confident using the LLEAP software after watching the video.
Open response questions revealed that using digital tools added interactivity to the learning, aided learning at their own pace and provided a source of information for reference or troubleshooting. Suggested improvements included making the cursor more visible in the video and to apply this type of training to other aspects of facilitation.
Addition of digital resources prior to hands-on training improved the confidence of new faculty in running the manikin during simulation and value for existing faculty was also demonstrated. Going forwards, these resources, with a few adjustments, will be used for the next intake of new faculty. Similar techniques may prove useful for other training such as introduction of the manikin and its functions.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable
1. Collins A, Brown JS, Newman SE. Cognitive Apprenticeship: Teaching the Crafts of Reading, Writing and Mathematics. In: Resnick LB (editor) Knowing, Learning and Instruction [Internet]. United Kingdom: Routledge; 1989. p.453–494. Available from: https://doi.org/10.4324/9781315044408-14.
2. Eltayar AN, Eldesoky NI, Khalifa H, Rashed S. Online faculty development using cognitive apprenticeship in response to COVID-19. Medical Education [Internet], 2020 Jul [cited 2025 April 24]; 54 (7): 665–666. Available from: https://doi.org/10.1111/medu.14190.
I would like to thank the Postgraduate Medical Education Team at The Shrewsbury and Telford Hospitals Trust for their support in the delivery of this training.
Emily Thorley 1, Karen Bryan 1, Amy Ingham Farrow 1, Aung Phyo Naing 1, Steven Mansell 1
[1]
The 2021 document “Modern ward rounds: Good practice for multidisciplinary patient review” recommends simulation as a useful strategy for training relating to ward rounds [1]. Existing ward round simulation predominantly targets undergraduates, or foundation doctors during induction, with limited integration across different grades of medical training. We hoped to take this opportunity to engage multi-disciplinary and cross-grade teams in a more authentic, collaborative learning experience around open communication and building positive working culture.
A half-day, multi-patient simulation event was designed to represent the complexities of ward rounds on an acute medical ward. This three-part session included a pre-brief alongside a period of sharing experiences and good practice, followed by the simulation and subsequent debrief. The ward round simulation comprised a bay of four patients at various stages of their inpatient journey. Foundation Year 1 doctors, senior registrars, consultants, and registered nurses were invited to attend as learner participants to allow development of authentic team dynamics.
Pre- and post- simulation surveys explored attitudes of learners to current ward round practices and what they had learnt from the experience. In total, 91 learners were surveyed across 17 episodes between September 2024 and March 2025.14% were consultants, 65% were resident doctors, 17.5% were nursing staff and the remainder listed their professional title as “other”.
The response was overwhelmingly positive, with 97.7% of 88 learners reporting that the training was “likely” or “very likely” to change their practice. 87.5% would “definitely recommend” the course. Verbal feedback from one ward manager stated that staff who had attended the simulation now realised the value they can add to a ward round.
In the pre-course survey, learners felt ward round effectiveness could be improved through better communication and more consistent multi-disciplinary involvement. Post-course, these feelings were replicated, with learners describing the recognition of a need for assertiveness, feeling more comfortable to challenge more senior colleagues, and to escalate concerns.
We observed that one of the greatest challenges for nurses is the ability to attend ward rounds. We would like to examine the barriers further as we develop the simulation in the coming year.
Learners have appreciated open discussions around the challenges and best practices of ward rounds made possible by the cross-grade and multi-disciplinary nature of this simulation. The diversity of perspectives demonstrated freely in debriefs provides optimism that this culture of mutual respect can be translated more widely into clinical areas.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Royal College of Physicians, Royal College of Nursing. Modern ward rounds: Good practice for multidisciplinary patient review [Internet]. London, Royal College of Physicians; 2021 [cited 2025 April 24]. Page 28. Available from: https://www.rcp.ac.uk/media/t2cplwpv/ward_round_report_0-1.pdf
We would like to acknowledge the important contributions, in particular of Dr. Kevin Eardley (Clinical lead for Simulation) and Sr. Claire Swindell (Practice Education Facilitator), to the development and delivery of the course, alongside the SaTH Postgraduate Medical Education Team. Thanks also to Dr. Gordon Wood (Director of Medical Education) and Dr. Saskia Jones-Perrott (Divisional Medical Director for the Medicine & Emergency Care Division) for their unwavering support in promoting ward round simulation.
Natassia King 1, 2, Andrew Greer 2, Deborah Clark 1
[1]
[2]
Many final-year student doctors report feeling underprepared and lacking in confidence in essential skills for on-call shifts [1]. On-call duties are a core component of foundation training. On-call simulation improves confidence in non-clinical skills such as prioritisation and stress management [2,3].
This project introduced a simulated on-call event for final-year student doctors at the University of Sheffield, aiming to boost confidence in non-clinical skills and preparedness for Foundation Year 1 (F1) on-call responsibilities.
To evaluate the impact of a simulated medicine on-call event on student doctors’ confidence in clinical and non-clinical skills.
23 final-year student doctors from the University of Sheffield participated in a three-part event: group teaching, simulation lab, and hospital-based simulation.
Students completed anonymised pre- and post-event self-assessment questionnaires rating their confidence across seven domains: receiving SBAR handover, providing SBAR handover, prioritisation, stress management, escalation, clinical reasoning, and overall preparedness for F1 medical on-calls. Responses used a 5-point Likert scale (1 = not confident at all; 5 = extremely confident). Scores were analysed using descriptive statistics and Mann-Whitney U analysis. The post-event questionnaire included additional feedback questions.
23 students completed the pre-event survey; 22 completed the post-event survey. 95.5% (21/22) reported increased confidence for medical on-calls; one reported no change.
The domain demonstrating greatest improvement was prioritisation: +2 in median and mode, and the highest mean increase: +1.55. Receiving SBAR handover and stress management increased by +2 in median and mode. Providing SBAR handover, escalation, and on-call preparedness increased by +1 in median and mode. Clinical reasoning remained unchanged in mode and median (score = 3) and had the lowest mean increase: +0.75. Mann-Whitney U analysis showed significant improvement in all domains individually (all p values <0.05), Figure 1. p values for mode (1.5), median (4), and mean (0) were all below the critical value at p<0.05 (8).
The simulation enhanced students’ confidence in core aspects of medical on-call duties. The most notable gains were in the domains of prioritisation, stress management, and providing SBAR handovers. There may be a need for additional interventions to further enhance clinical reasoning skills within this simulation. This study provides good evidence that simulation-based education is a highly effective method of increasing the confidence of student doctors in the skills required for on-call responsibilities.
Some limitations of this study include incomplete data sets, subjectivity of the Likert scale, and a small sample size. Further studies are required to validate findings.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Tallentire VR, Smith SE, Wylde K, Cameron HS. Are medical graduates ready to face the challenges of Foundation training? Postgrad Med J. 2011 Sep;87(1031):590–5. doi: 10.1136/pgmj.2010.115659. Epub 2011 Jun 20. PMID: 21690255.
2. So HY, Chen PP, Wong GKC, Chan TTN. Simulation in Medical Education. Journal of the Royal College of Physicians of Edinburgh. 2019;49(1):52–57. doi: 10.4997/jrcpe.2019.112.
3. Alan M Greenstein, Muniswamy Hemavathi. The bleep experience: preparing new doctors for on-call shifts. Future Healthcare Journal. Volume 7, Issue 1. 2020. Pages 84–85. doi.org/10.7861/fhj.2019-0020. https://www.sciencedirect.com/science/article/pii/S2514664524007914
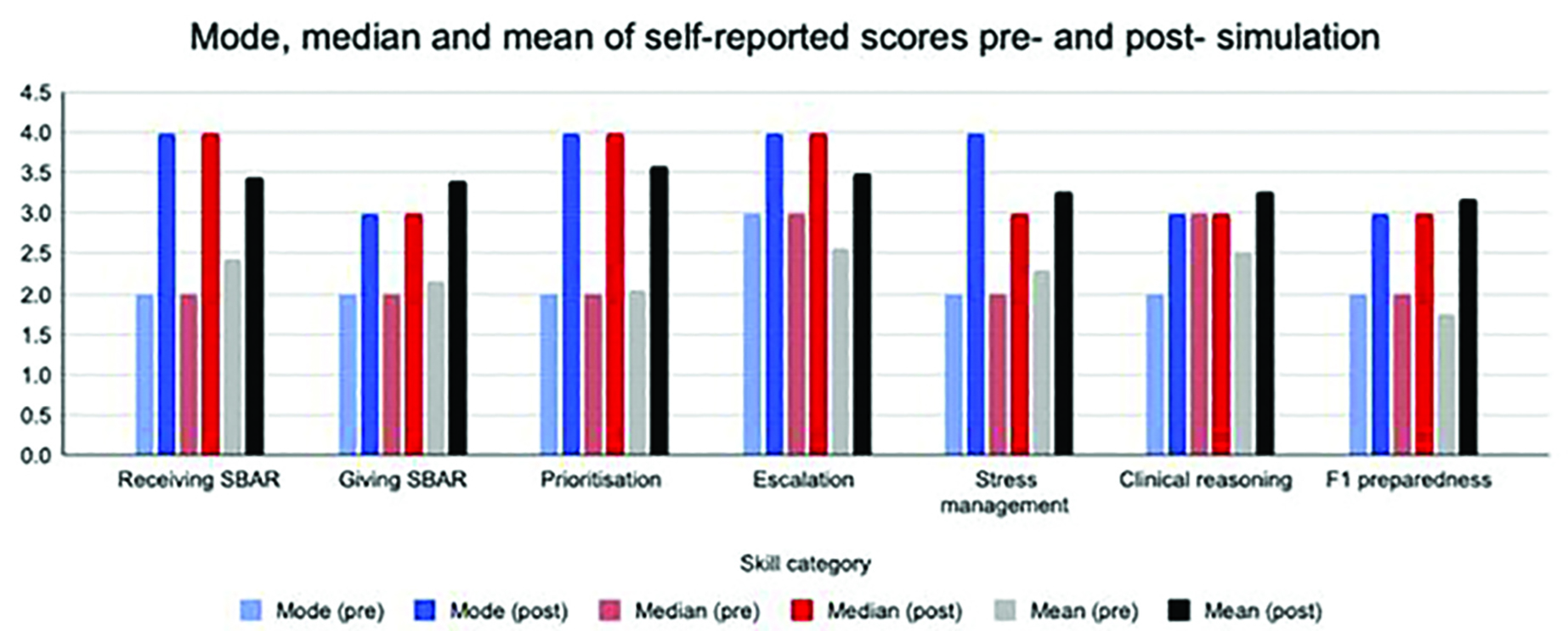
Robyn Stiger 1, Stephanie Mansell 2, 3, Amanda Thomas 4
[1]
[2]
[3]
[4]
On-call respiratory physiotherapy is provided by NHS Trusts for acutely unwell patients outside of normal working hours [1]. Training is provided before undertaking on-call duties. However, many physiotherapists find on-call situations stressful and report a lack of confidence to undertake these duties. Simulation provides a safe learning environment to develop on-call skills, when supported by trained faculty [2]. Access to faculty training is needed [3]. Therefore, a national course was developed for experienced physiotherapists looking to develop their skills as simulation faculty. It was aimed at participants with limited experience as simulation faculty, wanting to develop an on-call simulation provision at their institution.
A team of physiotherapy and simulation faculty experts designed a one-day course. Participants completed all six modules of the national “Becoming Simulation Faculty” E-Learning programme as pre-learning. The course included discussions about educational theories, scenario design, psychological safety and debriefing models. In a round-robin format supported by a mentor, participants ran an on-call scenario (prebrief to debrief), were active participants or observers, and supported a meta-debrief discussion. Quantitative and qualitative data from pre- and post-course questionnaires were collected and analysed.
The course ran three times in England (n=2) and Northern Ireland (NI) (n=1). 66 learners completed the course, from a wide geographical range (Figure 1).
Pre-course findings:
Respondents with no simulation experience as a learner: 35%(England); 77% (NI)
Respondents with no simulation faculty training: 65% (England); 94% (NI)
On-call simulation training being delivered at participant organisation: 67% (England); 12% (NI)
Two main themes about why participants attended the training were generated: “To set up or support an on-call simulation service, and/or to utilise existing simulation resources” and “Build knowledge and confidence in simulation methods (including technology, scenario writing, debriefing, evaluation)”. With a third theme in the England courses: “Collaboration/ sharing best practice/ improving existing services/ standards”.
Post-course findings:
All respondents (89% response rate) rated the course as Excellent (78%) or Good (22%), with positive themes regarding “the practical aspects of the course” and the “peer and experienced faculty discussions”. Participants wanted more training on “scenario writing”, “debriefing” and “advanced methods”.
This course highlighted the need for faculty training within respiratory physiotherapy to meet current simulation standards. It was well received. Further work is needed to explore support for sustainable faculty training in the physiotherapy workforce. Research to explore the impact of this course and on-going workforce training needs within simulation is underway.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. National Institute for Health and Care Excellence (2007). Overview | Acutely ill adults in hospital: recognising and responding to deterioration | Guidance | NICE. [online] Nice.org.uk. Available at: https://www.nice.org.uk/guidance/cg50.
2. Mansell, S.K., Harvey, A., & Thomas, A. (2020). An exploratory study considering the potential impacts of high-fidelity simulation-based education on self-evaluated confidence of non-respiratory physiotherapists providing an on-call respiratory physiotherapy service: a mixed methods study. BMJ simulation & technology enhanced learning, 6(4), 199–205. https://doi.org/10.1136/bmjstel-2019-000444
3. Mansell, S.K, Barnfield, E., Bendall, A., Cork, G., Thomas, A.J, Grafton, K., Eckersley, G., Lewko, A. (2024) Simulation Based Education in pre-registration and postgraduate respiratory physiotherapy: An ACPRC position statement. Journal of the Association of Chartered Physiotherapists in Respiratory Care. 56(3), 46–48. https://doi.org/10.56792/XRTY3249
Two of the courses were commissioned by the Association of Chartered Physiotherapists in Respiratory Care (ACPRC) and one of the courses was commissioned by the HSC Clinical Education Centre in Northern Ireland.

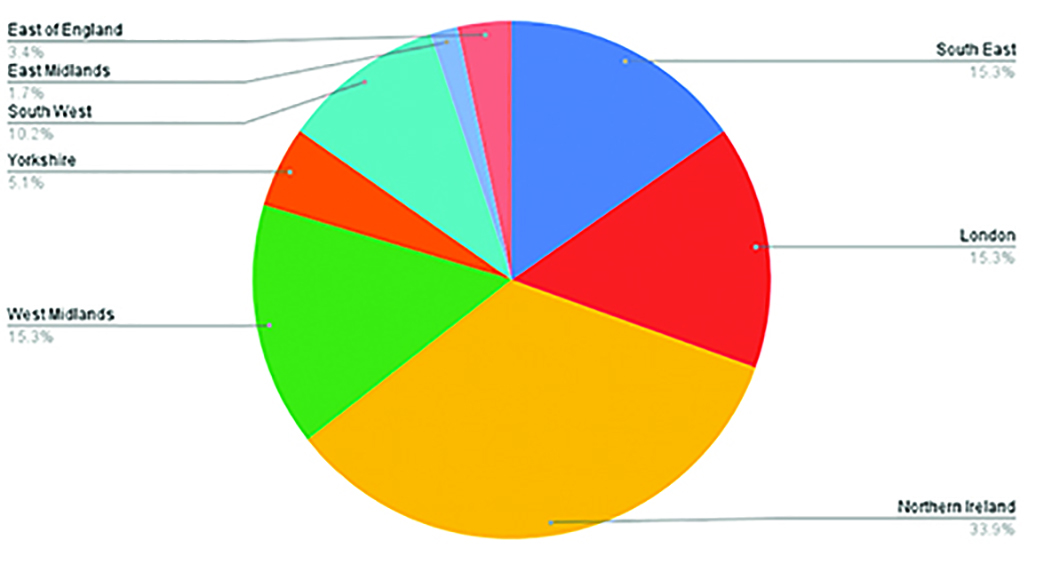
Chart to show regional distribution of course participants across the UK.
Karen Cairnduff 1, Chris May, Sonia Catchpole
[1]
Healthcare professionals need to recognise when someone is approaching the final days or hours of life and be confident to talk about death and dying. Undergraduate training in end-of-life care is inconsistent and students need more support [1]. In the UK, people are experiencing inequitable and suboptimal care before death, with delayed recognition of dying and poor communication resulting in inadequate support for symptoms [2]. Many students will not have a supported experience of caring for someone who is dying, whilst others will experience death frequently. Student nurses report fear, anxiety, and overwhelm about death on placement, feeling vulnerable and unprepared. This can lead to emotional trauma and dropping out before registration [3]. Simulation is used to specifically focus on increasing resilience and decreasing fear of death. A partnership simulation was designed to prepare student nurses for talking about death and dying, to improve end-of-life care experiences.
Student nurses had an extended prebrief which aimed to breakdown the taboo of talking about death. Students participated in four simulation scenarios designed to develop confidence with conversations about death and dying. Scenarios were supported by end-of-life care educators and simulated patient actors to enable realistic conversations about dying. Student led debriefing was facilitated by clinicians with advanced communication skills training.
There was a significant increase in the number of student nurses who felt comfortable to talk with patients and their families/friends about death and dying, with more than 60% of participating students confident to talk about death and dying on their first placement. Students reported a reduction in fear and felt more emotionally prepared for placement. Students were able to apply their learning. One first year student responded, ‘My first death was in week one and I was able to draw directly from the simulation to support the family’. Students were able to recognise and understand dying enough to be able to bring reassurance to patients and families and support themselves and colleagues with the emotional response to death.
End of life care simulation benefits from extended prebrief, partnership with expert clinicians and simulated patient actors to provide a transferable experience. The use of simulated experiences with actors increases realism and provides opportunity to bridge the gap between theory and real world practice. This collaboration is empowering student nurses to recognise dying and be comfortable talking about death; fundamental to person-centred compassionate care at end of life.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. White N, Oostendorp LJ, Minton O, Yardley S, Stone P. Palliative care training in undergraduate medical, nursing and allied health: a survey. BMJ Support Palliat Care. 2022;12(e4):e489–e492. doi: 10.1136/bmjspcare-2019-002025.
2. Marie Curie. Better End of Life Report 2024. Mariecurie.org.uk. 2024 https://www.mariecurie.org.uk/research-and-policy/policy/better-end-life-report
3. Soerensen J, Nielsen DS, Pihl GT. It’s a hard process - Nursing students’ lived experiences leading to dropping out of their education; a qualitative study. Nurse Educ Today. 2023;122:105724. doi: 10.1016/j.nedt.2023.105724.
Sophie Wilcox 1, Christine Walker, Danielle Jamieson
[1]
Working with People with Lived Experience (PLE) can provide a powerful learning experience, and services can be improved by including the expertise of PLE [1]. Motivated by a North East and North Cumbria Integrated Care Board patient safety alert [2], a training session collaborating with PLE of Learning Disability (LD) was developed. The primary objective was to evaluate inclusion of PLE in simulation training, and to explore viability for future expansion. Other objectives were to expand our repertoire of acute care scenarios to include people with existing long-term conditions (including mental health conditions and/ or neuro-developmental conditions), and to develop scenarios requiring professionals to individualise their communication approaches to the person.
A novel training session for foundation doctors was developed, using actors from ‘Northern Stars’ - a local performing arts company for people with LD. Actors met our simulation team for pre-briefing, tour of the simulation facility and received scenario scripts ahead of planned training dates. Each training session included an introductory plenary for learners, which covered communication, LD safety themes and pre-briefing. Subsequently, learners split into groups to undertake simulation activities. A high fidelity scenario (a patient with abdominal pain) with learning outcomes on communication, assessing pain and diagnostic overshadowing, ran in parallel with a simulated role-play (a patient with head injury requiring CT scan) with learning outcomes on explanation of investigations and making reasonable adjustments.
31 foundation doctors participated in training lasting 2 hours. There were significant improvements in learner rated confidence and knowledge following the training (Figure 1). Themes from narrative feedback included intentions to change future practice such making use of ‘hospital passports,’ Makaton (signs and symbols communication method) and adjusting communication style. Participants also commented on the training’s uniqueness (many having received little prior training on the topic.) Actors reported high levels of satisfaction with pre-briefings and understanding of the training’s purpose. All felt content during the session, and all were highly satisfied it was useful for the learners. Some actors also reported benefits on their own wellbeing.
Collaborating with people with lived experience of LD was successful; training proved very effective for learners and feasibility was proved for future expansion. There were also unintended positive outcomes for actor participants. We plan to run the training annually as part of Foundation Program training, and to expand to other staff groups.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. The power of lived experience to enhance health, World Health Organisation, 2022, https://youtu.be/8I4wA52BPGU
2. NENC ICB Learning Disability safety alert NENCSSA1, August 2024
Acknowledgement to Northern Stars performing arts
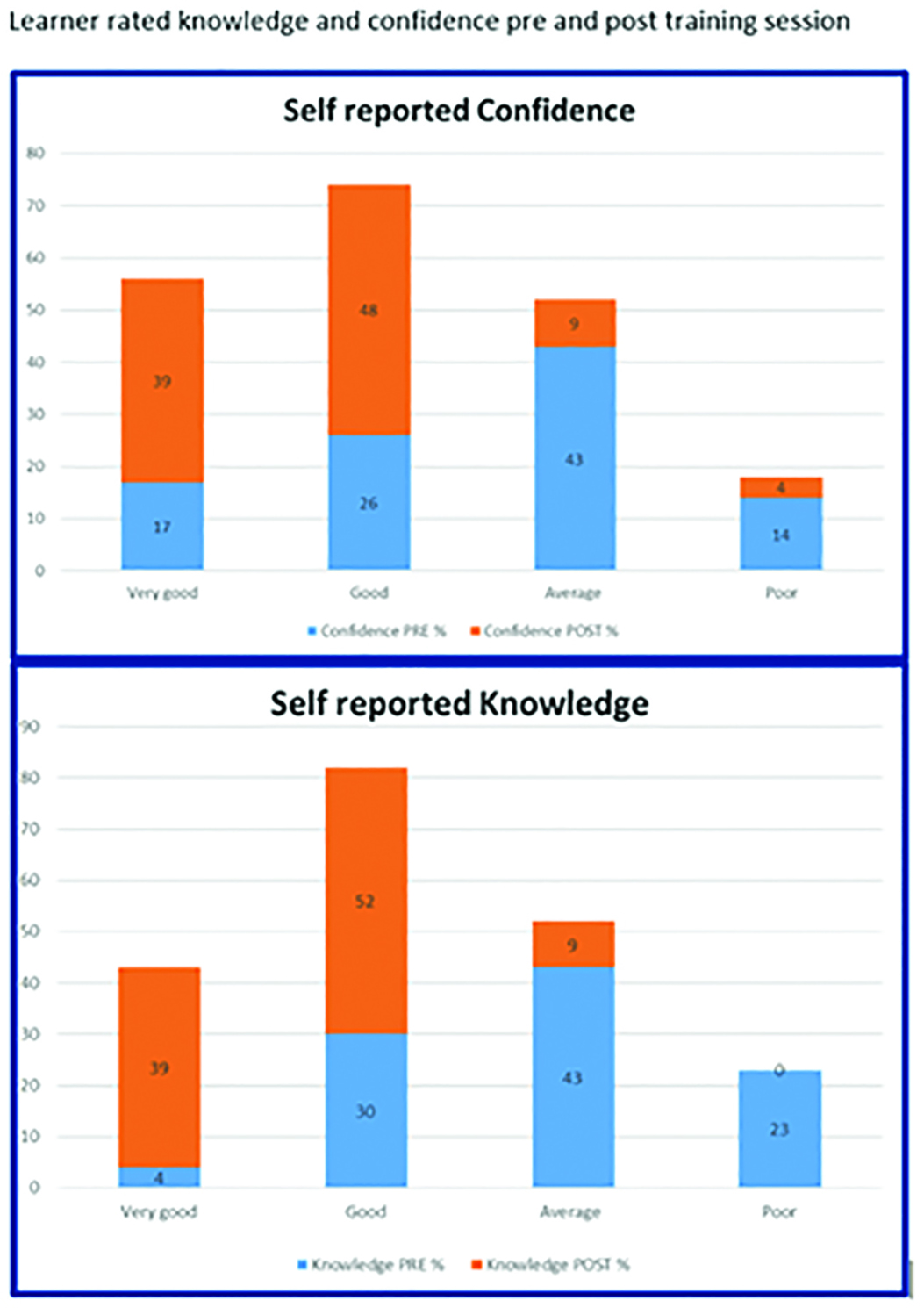
Sophie May 1
[1]
Effectively training healthcare professionals for complex elderly care is vital but often hindered by simulation costs. This project demonstrates a high-impact, low-fidelity simulation escape room designed for interprofessional groups of urgent care practitioners (nurses, paramedics). We aimed to enhance critical thinking, teamwork, and problem-solving by focusing on accessible, engaging pedagogical design incorporating gamification [1] and Visual, Aural, Read/Write, Kinesthetic (VARK) principles, demonstrating impact and creativity within resource constraints.
A structured design process, involving subject matter experts (SME), aligned escape room puzzles with elderly care learning objectives (falls, medication, psychological assessment). The design intentionally integrated VARK learning styles and gamification principles to maximise engagement. AI tools aided development-phase scenario refinement. This low-fidelity simulation was implemented with nurse and paramedic participants undertaking a minor illness course between September 2024 and April 2025. A mixed-methods evaluation used pre/post questionnaires primarily assessing confidence and preparedness, alongside qualitative feedback exploring the learning experience and impact on collaboration. Data was collected in March 2025.
The low-fidelity, design-centric approach proved highly effective. Quantitative data confirmed uniformly high participant engagement (rated 4 or 5/5). Qualitative feedback revealed the simulation was highly enjoyable compared to traditional methods, with participants particularly valuing the problem-solving aspects inherent in the gamified design. Participants reported significant increases in confidence managing complex elderly care scenarios, with 75% stating they felt more prepared to manage elderly falls patients’ post-simulation. Further qualitative data suggested increased confidence in applying key concepts and skills, alongside improved interdisciplinary communication, teamwork, and appreciation for collaborative problem-solving, directly addressing cultural aspects of healthcare teams.
This study confirms that impactful simulation, fostering creativity and cultural competence in healthcare teams, does not necessitate high-fidelity setups. By prioritising robust pedagogical design (VARK, gamification) and co-production principles (SME collaboration), effective, engaging, and accessible low-fidelity simulations can be developed. The strong positive outcomes related to participant engagement, confidence, self-reported preparedness for practice, and improved teamwork and communication [2] demonstrate the simulation’s value. This pilot provides a scalable, resource-conscious model for interprofessional workforce development in specialized areas like elderly care. Ongoing refinement based on feedback continues. This approach strongly aligns with the need for creative, co-produced simulations that deliver measurable impact
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1.van Gaalen AEJ, Brouwer J, Schönrock-Adema J, Bouwkamp-Timmer T, Jaarsma ADC, Georgiadis JR. Gamification of health professions education: a systematic review. Adv Health Sci Educ Theory Pract. 2021;26(2):683–711. doi: 10.1007/s10459-020-10000-3.
2. Keskın G, Edeer AD. Effectiveness of interprofessional simulation-based education programs to improve teamwork and communication for students in the healthcare profession: A systematic review and meta-analysis of randomized controlled trials. Nurse Educ Today. 2023;120:105650. doi: 10.1016/j.nedt.2022.105650.
Harriet Welch 1, Elinor Carlisle 2, Sarah Burgess 3
[1]
[2]
[3]
Uterine inversion is a rare but life-threatening obstetric emergency, with its precise incidence remaining unclear [1]. A Canadian case series by Baskett suggests an incidence of 1 in 3,127 deliveries [2]. Associated with considerable morbidity and mortality, prompt recognition and management are essential to improving maternal outcomes [1]. Given its rarity, exposure to this emergency may not occur until later stages of clinical training. We aimed to develop a skills-based session using low-cost simulation models to support obstetric trainees in managing acute uterine inversion and associated postpartum haemorrhage (PPH).
Four handmade uterine models were constructed from a mixture of felt, thread, velcro, cardboard, and wool. They represented key scenarios: inversion with adherent placenta, manual removal of placenta (MROP), atonic uterus for balloon tamponade, and a softly stuffed uterus for brace suture placement. Each model was integrated into a part-task pelvic trainer and used in a one-hour simulation session as part of an obstetric emergencies training day. Trainees (ST1–ST7) participated in small groups, facilitated by a registrar and consultant Obstetrician. The session included deliberate practice, structured discussions, and additional learning materials. Trainees completed all steps of uterine inversion management, MROP, and surgical control of PPH.
Feedback was obtained from 15 participants (n=15). 93.3% (n=14/15) rated the uterine inversion and MROP session as excellent and appropriate to their training level. Confidence levels, measured on a 5-point Likert scale (1= not at all confident to 5 = completely confident), increased from a pre-session mean of 3.1 to 4.2 following the session. Post-session, 87% (n=13/15) reported being fairly or completely confident, compared to 40% (n=6/15) beforehand. Similarly, 80% (n=12/15) rated the PPH surgical skills component as excellent and suitable for their training level. Confidence levels rose from a mean of 2.9 pre-session to 4.1 post-session, with 80% (n=12/15) feeling fairly or completely confident post-session, again up from 40% (n=6/15).
This low-cost, low-fidelity simulation, supported by expert facilitation, enabled participants to practice the management of a rare but critical emergency using a stepwise approach. Trainees across all grades reported improved confidence. While effective, the fabric models limited hydrostatic demonstration of the O’Sullivan technique. Future versions of the models will include enhanced anatomical features such as vasculature and adnexa to better simulate surgical procedures, including Huntington’s manoeuvre and emergency hysterectomy. Overall, this session achieved its educational objectives, was well received, and offers a reproducible model for future training.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Bhalla R, Wuntakal R, Odejinmi F, Khan RU. Acute inversion of the uterus. The Obstetrician & Gynaecologist. 2009;11:13–18. Available from: https://obgyn.onlinelibrary.wiley.com/doi/10.1576/toag.11.1.13.27463#b6
2. Baskett TF. Acute uterine inversion: a review of 40 cases. J Obstet Gynaecol Can. 2002;24(12):953–956. Available from: https://pubmed.ncbi.nlm.nih.gov/12464994/
Ambyr Reid 1, Paul O’Hara 1, 2, Paul O’Connor 1
[1]
[2]
Ultrasound (US) guided, or Point of Care Ultrasound (POCUS) procedures are increasingly commonplace in healthcare. These procedures improve accuracy and benefit patient safety [1]. Simulation provides a safe environment for healthcare providers to learn how to use the US probe and carry out different surgical or medical interventions such as a kidney biopsy. An innovative US compatible model for kidney biopsies was created out of mixed materials using Aqueous Dietary fibre and Antifreeze Mix (ADAM) Gel [2], a porcine kidney and porcine muscle and skin.
The model was created after two months of trialling different formulations of ADAM Gel, which was made from psyllium husk, anti-foam, propylene glycol and water. A porcine kidney was situated between two layers of ADAM Gel and a final layer of porcine muscle with skin attached was positioned on top. Both fresh and frozen kidneys were trialled. It was found that the kidneys that were frozen immediately after harvest and thawed before use yielded much better visual results under US in comparison to the fresh kidney used a day after harvest. Parts of the kidneys internal structures were well defined under ultrasound to assist in accurate identification of anatomical landmarks. The biopsy needle could be inserted through the layers and a tissue core, with visible glomeruli, was collected from the kidney. This could then be viewed under a microscope for diagnostic purposes.
The models were used at a national nephrology conference in Ireland. The mean learner (n=10) rating of the quality and performance of the models was 9.6 out of 10. The qualitative feedback on the models were that they were ‘very realistic’, ‘easy to use’ and that completing the procedure felt like a ‘true to real life experience’.
In summary, ADAM Gel allowed for the creation of a realistic synthetic base for learning how to carry out US guided procedures. It can be used alongside animal/biological tissue or other synthetic materials for a variety of different medical interventions and treatments. The ability to take tissue samples from the model means the procedure can be followed through up to diagnostic level rather than ending at the patient care level.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Hashim A, Tahir MJ, Ullah I, Asghar MS, Siddiqi H, Yousaf Z. The utility of point of care ultrasonography (Pocus). Annals of Medicine and Surgery. 2021 Nov;71:102982. doi: 10.1016/j.amsu.2021.102982.
2. Willers J, Colucci G, Roberts A, Barnes L. 0031 adamgel: An economical, easily prepared, versatile, self repairing and recyclable tissue analogue for procedural simulation training. Prize poster presentations. 2015 Nov; doi: 10.1136/bmjstel-2015-000075.66.
Amna Mahmood 1, Ahoane Qureshi 1, Cheryl Muir 1
[1]
Human factors are essential to patient safety and effective clinical practice, yet traditional teaching methods often struggle to engage multidisciplinary teams in a practical and collaborative manner. Escape rooms are increasingly recognised as a didactic tool that supports active learning, problem-solving, and the development of key skills such as teamwork and communication [1]. As part of the Skills and Simulation Team’s Open Days at University Hospitals Birmingham (Heartlands, Queen Elizabeth, and Good Hope), an interprofessional escape room was developed as a novel, recreational learning activity. It aimed to bring together clinical and non-clinical staff in a high-pressure, team-based environment to reflect on human factors concepts through immersive gameplay.
Participants formed interprofessional teams to complete an escape room comprising sequential puzzles embedded with clinical and human factors challenges. Tasks included anatomy-based codebreaking, the simulated management of a never event, and deciphering visual and riddle-based clues. The scenarios targeted core non-technical skills such as communication, situational awareness, prioritisation, and escalation. Approximately 34 staff members participated, including nurses, midwives, doctors, students, technicians, and administrative staff. The escape room was grounded in constructivist principles, promoting experiential learning, collaborative problem-solving, and reflection. Participant feedback was collected via structured questionnaires to assess perceived impact and engagement. To enhance motivation and foster a sense of friendly competition, a leaderboard displaying team names and completion times was maintained outside the room.
Participants (n=34) rated the escape room experience highly across all domains using a 0–10 Likert scale. The activity was found to be engaging and enjoyable (mean=9.59, SD=0.76) and promoted effective teamwork and collaboration (mean=9.65, SD=1.06). Objectives and instructions were perceived as clear (mean=8.88, SD=1.26). Participants also felt that the exercise encouraged critical thinking and problem-solving skills (mean=9.56, SD=0.83). Overall enjoyment was rated highly (mean=9.06, SD=1.59). Completion times ranged from 14 to 38 minutes. Many noted that the experience facilitated critical thinking and decision-making under pressure. The format was praised as accessible, well-organised, and suitable for a wide range of professional backgrounds and experience levels.
The interprofessional escape room proved to be an engaging, low-cost educational tool that effectively promoted human factors awareness, teamwork, and critical thinking. Its success highlights the potential for integrating gamified, simulation-based approaches into wider healthcare education, supporting a culture of safety and collaboration across diverse staff groups.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Taraldsen LH, Haara FO, Lysne MS, Jensen PR, Jenssen ES. A review on use of escape rooms in education – touching the void. Educ Inq. 2022;13(2):169–84. doi: 10.1080/20004508.2020.1860284.
Daniella Arboleda Pazos 1, Gianluca Colucci 2
[1]
[2]
Tissue-mimicking materials play an integral role in clinical education through providing a controlled, risk-free environment for skill development. While commercially available phantoms enhance trainee proficiency and patient safety, their high cost and limited accessibility hinder widespread adoption. Consequently, clinical training often relies on supervised practice, constrained by logistical challenges and patient safety concerns. To address these limitations, ADAMgel was developed as a low-cost, non-toxic, and recyclable biomaterial designed to replicate human tissue properties [1]. Its successful integration into procedural training models highlights its potential as an effective simulation medium. ADAMgel offers several advantages, including versatility, affordability (<£2/kg), self-healing properties, bacterial resistance, and compatibility with diathermy and harmonic scalpels. Additionally, it closely mimics human tissue under ultrasound imaging, making it particularly valuable for sonography-based training. However, a lack of comprehensive mechanics data has restricted broader implementation in medical training. This study systematically evaluates the mechanical properties of six ADAMgel formulations to refine their suitability for simulation applications.
Six formulations were prepared with varying concentrations of psyllium husk, glycol, antifoam, water, and gellan gum to assess their impact on mechanical performance. Each underwent standardised tests, including Ultimate Tensile Strength, Young’s modulus in both tensile and compression modes, and durability evaluations. All tests were conducted in triplicate to ensure statistical reliability on the 15/01/24, with data incorporated into mathematical models for analysis.
A controlled preparation protocol ensured consistency, facilitating reproducible comparisons. Mechanical properties varied significantly across formulations. V5 exhibited the highest ultimate tensile strength (1308.12 Pa) and compressive resistance (6540.60 Pa), indicating superior load-bearing capacity. In contrast, V1 demonstrated the lowest tensile resilience (687.5 Pa), reinforcing the inverse correlation between increased water content and structural integrity. Young’s modulus in tension revealed that V4 was the most rigid (4216.03 Pa), while V1 and Standard formulations displayed greater elasticity. Durability testing indicated no material degradation following cyclic loading, supporting ADAMgel’s durability for repeated use. Gum-based formulations (V5, V4) demonstrated enhanced mechanical stability, whereas lower-viscosity variants (V1, V3) showed greater deformability, making them suitable for applications requiring flexibility. The incorporation of gellan gum (V5) significantly improved tensile properties, highlighting its potential for load-bearing applications in surgical training.
These findings underscore ADAMgel’s adaptability and provide empirical data for optimising formulations to better mimic specific tissue types. Future research should focus on refining ADAMgel’s composition to bridge the gap between synthetic and biological tissue properties, further enhancing its efficacy in procedural training models.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Willers J, Colucci G, Roberts A, Barnes L. 0031 Adamgel: An economical, easily prepared, versatile, selfrepairing and recyclable tissue analogue for procedural simulation training. 2015 Nov;A27.2-A27.
Aishwarya Venkatachalam Rajendran 1, Jessica Wadsworth 1, Ruth Millett 1, Kristine Damberg 1, Anuprita Harne 1
[1]
Swarm debrief is one of the Patient Safety Incident Response Framework (PSIRF) learning response methods [1]. It is a group debrief aimed at fostering collective, system-based learning, used immediately after any event where there is something new to learn. During the implementation of PSIRF in our trust, a gap in Swarm debriefing skills was identified, and the simulation and human factors team was asked to provide educational support. In collaboration with the patient safety team and input from the NHS England PSIRF team, we developed a systems-based Swarm guide and an accessible, engaging audio-visual (AV) Swarm simulation to illustrate a more realistic ‘work-as-done’ example [2].
A fictional patient incident was scripted, drawing inspiration from recent incident reviews and our own collective clinical experiences as healthcare professionals. The script mirrored the debriefing prompts and system-based questions within the Swarm guide so that viewers could review the guide and video concurrently. The video, featuring a nurse manager, doctor, nurse, and healthcare assistant, depicts a simulated Swarm debrief held in the manager’s office (Figure 1). Filmed on a smartphone and edited using Mac and CapCut software, the 15-minute video was enhanced with subtitles to improve accessibility and engagement.
The video has been shown to over 100 learning response leads as part of their formal Swarm debriefing training. The Swarm guide and video link are also hosted on our website and are freely available on YouTube, making these resources accessible to a wider audience.
Participants in the Swarm debrief training filled out a post-course survey, where 96.67% rated the video as “very helpful” in enhancing their understanding of a Swarm debrief. Participants described the video as “relatable,” “clear,” and “confidence-building,” noting that it helped clarify the process and provided a relevant and safe example for discussion. Faculty observed that the use of the video within the course enhanced participant engagement and reflective practice.
This AV simulated example of a Swarm debrief demonstrates how low-cost, low-tech media can be produced to enhance staff education and support PSIRF implementation. Video-based learning offers a powerful modality for teaching these complex skills, allowing learners to observe key interactions directed by the Swarm guide and reflect on the process [3]. This video provides a clear example of how a Swarm debrief should unfold in the real world, making this abstract concept more tangible.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. NHS England. NHS England» Patient Safety Incident Response Framework [Internet]. www.england.nhs.uk. 2022. Available from: https://www.england.nhs.uk/patient-safety/incident-response-framework/
2. Steven Shorrock. The Varieties of Human Work [Internet]. Humanistic Systems. Humanistic Systems; 2016. Available from: https://humanisticsystems.com/2016/12/05/the-varieties-of-human-work/
3. Morgado M, Botelho J, Machado V, Mendes JJ, Olusola Adesope, Luís Proença. Full title: Video-based approaches in health education: a systematic review and meta-analysis. Scientific Reports. 2024 Oct 10;14(1).

Dani Hall 1, 2, Victoria Meighan 3, 4, Rachael Mitchell 5, Constantinos Kanaris 2, 6, Kat Priddis 2, 7, Sarah Davies 8, Aidan Beegan 9, Michael Barrett 10, 11
[1] Department of Paediatric Emergency Medicine,
[2] Blizard Institute,
[3] Department of Emergency Medicine,
[4]
[5]
[6]
[7]
[8]
[9]
[10] Paediatric Emergency Research and Innovation, Department of Paediatric Emergency Medicine,
[11] Women’s and Children’s Health, School of Medicine,
Narrative theory states that stories allow learners to contextualise education in a way that is valid to them [1,2]. Simulation-based education is an effective teaching modality, correlating with improved clinical performance. Learners benefit most from simulated environments they are engaged with and believe to be authentic [3]. Traditionally this can be limited by the number of participants. We sought to validate a combination of narrative theory and simulation-based education in Paediatric Emergency Medicine (PEM) education at international conferences.
We delivered an interactive simulation-based session at the Royal College of Emergency Medicine 2024 (RCEM24) conference. Using a pre-test post-test design, knowledge of paediatric Toxic Shock Syndrome (TSS) resuscitation principles was assessed at baseline and six weeks. Team management of a child with TSS was simulated on stage. Using live-voting technology, the audience voted for next management steps in five elements of the case. Each voting choice was debriefed live, and linked to recent and key evidence-based literature. Human factors within the resuscitation were also demonstrated and debriefed live.
An online questionnaire was emailed to attendees six weeks after the conference, repeating the same five questions and assessing practice-changing behaviour. Statistical analysis was performed using Two sample Z test of proportions.
Ethical approval was granted by Queen Mary University of London.
Between 87 and 103 live-vote responses per interactive question were captured during the session. Forty-four attendees (43%) completed the post-conference survey at six weeks.
The proportion of correct live scores pre-education was low for all questions, indicating low baseline knowledge. The proportion of correct scores at six weeks was compared. Post-education scores were high, and improvement was statistically significant for all questions (p<0.05) (Table 1).
One attendee had managed paediatric TSS in the six weeks post-RCEM24, and said the evidence taught changed their practice. Of the remaining 43 respondents, 38 (88%) said the session would result in a change in their practice in the future.
Our results demonstrate that by combining narrative, authentic simulation and learner interaction, educators can engage learners in paediatric resuscitation education, improve knowledge, and generate practice-changing behaviour. This methodology can be applied to a large group setting, increasing accessibility to this evidence-based learning experience. This study will be reproduced at the Irish PEM 2025 conference to validate the results, extending post-education assessment to 12 weeks to explore sustained change.
Combining storytelling via simulation with audience participation makes simulation accessible and incredibly powerful.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Milota MM, van Thiel GJMW, van Delden JMM. Narrative Medicine as a Medical Education Tool: A Systematic Review. Medical Teacher. 2019 Apr. 14;41(7):802–810.
2. Meisel ZF, Metlay JP, Sinnenberg L et al. A Randomized Trial Testing the Effect of Narrative Vignettes Versus Guideline Summaries on Provider Response to a Professional Organization Clinical Policy for Safe Opioid Prescribing. Annals of Emergency Medicine. 2016 Dec;68(6):719–728.
3. Dankbaar MEW, Alsma J, Jansen EEH, van Merrienboer JJG, van Saase JLCM, Schuit SCE. An experimental study on the effects of a simulation game on students’ clinical cognitive skills and motivation. Adv in Health Sci Educ. 2016;21:505–521.

| Question descriptor | Pre-education proportion of correct responses during the live session, mean (95% CI) | Post-education proportion of correct responses at 6 weeks, mean (95% CI) | Estimate for difference, mean (95% CI) | P-value |
|---|---|---|---|---|
| Timing of intubation | 58.3 (48.8–67.8) | 81.8 (70.4–93.2) | 23.5 (8.6–38.4) | 0.006 |
| Ventilation strategies | 35.6 (25.5–45.7) | 72.7 (59.5–85.9) | 37.1 (20.5–53.7) | <0.001 |
| Pulmonary haemorrhage | 5.2 (0.7–9.6) | 68.2 (54.4–82.0) | 63.0 (48.5–77.5) | <0.001 |
| Third line inotropes | 53.8 (43.6–64.0) | 93.2 (85.8–100) | 39.4 (26.7–52.1) | <0.001 |
| Intravenous immunoglobulin | 65.2 (55.5–74.9) | 90.9 (82.4–99.4) | 25.7 (12.8–38.6) | 0.002 |
Giuseppe Leontino 1, 2, Alison Vacani 1, Aidan Mitchell 1
[1]
[2]
Due to an everchanging healthcare environment and reduced placement availability, the NMC [1] has proposed the adoption of simulated practice learning (SPL). This has encouraged many higher education institutions (HEIs) across the country to bolster the simulation provision, preparing nursing students to face the challenges of the future in a safe environment without the risks associated with clinical practice [2].
During SPL planning for a last year undergraduate adult nursing masters programme, a learning need was identified through learners’ feedback, which highlighted their keenness to explore critical care before graduating. As the placement capacity could not be increased to accommodate large number of learners, the intensive care unit (ICU) environment was recreated digitally through projector-based interactive technology. Medical equipment, sounds, AI generated people, interactive touch-points and bed spaces were developed to increase immersion.
This paper focuses on the team’s own learning journey in adopting the technology, whilst sharing with the simulation community challenges and lessons learnt.
This initiative took eight weeks to develop and applied the experiential learning theory to immersive-interactive technology, combining experience, perception, cognition and behaviour [3]. A post-test design was employed to target and address pre-identified challenges (Table 1). The faculty took notes throughout the sessions and reported observations to the team lead.
The two-hour-long experience followed a patient’s journey from admission to discharge and aimed to enhance understanding of specialised equipment, MDT approach, deterioration management including delirium, patient and family’s perspective on being cared for in ICU. Quizzes, videos, drag and drop exercises and a Padlet QR code were embedded to support different learning styles and maximise engagement.
Structured and tailored pre-brief, brief and debriefing, using the PEARLS model, reinforced learning and assured psychological safety throughout.
The steps below led to implementation.
Identify the gap
Form a team
Develop vision and aims
Develop the content
Deliver & evaluate
The team met to discuss foreseen challenges and findings after each iteration. The findings and solution after 4 iterations are presented in Table 1.
Implementation required a multidisciplinary approach, including educators, learning technologists, and clinicians to provide a clinically sound and psychologically safe exploratory journey of a complex placement area. Albeit the initiative was successful, the literature on immersive room implementation in healthcare programmes is scarce and future work should focus on:
Developing validated frameworks, ensuring consistency and learning effectiveness
Implementing the technology to prepare learners for placement areas like the ICU and evaluate its effectiveness
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Nursing and Midwifery Council. The Code - Professional standards of practice and behaviour for nurses, midwives and nursing associates 2018. Available at: NMC. Accessed 1 October 2024.
2. Bearman M, Greenhill J, Nestel D. ‘The power of simulation: a large-scale narrative analysis of learners’. Medical Education. 2019;53(4):369–379.
3. Kolb DA. Experiential learning: Experience as the source of learning and development. Englewood Cliffs, NJ: Prentice Hall; 1984.

| Findings | Solution | |
|---|---|---|
| Lack of standardised practice | Unlike the tried and tested VR-based simulation, no established framework or model existed for designing and delivering an immersive room experience, leading to uncertainty and apprehension. | Produce an ad-hoc template to capture, LOs; Sequence flow (what happens at this stage); Resources needed (images, videos, sounds etc.); Interactive activity, (quizzes, drag and drop etc.) |
| Software inexperience | The team was unfamiliar with immersive room technology. | Regular catchups and training workshops were introduced, fostering progressive skills development. |
| Competing priorities | Balancing simulation development with teaching responsibilities proved challenging. | Using one version of a shared live document to identify critical steps, responsible person and obstacles, enabled asynchronous collaboration. |
| Educational effectiveness | Due to lack of prior experience, there were no metrics that could be used as benchmark. | A dry run, for faculty only, was conducted to test functionality and check timings. A lesson plan (LP) and a narrated video for faculty were instrumental to align LOs to delivery. The LP contained navigation of the scenes, layout of the room, duration of each scene, specific activities to run like quizzes and videos, discussion points, pre-brief, brief and debrief. |
| Learning and engagement | Long videos and long text caused engagement to drop. | Limit passive learning. Videos were shortened, whilst discussion points and dynamic activities were encouraged. |
| Future iterations | Further developments and activities stemmed from this experience. | The learning technologist adopted the template used for this experience as a starting block for a different session, resulting in a much quicker and streamlined development. |
Jorge Lopes Ramos 1
[1]
Empathy and effective communication are critical to safe, patient-centered healthcare, yet these ‘softer’ skills are often underdeveloped in traditional training when compared to ‘harder’ skills [1, 2]. Simulation tools exploring immersive and XR technologies can often prioritise clinical tasks over emotional engagement. Emerging from an arts-led collaboration between disabled-led arts organisation ZU-UK and researchers at the University of Greenwich, SIMFONIK is an app-based, audio-led XR simulation platform that uses storytelling, immersive audio, and scaffolded role-play to enhance healthcare students’ empathy [3], communication resilience, and emotional awareness. Drawing from techniques in serious games, LARP, and immersive theatre, SIMFONIK places students directly into the patient’s perspective through progressive and accessible instruction-led experiences.
A beta version of the SIMFONIK app has been piloted with undergraduate nursing cohorts at the University of Greenwich, and healthcare simulation staff across five UK universities. Using bone-conduction headphones, participants experienced the scenarios in pairs - receiving real-time role-play instructions within a range of patient scenarios. Instructions gradually shifted from directive to autonomous, encouraging independent empathic decision-making. Sessions were framed by clear pre-briefs and structured debriefs. Pre/post surveys assessed self-rated empathy and communication confidence.
Preliminary findings suggest positive impact. Across pilot sites, 81% of participants reported increased empathy and communication confidence. Average self-rated empathy scores improved by approximately one point on a seven-point scale post-session. Learners described the experience as understanding “what (empathy) really means,” “intense, making you actually think and feel,” and feeling “more equipped to implement it in practice,” highlighting the emotional realism generated by the audio storytelling and real-time role-play. Educators noted potential for greater engagement, deeper reflection around ‘hard-to-teach skills’, and improved emotional vocabulary. SIMFONIK’s technical setup proved low-cost, scalable, and adaptable to different classroom environments without the need for VR or specialist rooms.
Early evidence indicates that SIMFONIK effectively supports empathy and communication development in healthcare education. By combining scaffolded instructions with immersive storytelling, the platform enables students to explore patient emotions safely and build emotional resilience. SIMFONIK’s accessibility, emotional impact, and adaptability make it a strong candidate for integration into healthcare curricula seeking to develop compassionate, patient-centered practitioners. Further evaluation will focus on longitudinal impacts and expansion to broader healthcare disciplines.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Cho MK, Kim MY. Effectiveness of simulation-based interventions on empathy enhancement among nursing students: a systematic review and meta-analysis. BMC Nurs. 2024;23:319.
2. Bearman M, Palermo C, Allen LM, Williams B. Learning empathy through simulation: a systematic literature review. Simul Healthc. 2015;10(5):308–314.
3. Lopes Ramos J, Guillery K, Maravala PJ. Role-Play & Instruction: An Experiential Approach to Building Care. In: Saygin Ö, editor. Role-Play and Simulation. London: Bloomsbury; 2023. p. 135–149.
As a result of recent support from the AHRC/ESRC ARC Accelerate Catalyst Programme, SIMFONIK is currently being established as a spinout company.
ARC Accelerate programme (AHRC/ESRC), 2024-25
InnovateUK Creative Catalyst Programme, 2024-25
Nicola Steeds 1
[1]
Public satisfaction with General Practice (GP) services has reached an all-time low, amid increasing demand for appointments and strain on resources. In response, the UK government launched the “Delivery Plan for Recovering Access to Primary Care,” which includes a commitment to modernise primary care and improve patient access through digital innovation. A key component of this transformation is the implementation of Total Patient Triage (TPT), a model that assesses all patient contacts to determine the most appropriate clinical pathway. Widely adopted during the COVID-19 pandemic, TPT facilitates remote consultations, reduces reliance on traditional telephone booking systems, and aims to optimise time for both patients and clinicians.
This project aimed to evaluate whether training using simulation could enhance NHS staff understanding of the TPT model and foster collaborative working across all roles in General Practice.
A tabletop simulation was developed using a bespoke “triage card” system. Fourty anonymised, real-life patient queries were printed on cards resembling a deck of playing cards. Each query was paired with a range of potential triage outcomes, such as referral to a GP, pharmacist, nurse, or digital response options like questionnaires. Participants were asked to decide on the appropriate clinician, mode of consultation (face-to-face or remote), and urgency (same day, two weeks, or routine). Additionally, a set of “CHANCE” cards, inspired by the Monopoly game, introduced unexpected scenarios (e.g., medical emergencies) to encourage discussion around managing unpredictable events and their ripple effects on workload.
The simulation was conducted across five GP practices in Surrey during protected learning time (PLT), involving both clinical and administrative staff. The session was also delivered to GP trainees at the Royal Surrey County Hospital.
Participants completed an anonymous online feedback form, capturing their roles, prior interest in TPT, and session evaluation using a Likert scale. All respondents (100%) indicated they would recommend the session to colleagues. Feedback highlighted increased awareness of TPT and emphasised the value of multidisciplinary collaboration in improving patient flow and care prioritisation (Table 1).
The training simulation proved effective in promoting understanding of the TPT model and enhancing team-based decision-making. Bringing together diverse roles in a shared learning environment helped reinforce the collective responsibility and adaptability needed to manage modern primary care demands
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Morris J SL, Dayan M, Jefferies D, Maguire D, Merry L, Wellings D.. Public satisfaction with the NHS and social care in 2022. Results from the British Social Attitudes survey 2023 The Kings Fund; 2023.
2. England N. Delivery plan for recovering access to primary care. NHS Engl. 2023.
3. NHSEngland. Modern General Practice model2024 25th October 2024. Available from: https://www.england.nhs.uk/gp/national-general-practice-improvement-programme/modern-general-practice-model/.
I would like to express my sincere gratitude to all the individuals, organisations and teams who contributed to the development of this project. Your invaluable support, insights and expertise have significantly enhanced the quality of this work. Thank you for your guidance and encouragement throughout this process: Dr Jane Roome, Dr Jackie Knight, Dr Shereen Habib, Dr Jonathan Inglesfield.

| On a scale of 1-5 (5 being ‘strongly agree’ and 1 being ‘strongly disagree’), how much do you agree with the following statements? | Average score |
|---|---|
| I felt that today was interactive and stimulating. | 4.92 |
| I felt that today was relevant to my development needs. | 4.82 |
| I found today’s tabletop simulation useful. | 4.78 |
| My awareness of the total patient triage process has increased because of today’s session. | 4.68 |
Egle Mattar 1
[1]
Simulation-based training has been shown to significantly improve clinician performance in emergency front of neck access (eFONA), particularly among professionals in high-acuity settings [1]. However, traditional simulation options—including animal tissue models and commercially available part-task trainers—present notable limitations. Ethical concerns, unpleasant sensory experiences, high costs, and environmental impacts restrict their accessibility and scalability. In response to ongoing budget constraints within the NHS, we aimed to develop a low-cost, sustainable, and easily reproducible model for eFONA training using readily available materials.
Inspired by commercially available part-task trainers [2], we developed a prototype using plaster of Paris (POP), washing machine waste pipe, sleek tape, silicone, and a balloon. The total material cost per unit was £1.65. During the design process each prototype was tested and adaptations were made to ensure functionality, such as minor increases in diameter of the ‘cricothyroid membrane’ to ensure compatibility with a size 6 endotracheal tube. Functionality was further validated by an anaesthetist prior to course deployment.
The model was implemented in a trauma simulation course, where both quantitative and qualitative feedback were collected from participants regarding anatomical realism, tactile feedback, and overall usability (see Figure 1).
All participants rated the models realistic or very realistic in terms of anatomical landmarks and procedural feel, and all said that they would recommend using the models. Participants commented on specific features of the models:
1. “Landmarks easily identified and able to see if successful due to ballon inflation which have not seen on previous animal models/ models used”
2. “Able to practice procedure without needing animal models is great”
Cost analysis revealed an average saving of £612 per unit compared to four commercially available part-task trainers.
This low-cost, ethical, sustainable, and reusable alternative to traditional part-task trainers represents a significant step forward in accessible simulation training. Its favourable cost profile and positive user reception support its integration into existing training programmes, particularly in resource-constrained healthcare environments. Such innovations demonstrate that high-quality simulation education need not come at high financial or ethical cost and can be easily reproduced in any simulation setting.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Hubert V, Duwat A, Deransy R, Mahjoub Y, Dupont H. Effect of simulation training on compliance with difficult airway management algorithms, technical ability, and skills retention for emergency cricothyrotomy. Anesthesiology. 2014 Apr;120(4):999–1008. doi: 10.1097/ALN.0000000000000138. PMID: 24434303.
2. Winterbottom T, Patel B, King W. Cricothyroidotomy trainer review. Difficult Airway Society; 2018 [cited 2025 Apr 16]. Available from: https://database.das.uk.com/cricothyroidotomy_trainer_review
I would like to thank Dr Amy Ireson for her support in writing my first abstract!

Sandra Goldsworthy 1, Keith Weeks 2, Sue Baron 3, Naim Abdulmohdi 4, Karey McCullough 5, Nita Muir 6, Kim Sears 7, Kate Goodhand 8, Alex Weeks 9, Grace Perez 10, Laurence Moseley 2, Matt Brown 2, David Pontin 9
[1]
[2]
[3]
[4]
[5]
[6]
[7]
[8]
[9]
[10]
Medication administration is a high-risk clinical task, with errors contributing to preventable harm worldwide [1]. Competence in medicine calculation is essential to patient safety, yet nursing students often report anxiety and low confidence, increasing the risk of errors. Virtual learning environments provide valuable opportunities to develop students’ skills, build confidence, and enhance competency in medication administration.
This pilot study investigated the relationship between exposure duration to asynchronous virtual medication dosage calculation scenarios and nursing student actual and perceived competence, using a randomised quasi-experimental research design (pre- and post-test). Ethical approval was gained at each site before second/third-year pre-registration undergraduate nursing students were recruited from six sites in the UK and Canada in 2023 using purposive sampling. Participating students completed an orientation to the safeMedicate® Authentic Virtual Drug Dosage Calculation Clinical Learning Environment (VLE), and safeMedicate® 25-item Healthcare Numeracy Assessment (HNA) before being allocated to one of four groups with different exposure times to a safeMedicate® COVID-19 education module.
Actual and perceived competence assessment outcomes for all students (n=38) across the four groups were analysed and compared before and after variable exposure to the intervention using descriptive and inferential statistical analyses. Results showed that groups were homogeneous at baseline, i.e. no differences in the mean pre-test assessment results. Post-test assessment results showed that mean actual competence scores increased from 77 pre-test to 92 post-test, with perceived competence scores mirroring these results for all groups, including the control group which did not have intervention exposure. There was no evidence of significant outcome differences between groups with varied exposure duration, suggesting that increased exposure time did not translate into enhanced competence improvement. Rather, results indicated that exposure to the VLE and initial baseline and HNA assessments with outcome feedback had the greatest influence on the improvements found, and the psychological and confidence-building value of this VLE. This is consistent with previous research on self-efficacy enhancement effects of digital learning [2,3].
The lack of significant differences between groups with varying exposure durations found in this pilot study contradicts earlier studies advocating for prolonged engagement with VLEs to achieve competence [4]. Instead, the findings suggest that the increase in actual and perceived competency scores occurred because feedback on performance was also provided to students after each VLE assessment they completed. This may indicate that simulation-based intervention effectiveness is based on instructional design rather than on exposure time. However, because a key limitation of this pilot study is its small sample size, further research on a larger scale building on this pilot study is needed to explore and understand the impact of instructional design, feedback, and interaction on learning outcomes and the psychological and confidence-building value of this intervention and VLE.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable
1. World Health Organization. Global burden of preventable medication-related harm in health care: A systematic review. Geneva: World Health Organization; 2023. Available from: https://iris.who.int/bitstream/handle/10665/376203/9789240088887-eng.pdf?sequence=1.
2. Goldsworthy S, Muir N, Baron S, et al. The impact of virtual simulation on the recognition and response to the rapidly deteriorating patient among undergraduate nursing students. Nurse Education Today. 2022;110.
3. Heyn LG, Brembo EA, Byermoen KR, et al. Exploring facilitation in virtual simulation in nursing education: a scoping review. PEC Innovation. 2023;3.
4. Sato SN, Moreno EC, Rubio-Zarapuz A, et al. Navigating the new normal: adapting online and distance learning in the post-pandemic era. Education Sciences. 2024;14(1):1–25.
The authors acknowledge the Canadian Association of Schools for Nursing (CASN) for the Pat Griffin Grant. Special thanks to Fiona Budden, Ryan Muldoon and Jan Hutt from Bournemouth University.
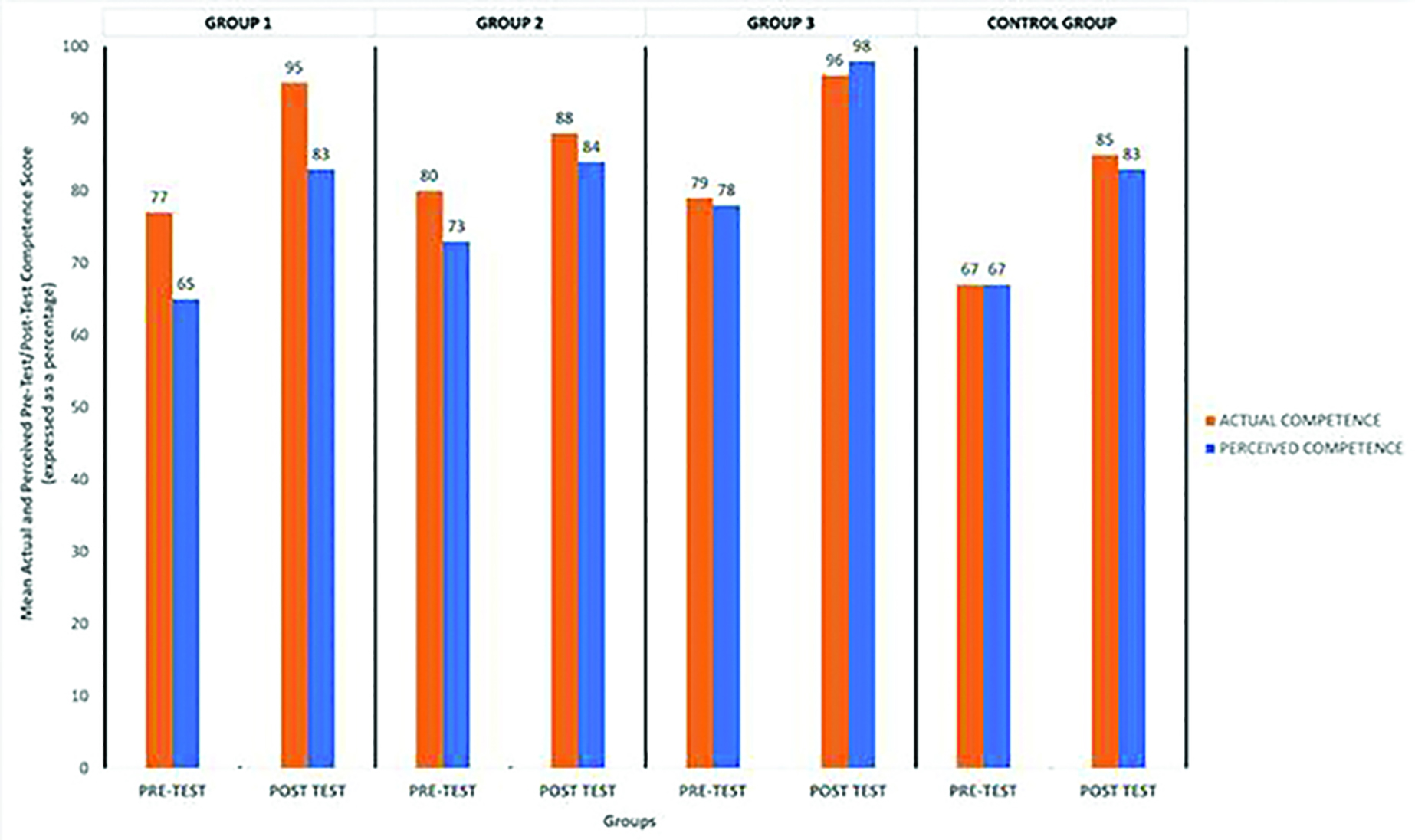
Gemma Blaza 1, Karen Hodges 1
[1]
It is known that for approximately 70% of tertiary level burns referrals, total body surface area (TBSA) calculations are largely overestimated. Furthermore, patients at the point of arrival often are inadequately fluid resuscitated. A learning need to address these factors for multi-disciplinary emergency and surgical care teams was identified, simulation is recommended as a useful tool to prepare health care workers for such cases and address skills gaps amongst teams [1]. A study conducted in 2016 [2] emphasized the affirmative impact of employing moulage based simulation of burns injuries on the overall learning process. In answer to this we have developed an innovative methodology for creating representations of full thickness burns on simulation manikins.
In collaboration between the Burns and Simulation teams, scenarios for simulation were developed from real life cases. A variety of cost and time effective moulage techniques for different burn modalities were developed.
The simulation technician implemented a technique of crafting flat clay moulds of burn wounds for the production of silicone overlays, these were painted with depth-indicating paint, and then adhered to manikins.
From 2023 to 2025 we have run 7 regional simulation days with 73 delegates and 56 pre and post course feedback responses. A summary of confidence ratings across differing aspects of burns care can be found in Figure 1. A mixture of confidence scoring from very low to relatively high was recorded dependant on exposure to burns, training and professional backgrounds, across all categories an increase in confidence was recorded overall.
Traditional methods of using make up paint and wig spray to simulate a burn on a patient have the benefit of being fast to implement and cheap. However, limitation on the realism of the injury have the potential to both inhibit the learner to fully grasp the extent of burn coverage and reduces the emotional impact that one has when presented with a full thickness burn.
Increased confidence and technical skill in the initial management of severe burns in multi-disciplinary emergency teams will lead to improvements in burns patient outcomes.
The model for high fidelity burns moulage has far reaching potential beyond the regional simulation course that it was initially developed for. These scenarios have been utilised in several training opportunities such as national symposium’s, care pathway trials as well as future plans to bring burns simulation to emergency response teams by working collaboratively fire and ambulance services.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. D’Asta F, Homsi J, Sforzi I, Wilson D, De Luca M. “SIMBurns”: A high-fidelity simulation program in emergency burn management developed through international collaboration. Burns [Internet]. 2018 Sep 26;45(1):120–7. doi: 10.1016/j.burns.2018.08.030.
2. Sadideen H, D’Asta F, Moiemen N, Wilson Y. Does overestimation of burn size in children requiring fluid resuscitation cause any harm? Journal of Burn Care & Research [Internet]. 2016 Jul 4;38(2):e546–51. doi: 10.1097/bcr.0000000000000382.
Special acknowledgements to Miss Alexandra Murray, (Consultant in Plastic Surgery and Burns at Buckinghamshire Healthcare NHS Trust) and Alexander Baldwin (Surgical Trainee in Plastic Surgery at Buckinghamshire Healthcare NHS Trust) for their ongoing support and enthusiasm as subject matter experts.
An acknowledgement to Ella Anthony (Burns Outreach Nurse at Buckinghamshire Healthcare NHS Trust) for her ongoing commitment to collaborate with us to diversify burns teaching for a multi agency and professional audience.
The initiative was financially supported by Health Education England with the aim of generating additional training prospects for trainees in the Thames Valley region, compensating for the training opportunities that were forgone during the COVID-19 pandemic.
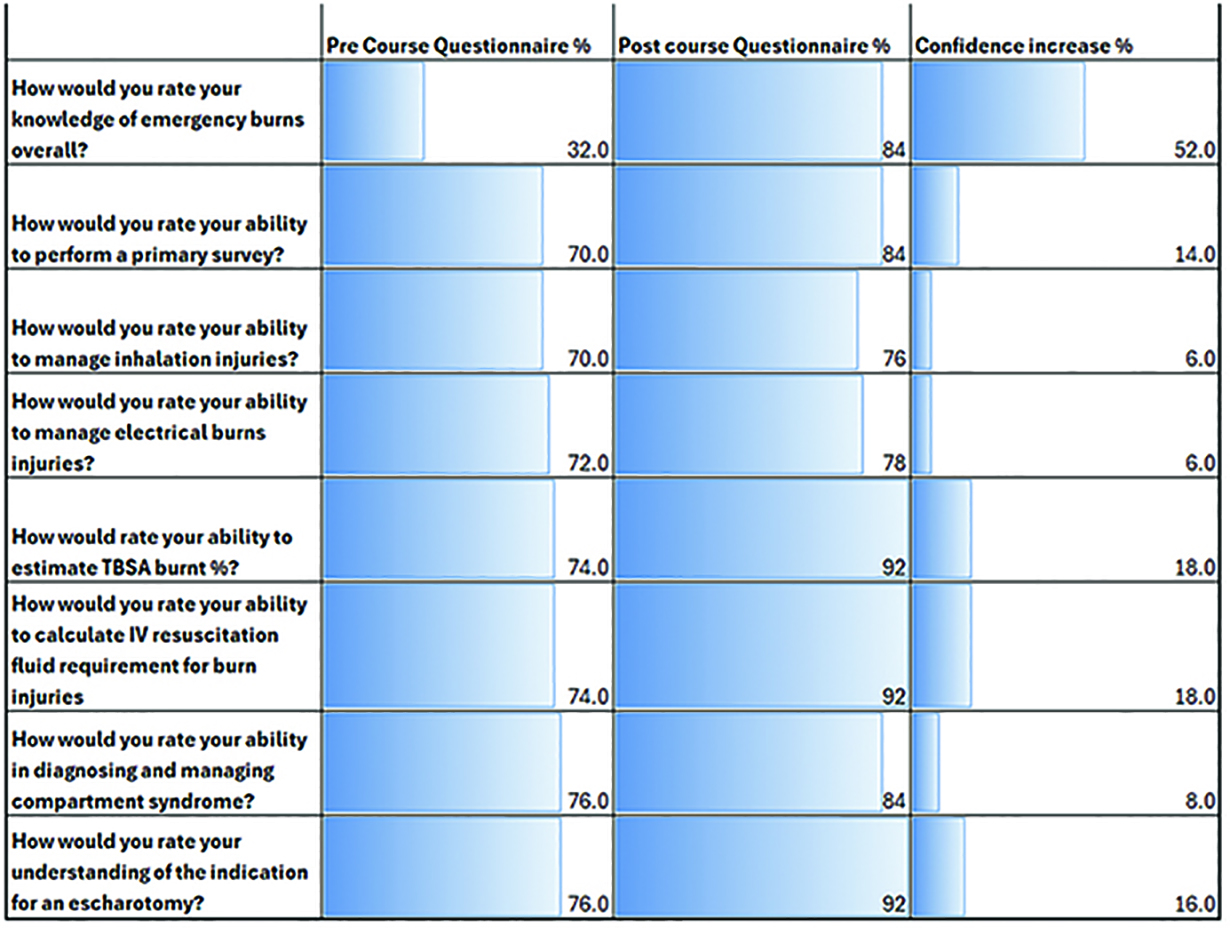
Stephen Ojo 1, Beili Shao 1, Sanjida Chowdhury 1
[1]
[2]
Augmented reality (AR) provides interactive and immersive experiences that enrich medical training by enhancing learners’ spatial understanding, clinical decision-making, and engagement [1-3]. However, the uptake of AR across educational institutions remains inconsistent due to variations in infrastructure, cost, and training. This study aimed to explore medical students’ experiences with AR, measure their immersion levels, and identify perceived benefits and barriers, particularly those linked to digital inequality.
A cross-sectional survey was conducted in 2024-2025 at a UK medical school following an AR-enhanced simulation session using HoloLens headsets and the HoloPatient application. Ninety-three medical students participated voluntarily. The Augmented Immersion Measurement Index (AIMI) was used to assess engagement across cognitive, emotional, and behavioural domains. Students also reported AR usage frequency, perceived educational benefits, technological limitations, and concerns about equitable access. Descriptive and correlational analyses were performed.
Students reported moderate immersion (mean AIMI score: 3.9/5), with emotional engagement highest (4.2/5) and behavioural engagement lowest (3.5/5). Key benefits included enhanced diagnostic reasoning (32%), improved patient interaction skills (28%), and increased surgical confidence (20%). However, 30% cited limited access to AR-enabled devices, and 27% reported lack of institutional support as major barriers. Over half (53%) expressed concern that AR could widen digital inequality. Subgroup analysis showed students with regular AR access had higher confidence in spatial awareness and technical skills. Conversely, those from lower-income backgrounds reported limited access, lower immersion scores, and less perceived benefit. Despite challenges, students valued AR’s ability to visualise complex anatomy, simulate clinical encounters, and reinforce theoretical learning.
This study confirms that AR can improve learner engagement and perceived clinical preparedness. However, barriers related to access, affordability, and institutional readiness may hinder equitable implementation. AR should be adopted as a supplemental tool within blended learning models. Institutions must invest in infrastructure, faculty training, and accessibility schemes—such as device loans or subsidies—to maximise educational benefit and mitigate the digital divide. Future studies should examine long-term skill retention, impact on clinical performance, and cost-effectiveness of AR-based medical education.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Moro C, Birt J, Stromberga Z, Phelps C, Clark J. Virtual and augmented reality enhancements to medical and science student physiology and anatomy test performance: a systematic review and meta-analysis. Anat Sci Educ. 2021;14(3):368–76.
2. George O, Foster J, Xia Z, et al. Augmented reality in medical education: a mixed methods feasibility study. Cureus. 2023;15(3):e36927.
3. Li X, Elnagar D, Song G, Ghannam R. Advancing medical education using virtual and augmented reality in low- and middle-income countries: a systematic and critical review. Virtual Worlds. 2024;3(3):384–403.
DREEAM, Nottingham University Hospital, UK for use of Hololens and Holopatient platfor
Hayley Lawson-Wood 1, Lorraine Whatley 1, Janice Watson 1
[1]
Nursing and Midwifery Council (NMC) approved institutions can deliver up to 600 hours of Simulated Practice Learning (SPL) within the 2,300 practice hours, pre-registration nursing students are required to register [1]. Many approved Higher Education Institutions (HEIs) are using immersive technology-enhanced learning as part of a blended approach in their SPL delivery. Virtual Reality (VR) is commonly used to simulate immersive environments where learners can practise decision-making skills within different clinical contexts. Alongside this, there is a need for 3rd year nursing students to develop peer supervision and coaching skills in preparation for registration [2]. The purpose of this work is to report on an evaluation of a teaching intervention, utilising both VR and peer-to-peer learning.
A peer-to-peer VR learning experience was delivered to 22, 3rd year children’s nurses using Oxford Medical Simulation (OMS) software. Students were paired, with one undertaking a simulation scenario using a VR Oculus headset, which was streamed to a computer screen. The second student observed this stream and made notes on their peers’ performance for feedback. The pair then had an unstructured debrief to explore ways to improve their performance. The roles were then reversed with the observing student completing the same scenario. Following this activity, the wider group came together for a facilitated debrief using the diamond debrief model [3].
Data collection included quantitative and qualitative student feedback gathered via a scannable QR code and quantitative data from the OMS platform’s feedback scoring system.
Qualitative findings brought up two main themes: translating theory to practice & and peer-to-peer support. Limitations of using immersive technology were also highlighted.
Quantitative results showed an overall improvement in clinical practice between the peer attempts. These results are seen in Table 1. Out of the 11 pairs of participants, 7 scored, on average, 18.12% better than their peers. Of the 3 pairs of participants that scored lower, they were 4.64% lower than their peers.
Repeated peer-supported VR scenarios have the potential to improve knowledge and enhance peer supervision. Importantly, the post-scenario debrief was positively received by the majority of learners to consolidate their in-scenario peer learning. We suggest that the value of using this approach within SPL may be an effective way for 3rd year student nurses to acquire knowledge and develop peer supervision skills. Challenges arose surrounding the use of a VR headset and limitations in using a virtual platform.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Nursing & Midwifery Council (NMC). Simulated Practice Learning [Internet]. 2024 Available from: https://www.nmc.org.uk/standards/guidance/supporting-information-for-our-education-and-training-standards/simulated-practice-learning/.
2. Yoong SQ, Wang W, Chao FFT, et al. Using peer feedback to enhance nursing students’ reflective abilities, clinical competencies and sense of empowerment: A mixed-methods study. Nurse Education in Practice. 2023;69:1–21. doi: 10.1016/j.nepr.2023.103623.
3. Jaye P, Thomas L, Reedy G. ‘The Diamond’: A structure for simulation debrief. The Clinical Teacher. 2015;12(3):171–175. doi: 10.1111/tct.12300.

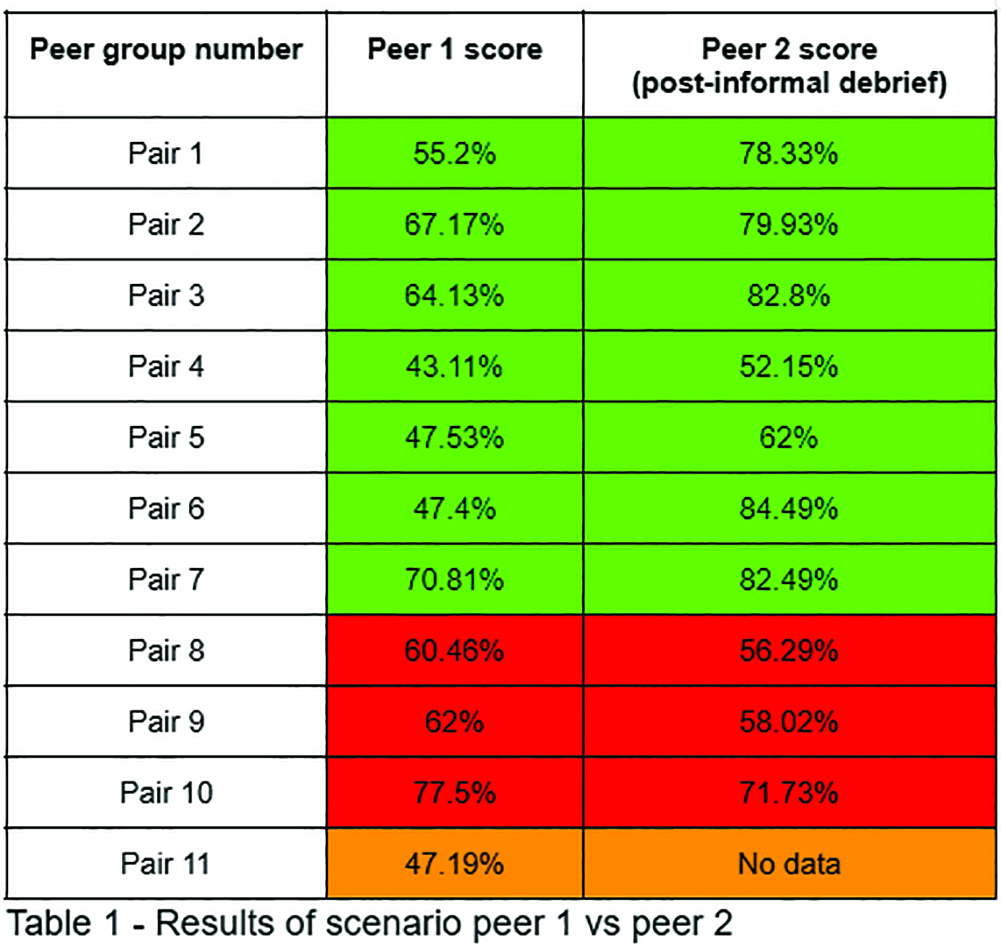 |
Trisha Choudhary 1, Hajnalka Huszka 2, Johann Willers 2, Alexander Hill 3
[1]
[2]
[3]
Rectus Sheath Block (RSB) is a ‘Plan A’ regional anaesthesia technique used for perioperative pain management in abdominal surgeries [1]. Anaesthetists must perform these blocks proficiently, yet limited training opportunities reduce confidence and procedural uptake. Simulation training offers a solution, but existing models are often costly or lack anatomical realism. This study aims to develop and evaluate a cost-effective, anatomically representative, and reusable RSB training model.
This prospective quality improvement project was registered with University Hospitals Sussex NHS Foundation Trust. A portable anterior abdominal wall model was constructed in a 1L storage container using ADAMgel, a low-cost, ultrasound-compatible material, alongside commercially available components such as chia seeds and latex exercise band [2]. The prototype was refined based on expert feedback. Anaesthetists from two hospitals evaluated the model by performing ultrasound scanning and needle insertions, on the 22/01/2025 and 07/02/2025 respectively. Feedback was then collected via an online questionnaire assessing ease of use, anatomical realism, needling practice, and overall usefulness on a 5-point Likert scale. Free-text responses provided additional insights. Quantitative data were analysed using descriptive statistics in Microsoft Excel, while qualitative data underwent thematic analysis.
Twelve anaesthetists (10 trainees, 2 consultants) evaluated the model. The majority (83%) found it easy to use (Likert score 4 or 5), and the same proportion considered it anatomically realistic. However, the most frequent suggestion was improving anatomical accuracy, particularly by varying the thickness of the transversus abdominis, internal oblique, and external oblique muscles. The model was especially valued as a medium to practice needling, with 92% rating it 4 or 5. This idea was further reflected in the free-text feedback where the realistic tactile response and reusable nature of the model were identified as key strengths.
This study demonstrates that a low-cost, reusable RSB training model can be effectively constructed using ADAMgel and other commercially available materials. The model was well received, particularly for its suitability for needling practice and realistic tactile feedback. Future improvements will focus on enhancing anatomical accuracy and enabling local anaesthetic injection to create a more lifelike experience. By providing an accessible training tool, this model has the potential to improve trainee confidence and proficiency, supporting regional anaesthesia training.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicabley.
1. Introduction | The Royal College of Anaesthetists [Internet]. [cited 2025 Mar 16]. Available from: https://www.rcoa.ac.uk/documents/2021-curriculum-cct-anaesthetics/introduction
2. Willers J, Colucci G, Roberts A, Barnes L. 0031 Adamgel: An economical, easily prepared, versatile, selfrepairing and recyclable tissue analogue for procedural simulation training. 2015 Nov;A27.2-A27.
Hajnalka Huszka 1, Nicholas Tovell 1
[1]
Table-top simulation is an innovative low fidelity simulation tool which has become trendy over the last few years. Despite its popularity the effectiveness of table-top exercises has not yet been examined in the literature. This narrative review aimed to examine if table-top simulation is an effective educational tool.
Studies were identified examining the effectiveness of table-top simulation from multiple databases. More than 100 publications were identified. After the screening process 26 studies were included as per the inclusion and exclusion criteria. Qualitative and quantitative studies were both included. Following basic descriptive measures, target audience, sample size, training needs assessment, learning outcomes and change in practice or behaviour were examined in each study. Findings were examined in the context of Kirkpatrick’s evaluation model and Moore’s expanded framework.
Table-top simulation was used for different reasons. Most commonly it was used to identify a gap in knowledge, transfer knowledge or as a type of assessment. As an educational tool it is effective on the lower levels of Kirkpatrick’s evaluation model and is not inferior when compared with high fidelity simulation [1]. It is well accepted by users through providing a safe and controlled environment for students to practise and refine their skills. Additional benefits include improvement in non-technical skills, feeling empowered to make decisions and increased sense of comfort.
Table-top simulation is effective and should be used in addition to traditional educational tools.
Some studies suggest that due to its resource and cost-effectivity table-top simulation is ideal for low or middle income countries. It can be used to deliver a variety of topics especially those that are not easy to fit into traditional simulation content such as disability, disaster medicine or opioid use disorder. It is highly beneficial for multi disciplinary teams to understand complex multidisciplinary team dynamics and improve collaboration between team members.
This review confirms that there is a place for table-top simulation in medical education. Further studies are required to determine the effectiveness of table-top simulation on higher levels of Kirkpatrick’s model of evaluation and Moore’s expanded framework, to prove cost-effectiveness, investigate sustainability and to evaluate table-top simulation as an assessment method.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable
1. Offenbacher J, Petti A, Han Xu, Levine M, Manyapu M, Guha D, et al. Learning Outcomes of High-fidelity versus Table-Top Simulation in Undergraduate Emergency Medicine Education: Prospective, Randomized, Crossover-Controlled Study. West J Emerg Med Integrating Emerg Care Popul Health. 2022 Jan;23(1):20–5.
Janice Watson 1, Harry Wood 1, Russell Sinclair 1
[1]
Increasingly adopted in healthcare education for their ability to engage learners, develop teamwork and critical thinking skills, escape rooms are defined as ‘live-action, team-based games where players discover clues, solve puzzles, and accomplish tasks in one or more rooms in order to accomplish a specific goal’ [1]. The literature suggests that escape rooms have the potential to engage learners[2,3]. Our simulation team, consisting of academic and simulation technicians, created a virtual escape room using IntuifaceTM software for our immersive learning environment. This interactive touchscreen experience allowed nursing students to practice critical thinking, communication, and teamwork as they navigated a virtual patient’s home, consisting of a linear storyline of puzzles within a 40-minute limit. These were focused on wound assessment and management.
This learning experience involved groups of up to 12 students, structured with rotating participation of 5-6 active learners, and 5-6 active observers who contributed suggestions and insights. Solving the sequential puzzles demanded effective teamwork, clear communication, and the application of knowledge relevant to the scenario’s phases: history taking, information gathering, the correct utilization of wound assessment tools, and the selection of appropriate wound dressings. A simulation technician facilitated the technical operation, while an academic facilitator guided the in-experience discussions and debriefing to enhance learning.
Feedback was collected from participants at the end of each session via a QR code. A total of 6 sessions were delivered in 1 day. 65 students took part, with 31 completing the evaluation form (response rate of 47.7%). Overall, student feedback indicated a positive learning experience and participants reported high levels of enjoyment and engagement with the activities, with evidence of perceptions of successful teamwork and communication. Additionally, at least one student noted the development of valuable skills such as critical thinking and problem-solving. The unique and fun nature of the session appears to have contributed to this learning opportunity, see Figure 1.
The feedback identified a potential area for improvement which was highlighted by “more time and guidance”, suggesting that some students may have felt pressed for time, or required additional support to fully benefit from the activities. This warrants consideration in future session planning to ensure adequate time allocation and appropriate levels of guidance are provided to accommodate all learners. Despite this point for potential enhancement, the feedback suggests the learning experience was innovative and well-received by the participating students, and will be embedded in future nursing curricula.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Nicholson S. Peeking Behind the Locked Door: A Survey of Escape Room Facilities [Internet]. 2015. Available from: http://scottnicholson.com/pubs/erfacwhite.pdf. Accessed 10 April 2025.
2. Millsaps ER, Swihart AK, Lemar HB. Time is brain: Utilizing escape rooms as an alternative educational assignment in undergraduate nursing education. Teaching and Learning in Nursing. 2022 Mar;17: 323–327.
3. Lin Hui Quek, Apphia J.Q. Tan, Marcia J.J. Sim, Ignacio J, Harder N, Lamb A, et al. Educational escape rooms for healthcare students: A systematic review. Nurse education today. 2024 Jan 1;132:106004–4.

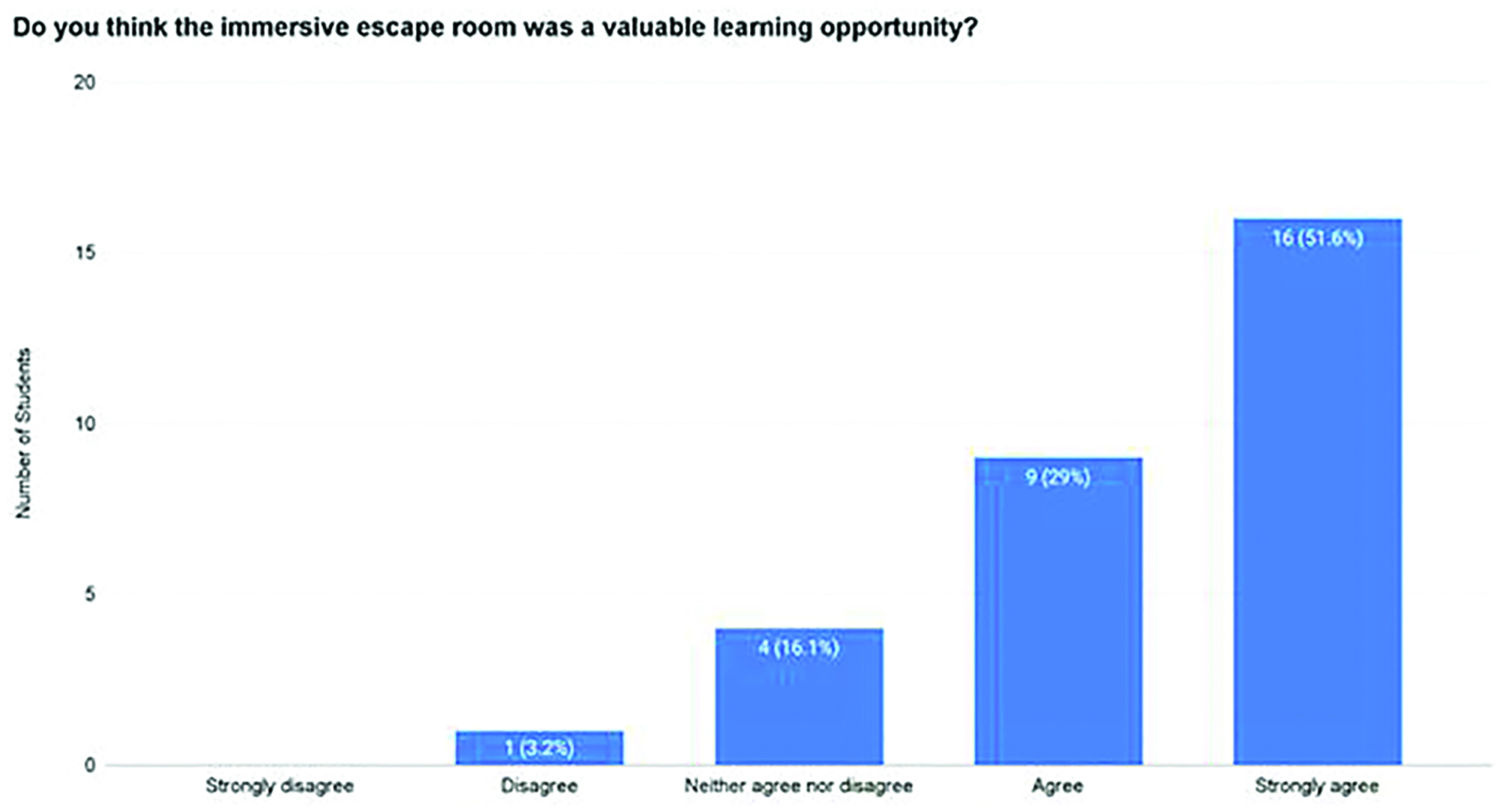
Akshay Doshi 1, Cameron Niven 1
[1]
Case-based learning (CBL) is a widely used teaching method, promoting clinical reasoning and application of knowledge through structured scenarios (1). Developing high quality CBL materials requires significant expertise and resources. Recent advances in Artificial Intelligence (AI) offer the potential to streamline this process, yet its effectiveness in producing high quality educational material is uncertain. This study aimed to evaluate whether CBL scenarios produced by AI are comparable in quality to those written by experienced educators, based on expert review across key educational domains.
Five CBL scenarios were generated using ChatGPT, guided by a prompt based on learning objectives from an established series of educator-written CBLs. For each topic, an AI-generated case and a corresponding educator-written case aligned to the same objectives were evaluated. Four experienced medical educators independently assessed each case using a five-point Likert scale across key domains: clinical accuracy, alignment with learning objectives, structure, educational value, and usability for teaching. Evaluators were blinded to the source of each case. The AI prompt was iteratively refined prior to final case creation to ensure structural comparability between AI-generated and educator-written CBLs.
AI-generated CBL scenarios were comparable in quality to educator-written cases across all evaluated domains, with no statistically significant differences observed. Educator-written cases scored slightly higher in clinical accuracy (mean 4.45 vs 4.30, p=0.12) and educational value (mean 4.45 vs 4.00, p=0.09), while AI-generated cases scored marginally higher for alignment with learning objectives (mean 4.45 vs 4.30, p=0.68). Overall, AI-generated cases demonstrated a similar standard of clinical accuracy, educational value, alignment with learning objectives, structure, and usability.
AI-generated educational materials do not depend on access to conventional teaching resources, which require significant expertise and time to produce. Our findings suggest that AI can generate CBL scenarios of comparable quality to those written by medical educators, promoting global access to medical education, particularly in regions with limited infrastructure. The ability to rapidly generate structured CBLs with minimal input highlights the potential for scalable implementation in diverse educational settings.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Holland JC, Pawlikowska T. Undergraduate Medical Students’ Usage and Perceptions of Anatomical Case-Based Learning: Comparison of Facilitated Small Group Discussions and eLearning Resources. Anat Sci Educ. 2019 May;12(3):245–256. doi: 10.1002/ase.1824. Epub 2018 Oct 30. PMID: 30378294.
Mohamed Shirazy 1, Emma GreenWood 2, Lousie McKee 2, Nicola Weatherup 2
[1]
[2]
Managing anticoagulation in emergencies requires swift decisions, collaboration, and precision. Despite existing guidelines, real-world practice often suffers from delays and inconsistencies. This Quality Improvement Project (QIP) at the Royal Victoria Hospital (RVH) used in situ simulation combined with a novel debriefing model integrating, Figure 1:
Scottish Debrief Model – for emotional processing and team reflection.
SEIPS framework – to analyse system-level safety factors.
i-SOG – to highlight gaps between intended and actual workflows.
This structured debriefing enabled identification of performance and system issues while aligning with the four Meta-Debriefing pillars:
Theory-based – rooted in established models.
Psychologically safe – fostering open discussion.
Context-dependent – focusing on ED-specific anticoagulation challenges.
Formative – driving practical improvements and learning.
Three in-situ simulation sessions simulated major haemorrhages in anticoagulated patients. ED doctors, nurses, and pharmacists participated; senior clinicians and QI leads observed. Each session was followed by structured debriefs assessing: Individual/team performance (Scottish Model), System inefficiencies (SEIPS), and Workflow discrepancies (i-SOG).
First simulation exposed major issues:
Delays due to poor access to reversal agents
Uncertainty around guideline interpretation
Environmental constraints like poor layout
Interventions included:
Improved drug storage and accessibility
Simplified, more visible guidelines
Environment redesign for better workflow
Targeted team training
Second simulation (post-intervention):
Better protocol adherence
Quicker, more confident drug handling
Stronger communication and teamwork
Third simulation (with new pathway):
Marked improvement in protocol compliance
Reduced drug preparation delays
Closure of key workflow gaps
This debrief model provided a comprehensive view of individual and system-level issues. It led to the creation of a practical, ED-specific anticoagulation reversal pathway, addressing both human and systemic challenges. The method upheld the four Meta-Debriefing principles, ensuring simulations were safe, relevant, and improvement-oriented.
By validating the interventions through measurable improvements, this approach proved effective. It offers a scalable model for embedding into routine emergency training, enhancing clinician readiness, workflow efficiency, and patient safety in high-risk scenarios.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Holden RJ, Carayon P, Gurses AP, Hoonakker P, Hundt AS, Ozok AA, Rivera-Rodriguez AJ. SEIPS 2.0: a human factors framework for studying and improving the work of healthcare professionals and patients. Ergonomics. 2013 Nov 1;56(11):1669–86.
2. Patterson MD, Geis GL, Falcone RA, LeMaster T, Wears RL. In situ simulation: detection of safety threats and teamwork training in a high risk emergency department. BMJ quality & safety. 2013 Jun 1;22(6):468–77.
3. Kumar P, Collins K, Oliver N, Duys R, Park-Ross JF, Paton C, Laws-Chapman C, Eppich W, McGowan N. Exploring the Meta-debrief: Developing a Toolbox for Debriefing the Debrief. Simulation in Healthcare. 2024 Oct 17:10–97.
We would like to extend our sincere gratitude to the Emergency Department team at the Royal Victoria Hospital for their invaluable support and collaboration throughout this Quality Improvement Project. Their commitment to excellence, openness to innovation, and active participation in simulation-based learning were instrumental in driving meaningful change. This work would not have been possible without their enthusiasm, expertise, and dedication to improving patient safety and clinical practice.

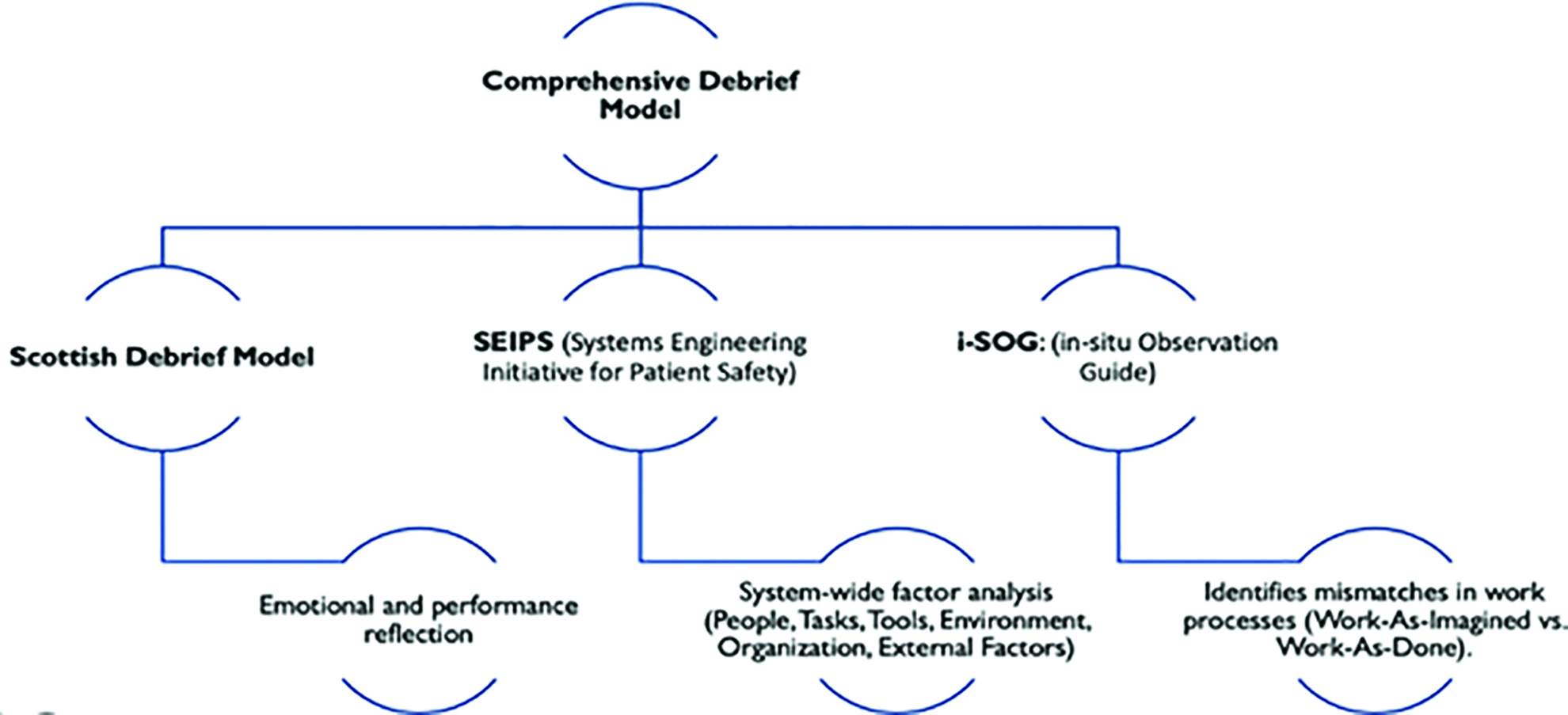
Radhika Kumar 1, Amy Ireson 1
[1]
Cardiac arrests, though rare in District General Hospitals (DGHs), require effective team performance. Studies show that each minute of delay in delivering the first shock during out-of-hospital ventricular fibrillation cardiac arrest decreases the probability of survival to discharge by 6% [1].
During our monthly in-situ simulation program, we identified a potential delay to shock delivery with delayed connection of defibrillator pads. Using the SEIPS framework [2] we aimed to explore both equipment and workflow inefficiencies.
Simulations were conducted to quantify the delay, using a CPR training manikin, defibrillator training pads, and staff’s own ward defibrillators. Thirty staff members participated, with a range of seniorities and specialities, all holding current Immediate or Advanced Life Support certificates (and hence trained to use a defibrillator).
Time was recorded from pad application to connection and activation of the defibrillator in seconds. The primary outcome was connection time, with the aim of all staff carrying out the task in under 60 seconds. Secondary outcomes included perceived cognitive load, assessed via informal debriefs.
Repeated cycles introduced system-based interventions to reduce connection time. Staff roles and experience levels were similar across cycles, with 30 different participants in each.
The first cycle revealed an average connection time of 62 seconds (range: 10–205 seconds). Staff had no difficulty placing pads but consistently struggled to locate the connection port. In the second cycle, coloured labels (“attach pads here”) were added (see Figure 1) with the aim of making identification of the connection site easier. Surprisingly, average connection time increased to 96 seconds (range: 6–300 seconds) in this cycle.
Debriefs with staff members revealed not only a significant cognitive load, but also real-life stories of how difficulty connecting pads had impacted actual cardiac arrests – with some staff expressing significant guilt over not knowing how to connect the pads at the time.
This study revealed that the task of pad connection was a common difficulty for staff, and that simple interventions were ineffective at reducing time to pad connection. A decision was subsequently made at trust level to procure pre-connected pads to eliminate the task entirely.
By addressing the issue at a system level - through redesign rather than retraining - we aim to improve patient safety and reduce staff cognitive burden in the long-term.
This project is highly transferable to other hospitals and demonstrates the value of a systems-based approach to simulation learning and quality improvement.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Stieglis R, Verkaik BJ, Hanno LT, Koster RW, van Schuppen H, van der Werf C. Association between delay to first shock and successful first-shock ventricular fibrillation termination in patients with witnessed out-of-hospital cardiac arrest. Circulation. 2024;151(3). doi: 10.1161/CIRCULATIONAHA.124.069834.
2. NHS England. SEIPS quick reference and work system explorer. Version 1. [Internet]. 2022 [cited 2025 Apr 14]. Available from: https://www.england.nhs.uk/wp-content/uploads/2022/08/B1465-SEIPS-quick-reference-and-work-system-explorer-v1-FINAL.pdf
Acknowledge: Billy Perrin, Resuscitation Lead at Homerton Healthcare NHS Foundation Trust

Radha Brown 1, Kelly Russell 1, Anthony Richardson 1, Rachel Murdoch 1, Priyanka Das 1
[1]
Analysis of patient safety incidents and complaints is an essential form of learning for healthcare institutions, with harm to patients having major human, moral, ethical and financial implications¹. In response to common and repeated incidents, weekly in-situ simulation-based education has been implemented on the Older Persons’ Medicine (OPM) ward to enhance learning amongst the multidisciplinary team. The team included Doctors, Nurses, Healthcare Assistants and Advanced Nurse Practitioners.
• To enhance staff engagement with the learning from incidents process, reducing repeated incidents on the following topics: seizures, pulmonary embolism, rapid tranquilisers, hypoglycaemia and opiate toxicity.
•To improve multidisciplinary team technical and non-technical skills and knowledge.
This was a prospective study to deliver in-situ simulation to an OPM ward at a tertiary NHS hospital based on repeated clinical incidents that took place between 2022 and 2024. A pilot session was carried out for 3 months, and simulation-based education and psychological safety rules for debriefing were introduced to the staff. Weekly in-situ simulation training was delivered for 2 years.
Incidents and complaints were collected via the incident recording system. In-situ simulation training was implemented where the multidisciplinary staff were allocated protected time weekly for simulation training. Scenarios were created based on repeated incidents and each scenario was delivered for a month to capture all the staff on the department. Feedback from staff was collected via QR code after sessions and staff were empowered to suggest service improvement initiatives within their feedback questionnaire. Feedback was reviewed and ward managers instigated the necessary changes suggested by the staff.
Debriefing is undertaken after the scenario delivery to reinforce individual learning. Alongside weekly in-situ simulation, an unannounced drill is performed twice a year on scenarios that have been previously delivered to ensure staff are retaining knowledge.
Using in-situ simulation has been incredibly well received by ward staff. The team showed a willingness to learn through simulation. Feedback amongst staff is very positive, Table 1.
90% of staff in the department are now trained, inclusive of staff on long-term absence and new recruits. The impact of the training has resulted in a decrease in repeated incidents from 5 cases in 2022 to 1 incident in 2024.
Simulation has proven its impact on limiting the number of patient safety incidents and complaints, thus improving patient care.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable
1. Panagioti M, Khan K, Keers RN, Abuzour A, Phipps D, Kontopantelis E et al. Prevalence, severity, and nature of preventable patient harm across medical care settings: systematic review and meta-analysis. BMJ. 2019;366:l4185. doi: 10.1136/bmj.l4185.

| Location | Participants | Feedback |
|---|---|---|
| Both wards on older persons’ medicine. | 90% Nursing, Health Care Nursing, and Doctors. | “I feel that having the training on the actual ward where I work was very beneficial as it added to the atmosphere of trying to work in a busy clinical environment.” “Really good session as difficult to access some training due to ward pressures. Also the session being catered to our specialty is better for staff to increase their knowledge and skill set” “Do more!” |
Daniel Raison 1, Caroline Evenden 2
[1]
[2]
Opioid analgesia remains a key pharmacological option for the management of post-operative pain [1]. Preventing and recognising adverse events associated with opioid analgesia is vital, due to the risk of life-threatening sedation and respiratory depression. Nurses play an important role in the recognition and initial management of these patients.
Simulation-based education (SBE) has been shown to have a significant positive effect as a training strategy for nurses [2]. Here, we aim to determine whether SBE, delivered in a ward environment, can increase nurses’ knowledge and confidence in managing patients with opioid toxicity with respiratory compromise.
Over a period of five weeks SBE was delivered to nurses in their clinical areas using small group point-of-care (POC) simulation. The simulation included both a simulated participant and a task-trainer airway head to perform airway manoeuvres. Learners were provided with basic monitoring equipment, simple airway adjuncts and patient-specific paperwork. The scenario was facilitated and debriefed by experienced simulation faculty.
A feedback survey was carried out using a QR code immediately after the scenario. A follow-up survey was emailed to the participants two weeks after the final simulation. They comprised the same five questions: 1) knowledge of opioid toxicity (including theory and risk factors); 2) confidence in recognising opioid toxicity; 3) basic airway management; 4) managing opioid toxicity; 5) administering naloxone if prescribed appropriately. Candidates were asked to complete a five-point Likert scale before the simulation, immediately after the simulation and in the follow up survey.
Wilcoxon signed-rank test was performed on survey responses to each question to determine whether there were significant differences between: 1) before and after the simulation 2) before the simulation and follow-up.
A total of seven registered nurses attended a simulation session over the five weeks. All attendees completed the survey immediately after the session and six at the follow-up questionnaire. The follow-up questionnaire was completed at two to six weeks after the simulation. The results are summarised in Table 1.
Four out of five of the questions in the survey immediately after the session, and three out of five at follow-up, showed a significant increase in value. This shows the POC simulation increased knowledge and confidence in the recognition and management of opioid toxicity. Despite the benefits demonstrated, the limitations of this project included staff availability, the length of time the training could be offered and the number of survey responses.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable
1. Jarzyna D, Jungquist CR, Pasero C, et al. American Society for Pain Management Nursing guidelines on monitoring for opioid-induced sedation and respiratory depression. Pain Manag Nurs. 2011;12(3):118–45.e10. doi: 10.1016/j.pmn.2011.06.008.
2. Hegland PA, Aarlie H, Strømme H, Jamtvedt G. Simulation-based training for nurses: Systematic review and meta-analysis. Nurse Educ Today. 2017;54:6–20. doi: 10.1016/j.nedt.2017.04.004.

| Number of responses | Mean (range) | Standard deviation | z-value (compared to before) | p-value* (compared to before) | |
|---|---|---|---|---|---|
| 1) Knowledge | |||||
| Before | 7 | 3.57 (3–5) | 0.787 | --- | --- |
| After | 7 | 4.57 (4–5) | 0.535 | 2.377 | 0.0174 |
| Follow-up | 6 | 4.17 (4–5) | 0.408 | 2.236 | 0.0253 |
| 2) Recognition | |||||
| Before | 7 | 3.57 (2–4) | 0.787 | --- | --- |
| After | 7 | 4.71 (4–5) | 0.488 | 2.53 | 0.0114 |
| Follow-up | 6 | 4.16 (3–5) | 0.753 | 1.41 | 0.1585 |
| 3) Airway management | |||||
| Before | 7 | 3.71 (2–5) | 0.951 | --- | --- |
| After | 7 | 4.71 (4–5) | 0.488 | 2.377 | 0.0174 |
| Follow-up | 6 | 4.33 (4–5) | 0.516 | 1.964 | 0.0495 |
| 4) Management | |||||
| Before | 7 | 3.71 (2–5) | 0.951 | --- | --- |
| After | 7 | 4.42 (3–5) | 0.787 | 1.673 | 0.0944 |
| Follow-up | 6 | 4.50 (4–5) | 0.548 | 2.169 | 0.0301 |
| 5) Naloxone | |||||
| Before | 7 | 3.86 (1–5) | 1.345 | --- | --- |
| After | 7 | 4.86 (4–5) | 0.378 | 1.976 | 0.0482 |
| Follow-up | 6 | 4.83 (4–5) | 0.408 | 1.732 | 0.0833 |
Amy Ireson 1, Sini John 1, Linnie Pontin 1, Rachel Thomas 1, Susanne Dekker 1
[1]
The introduction of the Patient Safety Incident Response Framework (PSIRF) marked a shift in how patient safety incidents are reviewed. Although external training opportunities are available, staff feedback highlighted a need for more practical understanding of PSIRF and human factors. To address this, we developed a bespoke, financially sustainable course, enabling staff to engage interactively with the changes in PSIRF. A key focus was on preparing staff to carry out swarm huddles, as the new learning response with the most local ownership.
In collaboration with the patient safety team, the simulation team designed a full-day course combining lectures, workshops, and simulations to explore human factors and systems thinking (using the SEIPS tool [1]) before scaffolding this knowledge to carry out swarm huddles. We began with non-clinical examples such as “A Cup of Tea” developed by Epsom + St Helier [2], before progressing to analyse clinical scenarios using SEIPS. We created two videos of clinical scenarios: a deteriorating patient and a misplaced naso-gastric tube [3]. Participants then had the opportunity to conduct a swarm huddle with the involved characters, played by faculty members.
Success was evaluated through post-training surveys, qualitative feedback, and observed improvements in incident response.
To date, 62 senior staff from diverse roles, including acute, community and non-clinical staff, have attended the training. 84% of attendees completed a post-course survey, leading to ongoing adaptations in course content.
Feedback included Likert scale assessments of confidence as well as qualitative comments. Attendees highlighted the cultural shift that the course contributed towards, commenting:
“Fostering an environment where staff feels safe to be a part of the learning process”
“More talking and bringing people together,”
“A focus on meaningful actions that genuinely demonstrate learning.”
A new swarm huddle template, developed during the course, is now used across the Trust. Staff, including those from the emergency department, have fed back successes of carrying out swarm huddles to learn from both events that have gone well and less well.
While PSIRF focuses on patient safety, it also promotes a just culture centred on systems thinking and continuous improvement. This approach moves teams away from a blame culture and fosters unity across the Trust. Our program has garnered attention beyond our Trust, with positive feedback from organisations including North London Hospice and NHS England South-West, particularly regarding the simulated videos. The course is being peer reviewed for quality assurance.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable
1. NHS England. SEIPS quick reference and work system explorer. Version 1. [Internet]. 2022 [cited 2025 Apr 14]. Available from: https://www.england.nhs.uk/wp-content/uploads/2022/08/B1465-SEIPS-quick-reference-and-work-system-explorer-v1-FINAL.pdf
2. Epsom + St Heliers NHS. SEIPS Just a cup of tea [Video]. YouTube; 2023 [cited 2025 Apr 14]. Available from: https://www.youtube.com/watch?v=3Svf6auw9_s
3. Homerton Digital Learning. SEIPS Training videos [Playlist]. YouTube; 2025 [cited 2025 Apr 24]. Available from: https://www.youtube.com/playlist?list=PLuRc8vhK-AYglxw76Z9R2eBMqaW36vIrL
Jessica Casey 1, Swati Gupta 2, Kitt Richardson 1, Natalie Hay 1, Hazel Luck 1, Frances Verey 1
[1]
[2]
The provision of major trauma resuscitation in the emergency department (ED) is a life-saving, time-critical multidisciplinary (MDT) process that is susceptible to latent safety threats (LSTs). Testing the system response using simulation can yield valuable lessons for improving patient safety [1]. No ‘blueprint’ currently exists to guide planning and delivery of this quality improvement (QI) process within NHS acute EDs that form part of major trauma networks (MTNs). This project aimed to develop and pilot a replicable strategy for delivering in-situ simulation to test and improve trauma resuscitation systems.
The strategy development process involved attending relevant webinars and reviewing the existing literature on transformative simulation in critical care scenarios, including resources from specialist interest groups of the Association for Simulated Practice in Healthcare [2]. Areas targeted as needing creative solutions included how to formally conduct a needs assessment, identify barriers to delivery and select relevant outcome measures to assess impact. A steering group was formed via a collaborative approach with the SouthWest MTN, local and regional simulation services and the local ED. The project was registered with the QI department at the regional major trauma centre and a pilot was conducted.
Process mapping and timeline development were undertaken. Early stakeholder engagement was deemed crucial and these were identified as trauma leadership, clinical teams, and support services such as transfusion and radiology. Needs assessment methods included focused stakeholder discussions and examination of local critical incident reporting systems. Key planning decisions included participant pre-briefing, consent considerations, and digital recording. A plan-do-study-act (PDSA) QI methodology guided the simulation, which identified LSTs using a Systems Engineering Initiative for Patient Safety (SEIPS) framework [3], measured performance timescales, assessed adherence to national trauma registry audit standards and captured participant satisfaction using a tailor-made survey. Final stages included scenario design and resource coordination. Debriefing used a SEIPS-based chronological analysis. The pilot delivered at the local major trauma centre identified 11 actionable recommendations and generated strong participant satisfaction.
Further work planned includes repeating the simulation after implementation of these recommendations to assess impact and complete the PDSA cycle. A delivery toolkit has been created to support the rollout of the QI project across all trauma units in the network. The strategy outlined above is adaptable and scalable, showcasing the creative intersection of simulation and QI in a busy NHS department. This approach has the potential to inform national simulation-based QI efforts in trauma care.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Petrosoniak A, Fan M, Hicks CM, White K, McGowan M, Campbell D, Trbovich P. Trauma Resuscitation Using in situ Simulation Team Training (TRUST) study: latent safety threat evaluation using framework analysis and video review. BMJ Qual Saf. 2021 Sep;30(9):739–746.
2. Binder C, Elwell D, Ackerman P, Shulman J, Yang C, Jafri F. Interprofessional In Situ Simulation to Identify Latent Safety Threats for Quality Improvement: A Single-Center Protocol Report. J Emerg Nurs. 2023 Jan;49(1):50–56.
3. Holden RJ, Carayon P, Gurses AP, Hoonakker P, Hundt AS, Ozok AA, Rivera-Rodriguez AJ. SEIPS 2.0: a human factors framework for studying and improving the work of healthcare professionals and patients. Ergonomics. 2013;56(11):1669–86.
Suzanne Scaffardi 1
[1]
A quality improvement (QI) project using in-situ simulation (ISS) was undertaken at a Cardiac catheterisation laboratory (CCL) in a London teaching hospital. The CCL provides 24-hour primary percutaneous coronary intervention (PPCI) for patients having a heart attack and is a lifesaving treatment. Cardiac arrest can happen during the procedure as a heart attack complication.
Guidance released in 2021 [1] advocates early use of a mechanical cardiopulmonary resuscitation (M-CPR) device after the first cycle of CPR meaning PPCI can continue as it is safe to deliver fluoroscopy, which may facilitate treatment intervention for the potential cardiac arrest reversible cause. A baseline audit showed this was not happening.
Institute of Health Improvement (IHI) Model for Improvement QI approach was utilised alongside in-situ simulation (ISS) over 6 months, the aim statement was to apply M-CPR device during cardiac arrest in the CCL after 1st cycle of CPR.
A scoping survey to understand multi-disciplinary staff opinion and experience from cardiac arrests in the CCL was displayed in Pareto charts to target high impact change ideas.
Plan-Do/Simulate-Study-Act (PDSA) cycles using inter-disciplinary ISS and simulation debrief, using PEARLs for systems integration tool [2], allowed exploration of staff lived experience, training gaps, system issues, latent threats, and potential solutions.
Run charts were used to capture data and ISS pre and post questionnaires for training evaluation.
The M-CPR device became consistently used after 1st cycle of CPR and a shift on the run chart was seen.
There was statistical (SPSS 27) significance from simulation evaluation in increase in confidence in leadership (p<.001) and speaking up (p<.001) at cardiac arrests in the CCL.
Improvement ideas were developed from simulation debriefing.
QI methodology and MDT ISS facilitated greater understanding of contextual issues of system interaction and the human side of change. It supported a team approach and provided a voice for staff.
Increasing staff confidence and speaking up during a cardiac arrest was not part of the original project aims but demonstrates how simulation has supported behaviour traits of leadership and communication, by making staff feel more confident to act in real life and initiate the “right things” to happen.
PDSA cycles demonstrated how education is not enough to impact a change in practice. This is an important consideration in the value of what ISS can offer organisations in terms of learning about everyday work and supporting learning to enact change.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Dunning J, Archbold A, De Bono JP, Butterfield L, Curzen N, Deakin CD, et al. Joint British Societies’ guideline on management of cardiac arrest in the cardiac catheter laboratory. Heart. 2022;108(12):E3.
2. Dubé MM, Reid J, Kaba A, Cheng A, Eppich W, Grant V, et al. PEARLS for Systems Integration: A Modified PEARLS Framework for Debriefing Systems-Focused Simulations. Simulation in Healthcare: The Journal of the Society for Simulation in Healthcare. 2019;14(5):333–342
Barah Hassan 1, Jenna Gillone 1
[1]
Workplace incivility is a pervasive issue in healthcare, negatively impacting staff well-being, teamworking, cognitive load and patient safety [1]. Traditional training may not capture specific human factor or patient safety elements related to incivility. This project aims to evaluate the effectiveness of an innovative, multidisciplinary simulation-based intervention designed to increase awareness of incivility and its impact on patient safety within the NICU.
A prospective design was used in preparing and planning the scenario [2,3]. The simulation ran during a structured teaching session, with participants of various nursing and medical grades from the NICU. In total there were 4 participants with 3 confederates in the simulation and 21 observers. A learning conversation was guided by 4 experienced debriefers, 1 of whom was a confederate.
The multidisciplinary team participated in a high-fidelity simulation depicting a patient handover with an array of embedded uncivil behaviours enacted by and towards pre-briefed confederates. Participants were briefed to receive handover but not briefed around the central theme of incivility. Their experience and response to witnessing incivility was the central driver for the learning conversation. Psychological safety was considered through confederate training and structured debriefing immediately post-simulation.
Feedback was collected via direct observation during the simulation, analysis of debriefing, and anonymous post-simulation surveys assessing realism, learning and perceived changes in awareness and preparedness.
Observation confirmed realistic enactment of incivility and notable bystander passivity among participants. Post-event analysis demonstrated increased participant recognition of incivility, understanding of its link to communication breakdown and cognitive load, and crucially, a connection drawn between the simulated incivility and a patient safety. Survey data indicated high perceived realism and educational value, particularly for the debriefing. Participants reported significantly increased awareness of incivility and its impacts, alongside increased (though less pronounced) preparedness to address it.
The simulation effectively increased awareness of incivility and vividly demonstrated its potential patient safety consequences within a realistic NICU context. The link was made to potential patient care errors and impact on cognitive load, underscoring mechanisms by which incivility impacts care. Observed bystander passivity highlights potential cultural challenges requiring further attention, but the inherent difficulty associated with challenging incivility. The findings support immersive simulation as an effective educational strategy for this sensitive topic but emphasise the absolute necessity of psychological safety for participants and observers throughout design and implementation. This intervention provides a valuable model adaptable to other healthcare settings seeking to foster civility and improve safety.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Van Heugten K, Casler K, Sharplin E. The prevalence of incivility in hospitals and the effects of incivility on patient safety culture and outcomes: A systematic review and meta-analysis. J Adv Nurs. 2024 Mar 22. doi: 10.1111/jan.16111. Epub ahead of print. PMID: 38515008.
2. Rudolph JW, Raemer DB, Simon R. Establishing a safe container for learning in simulation: the role of the presimulation briefing. Simul Healthc. 2014 Dec;9(6):339–49. doi: 10.1097/SIH.0000000000000051. PMID: 25119147.
3. Cook DA, Hatala R, Brydges R, Zendejas B, Szostek JH, Wang AT, Erwin PJ, Hamstra SJ. Technology-enhanced simulation for health professions education: a systematic review and meta-analysis. JAMA. 2011 Sep 7;306(9):978–88. doi: 10.1001/jama.2011.1234. PMID: 21900138.
Kirsten Howson 1, Carrie Hamilton 1, Erin Power 2, Caroline Tomkins 1, Nichola Martin 1
[1]
[2]
A sense of belonging within the National Health Service (NHS) workforce is imperative in establishing a safe and effective working environment, as outlined in the NHS People Plan (2020) [1], ‘The NHS must welcome all, with a culture of belonging and trust. We must understand, encourage and celebrate diversity in all its forms’ (p.24). It can be challenging to establish a sense of belonging within the NHS where large teams are working under high pressures in inconsistent shift patterns. Incorporating lived experiences, a simulation workshop was designed to enhance participants’ knowledge and understanding of how to foster workplace belonging when interacting with colleagues with protected characteristics.
The workshop was delivered twice and opened with an introduction, explaining the use of simulation, how scenarios will run, the timetable and an ice breaker, establishing psychological safety. The workshop contained a diverse variety of simulated scenarios, using a range of simulation techniques, including, observed simulation, forum theatre and character monologues. The scenarios focused on working alongside colleagues with a range of protected characteristics, including those with caring responsibilities, age and faith.
The scenarios were followed by reflective debriefs, led by experienced facilitators, providing a psychologically safe space in which to explore the pre-set learning objectives, reflections, feelings and previous experiences.
Two separate communication frameworks were shared with participants in order to assist them in preparing for supportive conversations. These are: STEPS (Start, Time, Empathy, Provision of Support, Sense Check) [2] and CUS (Concerned, Uncomfortable, Safety) [3] and Clean Feedback [4].
Pre- and post-course rating scale evaluations were used following workshop delivery in April and May 2024, focussing on the individualised workshop learning outcomes, alongside free-text responses and were completed by a total of 9 participants. The feedback demonstrated an improvement in knowledge on the topics covered, with 46% of the participants expressing limited, neutral or no knowledge before the workshop and 99% expressing excellent or good knowledge after the workshop. Qualitative feedback highlighted the reflective value of the workshop, in addition to the authenticity of the scenarios, which were described as “real-life.”
The feedback supports the use of simulation training, containing embedded communication models in enhancing the ability of NHS employees to support colleagues with protected characteristics, in turn fostering a sense of belonging amongst the workforce. Specific feedback focussed on the value of ensuring that scenarios are authentic.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. NHS England. WE ARE THE NHS: People Plan 2020/21 - Action for Us All [Internet]. NHS England. NHS England; 2020. Available from: https://www.england.nhs.uk/wp-content/uploads/2020/07/We-Are-The-NHS-Action-For-All-Of-Us-FINAL-March-21.pdf
2. Hamilton C, Thame A, Spencer J. A78 STEPS: Development of a communication skills framework for use in a broad range of simulation-based education. International Journal of Healthcare Simulation. 2023 Oct 31.
3. Agency for Healthcare Research and Quality. Tool: CUS | Agency for Healthcare Research and Quality [Internet]. www.ahrq.gov. 2023. Available from: https://www.ahrq.gov/teamstepps-program/curriculum/mutual/tools/cus.html
4. Doyle, N. (2008). Cleaning up the ‘F’ word in coaching – cleanlanguage.com. [online] Cleanlanguage.com. Available at: https://cleanlanguage.com/cleaning-up-the-f-word-in-coaching/. Accessed 8 April 2025.
Joanne Davies 1, Julia Terry 1, Ioan Humphreys 1, Rachel Wilks 1
[1]
Following funding from the Morgan Advanced Studies Institute (MASI) a pilot study was conducted with expertise from the SUSIM Simulation and Immersive Learning Centre at Swansea University.
Healthcare professionals often lack the training and confidence to communicate effectively with d/Deaf patients, leading to miscommunication, reduced trust, and poorer health outcomes. Traditional simulation-based education (SBE) programmes rarely reflect the lived experiences of d/Deaf individuals or include British Sign Language (BSL) and deaf culture [1,2]. This project aimed to address this gap through the co-creation of immersive Virtual Reality (VR) learning modules with the d/Deaf community. The research question was: How can immersive simulation technologies be co-designed with the d/ Deaf community to enhance student understanding and inclusive communication in healthcare?
Using an inclusive, values-led approach, the research team collaborated with d/Deaf community members, BSL interpreters, and healthcare students to co-design a suite of computer based and virtual reality (VR) learning packages. A series of structured workshops facilitated open dialogue about lived experiences in healthcare, barriers to communication, and priorities for professional education. Insights from these sessions directly informed scenario design, scripting, and visual storytelling. VR content was developed using 360° video, with bilingual (BSL and English) integration and d/Deaf individuals portraying themselves within the simulations. Qualitative feedback was collected throughout the process from both community participants and students.
A series of workshops from May 2024 to July 2024, revealed strong themes around disempowerment, safety, and the emotional toll of exclusion in clinical settings. These narratives shaped two pilot VR modules focused on first point-of-contact healthcare encounters. Deaf participants reported feeling valued and empowered in the co-design process. Using a mixed methods approach preliminary pilot student feedback showed increased awareness of the communication needs of d/Deaf patients, increased empathy and appreciation for learning directly through immersive, patient-led scenarios. A key outcome was the creation of a culturally respectful and pedagogically sound set of VR modules now embedded in pre-registration curricula at Swansea University [3].
This initiative demonstrates that co-designed simulation with the Deaf community is both feasible and impactful. The approach moves beyond tokenistic inclusion to authentic collaboration, positioning lived experience as essential to the learning environment. The learner pilot highlighted the importance of cultural humility, developing simulation content that promotes thoughtful, patient centric reflection and care with VR enhancing their opportunity to experience realistic immersion.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Shank C, Foltz A. Health and Wellbeing for Deaf Communities in Wales: Scoping for a Wales-wide survey [Internet]. Bangor University; 2019 [cited 2025 Apr 18]. Available from: https://research.bangor.ac.uk/portal/files/26546430/PHW_Health_and_Wellbeing_for_Deaf_Communities_in_Wales_Report_ENG.pdf
2. Terry J, Meara R. A Scoping Review of Deaf Awareness Programs in Health Professional Education. Plos Global Public Health. 2023. Available from: https://journals.plos.org/globalpublichealth/article?id=10.1371/journal.pgph.0002818
3. Terry J, Davies J, Wilks R, et al. Enhancing empathy and understanding; developing a virtual reality simulation to educate healthcare students on deaf patient experiences. Journal of Clinical Simulation in Nursing. [Under review].
Funding from the Morgan Advanced Studies Institute (MASI). Special thanks to - The amazing d/Deaf Community Focus Groups, BSL-using steering group members for all of their time and expertise; and BSL/English interpreter colleagues. The MSc Virtual reality students and staff team for the CGI development. RESCAPE for donating resources and filming time alongside the donated resources and expertise of the SUSIM team.
Swansea University Interprofessional Education Lead Nikki Williams for promoting the student pilot.
The project contribution of SU faculty: Ted Thomas, Sebastian Vowles, Julian Hunt, Deborah Rowberry,
Martin Nosek

| Lack of healthcare staff awareness about interpreter provision | Poor communication | Stereotypes of deaf people | Impact of poor health staff Deaf awareness | Discrimination (specific acts) | Positive suggestions to improve care for Deaf patients |
|---|---|---|---|---|---|
| Wi-Fi is a big issue when using remote interpreters |
Call name? reception call name, assume not present | Assuming I won’t complain or answer back | Being a patient (in-patient), very lonely and isolating | Refusal to wear a clear mask. Told me to ‘watch my behaviour’ | Ask patient what works well for them |
| Assumption of not needing an interpreter without clarification or communication |
I prefer to have it all written down, but their handwriting is terrible and not as detailed | Assumption – when you can talk | Lip reading is hard, when you are ill it’s worse | Interpreter being asked to wait outside as too many people in the room | Male interpreter for male patients, female for female especially if treatment is sensitive |
| No clue about how to book interpreter |
If they shout room number, then I don’t know | Patients feel that staff can revert to shouting, banging, poking instead of the medical notes being clear that the patient is Deaf and seeking an interpreter |
Issues of informed consent | Need a screen with name and room number and estimated wait times |
Esmé Ward 1, Dave Wright 1, Paul Sellens 1
[1]
When opening a new healthcare space, simulation based clinical systems testing allows for potential patient safety threats to be identified [1]. Translational simulation can be used in this context due to the focus on improving patient care and healthcare systems through diagnosing safety and performance issues and delivering simulation-based intervention [2].
The creation of a new paediatric day surgery centre required an interdisciplinary simulation programme designed to familiarise staff with the new environment and equipment, test systems and processes, and enhance team working both within and between departments. Clinical scenarios added focus on human factors and non-technical skills alongside strategies for improvement [3].
How can a simulation programme help prepare for the safe, functional operation of a new day surgery unit?
The two day in-situ simulation took place at the new Paediatric Day Surgery Unit at Castle Hill Hospital. Participants included anaesthetists, operating department practitioners, scrub, theatre and recovery staff and paediatric nurses, alongside wider hospital teams including outreach, porters, ambulance services, and blood transfusion. The programme involved various clinical and non-clinical scenarios focusing on testing the environment, processes and team-working. All scenarios included debriefing and discussion to raise main learning points and areas for improvement and change.
The simulation programme provided valuable insights and over fifty learning points or adjustments were identified. Patient safety threats highlighted included issues with emergency equipment location, familiarity and accessibility, unfamiliarity with novel equipment, availability of protocols for emergencies and transfer and communication between departments or teams. Emergency preparedness was significantly enhanced, with staff demonstrating increased confidence and competence in managing critical situations. Due to the in-situ nature of the simulation, many changes were able to be made on the day by the team directly impacted by them. Actions taken forward included further training sessions, equipment adjustments and process refinements.
The results indicate that the simulation programme was instrumental in identifying and avoiding potential patient safety risks within a new paediatric day surgery unit. Staff gained familiarity with the new environment, tested medical and non-medical equipment, and validated systems and processes. Hands-on experience and interdepartmental involvement ensured a thorough understanding of the unit’s layout and system functionality. The major conclusion is that simulation-based training is an effective strategy for enhancing patient safety, staff readiness, team working and operational efficiency in a new clinical setting. Future work will focus on implementing the identified actions and conducting follow-up evaluations to assess long-term impact.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Colman N, Doughty C, Arnold J, Stone K, Reid J, Dalpiaz A, et al. Simulation-based clinical systems testing for healthcare spaces: from intake through implementation. Advances in Simulation. 2019;4(19).
2. Brazil, V. Translational simulation: not ‘where?’ but ‘why?’ A functional view of in situ simulation. Advances in Simulation. 2017;2(20).
3. Kelly FE, Frerk C, Bailey CR, Cook TM, Ferguson K, Flin R, et al. Implementing human factors in anaesthesia: guidance for clinicians, departments and hospitals. Guidelines from the Difficult Airway Society and the Association of Anaesthetists. Anaesthesia. 2023;78:458–478.
Scarlet Herbertson 1, Carrie Hamilton 1, Caroline Tomkins 1, Kirsten Howson 1, Nichola Martin 1
[1]
Patient safety is a cornerstone of healthcare, and this principle extends to simulated patients/participants (SPs) who contribute to healthcare education. Ensuring their well-being is an ethical obligation that requires careful consideration of recruitment, role allocation, emotional impact, and ongoing support [1]. This innovation explores an ethical framework, produced with SPs, that prioritises their safety and well-being while maintaining the integrity of the educational event. Originally conceived in 2016 [2], this framework has since been refined, with multiple supportive tools, to enhance its effectiveness and applicability.
The framework is structured around the four key ethical principles: respect for autonomy, justice, non-maleficence, and beneficence [3]. A collaborative methodology was used to develop the ethical framework further. SPs, educators, and simulation experts have authored a suite of resources and processes which now support the efficacy of the framework, with due consideration of accessibility. These include an SP training video with content summary, updated recruitment practices, an understanding of expectations, feedback guidance using the CORBS model (clear, owned, regular, balanced, specific), and an aide memoire outlining key scenario formats and processes. Formal support mechanisms now include follow-ups for emotionally challenging roles, and a process of signposting to mental health services. Additionally, quarterly peer debrief sessions run, along with virtual peer mentoring between experienced and new SPs. A monthly tracker has been introduced to monitor engagement and gather feedback for continuous improvement.
The ethical framework and its associated documents have led to improved support mechanisms for SPs, with the aim of reducing distress and enhancing role satisfaction. Key outcomes include:
Improved recruitment and role alignment
Increased SP confidence and satisfaction in their roles
Reduction in reported emotional distress through structured debriefing, de-roling and support systems
Strengthened communication between educators and SPs
This framework aligns with the transformational simulation I’s: improvement, involvement, inclusion, identification and influence. The framework is deliberately structured to safeguard SPs while maintaining the authenticity of learning experiences, Figure 1.
Safeguarding SPs is as essential as protecting patients in healthcare education. Embedding SP safety through ethical recruitment, structured support, and peer-led governance improves outcomes for both SPs and learners. The transformative approach of integrating SP voices into their own governance has set a new benchmark for simulation-based education. Future development should aim to embed this framework across institutions, guided by the ASPiH standards and ASPE best practices.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Diaz-Navarro C, Laws-Chapman C, Moneypenny M, Purva M. The ASPiH Standards - 2023: guiding simulation-based practice in health and care. Available from: https://aspih.org.uk/
2. Hamilton C, Clarkson G, Perry J. O54 Child simulated patients: Being ethically responsible. BMJ Simulation & Technology Enhanced Learning. 2017;3:A36–A37.
3. Beauchamp TL, Childress JF. Principles of Biomedical Ethics (8th ed.). New York: Oxford University Press; 2019.
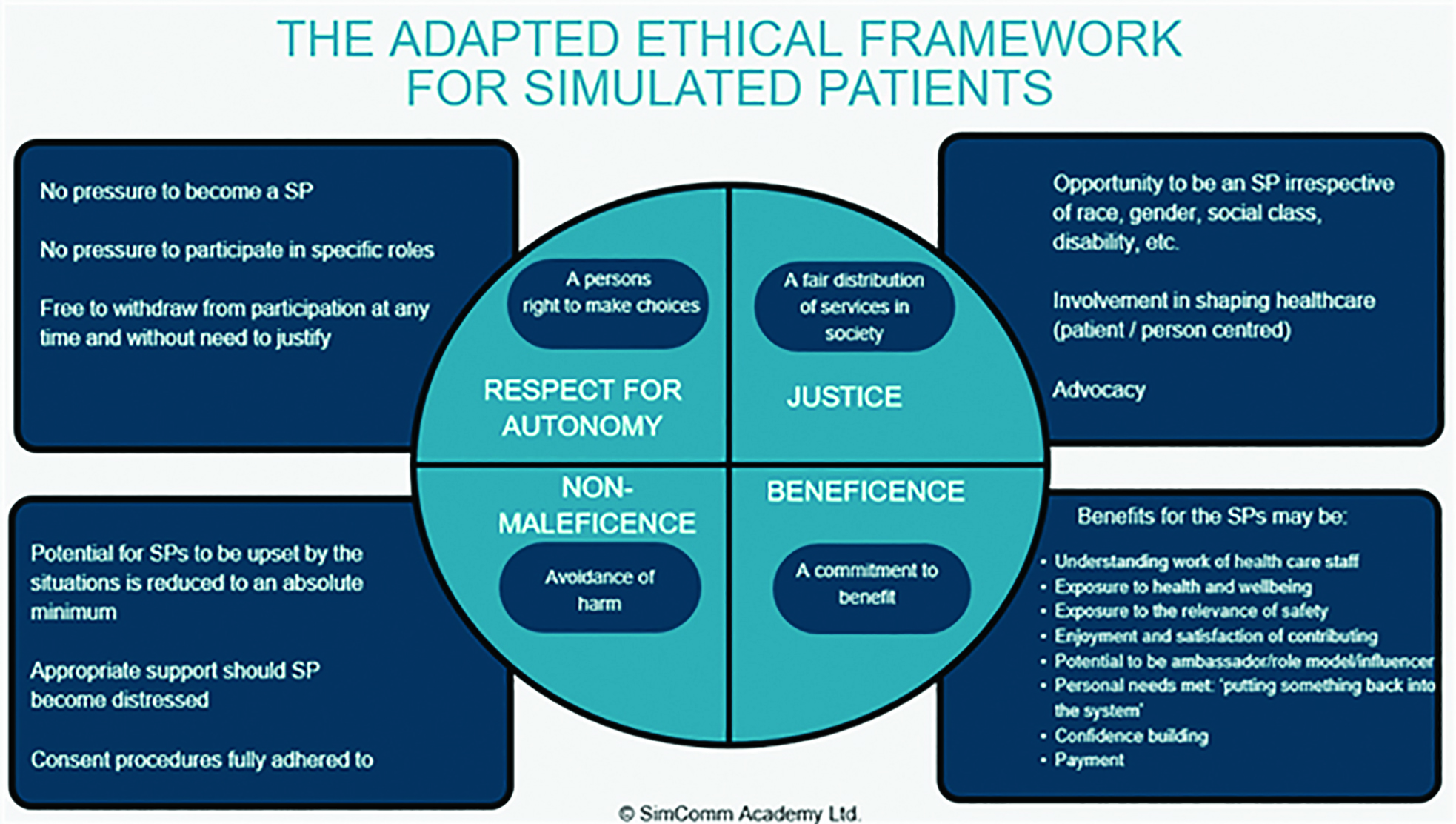
Emma Murray 1, Ashley Gillanders 1, Alix Murphy 1, Caroline Curry 1, Mary Molloy 1
[1]
Provision of safe perioperative care in remote theatre locations has many challenges. NAP 4 identified airway management in remote sites is associated with increased risk of morbidity and mortality [1]. Simulation training can aid preparedness to manage infrequent but highly critical events. Simulation training is often recommended following a critical events [2]. Insitu Simulation (ISS) undertaken in a clinical team’s own workplace provides a safe learning environment, improves team work and performance and identifies latent safety threats [3]. We organised ISS training in our dental DPU for the clinical team after review of learning needs and following recommendations from a critical event.
Protected time for ISS was secured through list cancellation in dental DPU. Scenarios were built around agreed learning outcomes (LOs) and specific critical events. Mannequins and portable simulation patient monitors were used. An eFONA workshop was also delivered. The ISS organised session was run twice, morning and afternoon to facilitate smaller groups and reflective of healthcare team working in theatre and recovery on a standard day. Each group rotated though scenarios in main DPU theatre, dental chair theatre and recovery. Scenarios included CICO, anaphylaxis, choking under sedation, post op bleeding in oral cavity and emergency airway management in recovery. Communications systems were tested to seek assistance from main hospital site. Each scenario was preceded by team brief and followed by structured debrief. Feedback questionnaire was distributed to team members after event.
Received an 80% response to the feedback survey. Those who responded 100% agreed or strongly agreed ISS was a psychologically safe learning environment.100% agreed or strongly agreed improved communication, team work, confidence, clinical skills and feeling of preparedness. Team members were able to identify areas for improvement and deficits in resources.
83% suggested ISS should be delivered more frequently, 50% indicated at least twice yearly.
Feedback indicates ISS was valuable to the clinical team in our dental DPU. Debrief sessions helped identify areas of latent safety threats and areas for improvement. Familiarising with airway drills and eFONA skills with the clinical team may be helpful in difficult airway management or CICO situation for any anaesthetist working alone in a remote setting.
Time pressures in clinical environments impede ISS which leads to difficulty in showing improvement in patient outcomes. However, if recommended in a critical event report this is a powerful tool for stakeholders to secure protected time for ISS training.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Wijesuriya J, Brand, J. Improving the safety of remote site emergency airway management. BMJ Quality Improvement Reports. 2014;2(2):1
2. Diaz-Navarro, Jones B, Pugh G et al. Improving quality through simulation; developing guidance to design simulation interventions following key events in healthcare. Advances in Simulation. 2024;9(30)
3. Gros E, Shi R, Hasty B et al. Insitu interprofessional operating room simualtions: Empowering learners in crisis resource management principles. Surgery. 2021;170(2):432–439
Bridie Jones 1, Clare Hawker 1, Sara Catrin Cook 1, Suman Mitra 1
[1]
Simulation plays a crucial role in healthcare by providing a controlled and risk-free environment for training, education, quality improvement, innovation and research. Funding is often required to support the resources needed including; faculty, equipment and/or technology, venues, scenarios and administrative support, amongst others to develop, establish and sustain the delivery of simulation activity. There is a need to clearly articulate the requirements, benefits and cost effectiveness of simulation to justify and secure investment. Additionally, there is a need to foster organisational ownership and buy in to help sustain simulation. Yet funding for this type of learning activity is finite and understanding and justifying costs can be challenging [1].
The Health Education Improvement Wales (HEIW) Simulation team hold a strategic, facilitatory and supportive role to the diverse multiprofessional simulation community across healthcare in Wales. Frequently the team are asked how and where funding can be sourced to support the development of simulation activity, as well as what rationale can be provided within any business case to justify any expenditure required.
In response, the HEIW team undertook a scoping review to determine potential funding sources external to the organisation that can be applied to/accessed by the simulation community across healthcare in Wales to support a range of simulation activity. A guidance document was developed providing a list of the identified potential sources as well as guidance on how to identify other potential sources of funding.
In addition, a narrative was developed based on a literature review of the benefits and impact of simulation activity, that could be used to support the development of a business case in application of funding for the use of simulation.
The narrative articulates the advantages of simulation in terms of staff development, patient safety, enhancing procedural skills, clinical decision-making, collaboration, teamwork and communication, alongside fostering innovation and quality improvement [2,3]. In particular, it emphasises the importance of simulation as an essential tool for workforce development and operational efficiency.
Funding may be crucial for some simulation projects as it allows the financing of a range of potential resources that may not already be available. Yet, to gain funding there needs to be an informed and detailed rationale demonstrating the significant value and impact of simulation.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable
1. Senvisky JM, McKenna RT, Okuda Y. (2025) Financing and Funding A Simulation Center. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK568786/
2. Sollid SJM, Dieckman P, Aase K, Søreide E, Ringsted C, Østergaard D. (2019) Five Topics Health Care Simulation Can Address to Improve Patient Safety: Results From a Consensus Process. Journal Patient Safety Jun;15(2):111–120. doi: 10.1097/PTS.0000000000000254. PMID: 27023646; PMCID: PMC6553986.
3. Dale-Tam J, Dale L. Using Simulation to Develop Clinical Reasoning Skills for Registered Practical Nurses New to Acute Care. Clinical Simulation in Nursing. 2024;86:101477. doi: 10.1016/j.ecns.2023.101477.
In February 2025 Newcastle Hospitals Trust ran a multi-disciplinary, multi-stage simulated exercise demonstrating care for a patient with a viral haemorrhagic fever (VHF). The exercise, entitled ‘Moulin Rouge’, followed on from work at the Royal Free Hospital, London (Exercise ‘Mamma Mia’), which conducted an exercise using a Trexler-based method of isolation and care in 2024 [1]. The Infectious Diseases (ID) team at Newcastle simulated a PPE-based care model to explore the relative challenges and benefits compared against the Trexler model.
To review the impact of a transformational simulation enabling practice and evaluation of effective procedures for providing peri-partum and neonatal care for a patient with a VHF.
The Trust’s Emergency Preparedness Resilience & Readiness (EPRR) lead anticipated that the exercise was likely to be large scale and that simulating the clinical elements would be essential. Planning closely followed the transformational simulation framework [2], with weekly design meetings attended by representatives of each department involved. Simulation representation from an early stage allowed for the appropriate targeting of simulation resources, as well as providing advice on the appropriate structuring of the four exercise scenarios taking place over two days.
The simulation team provided several key components: audio-visual (AV) support for the exercise, a neonatal manikin, and an extensively modified obstetric manikin to allow for caesarean-section, hysterectomy, and significant (4.5litres>) blood loss.
The AV support included pre-recorded video, alongside an unobtrusive multi-camera live stream, in-room audio and live narration, with patient observations inserted into the live stream as required. This enabled the large number of observers to participate in the debriefing discussions after each scenario.
The c-Section & hysterectomy modifications were developed and refined with expert obstetrics and gynaecology teams to ensure that they would be able perform in their role in as realistic a manner as possible.
Of the 100 attendees 33 completed the exercise evaluation form. Attendees were asked to grade on a Likert scale whether the exercise ‘did not meet’/’partially met’/’met’ stated objectives (Figure 1). Weighting for percentage = Not met 0%; partially met 50%; fully met 100%.
Moulin Rouge had nine stated objectives, seven of which required some level of clinical simulation (Figure 1). EPRR often utilises a less resource intensive ‘tabletop’ approach to deliver an exercise, however the inclusion of transformative simulation enhanced the debriefing discussion and highlighted unexpected human factor elements that may not have been noticed without it. Evaluations emphasise that the transformative simulation was vital in enabling a high-level discussion of the complex issues raised by the exercise objectives and will directly influence national discussion and policy around the management of patients with a VHF.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable
1. Alonso A, Cohen J, Cole J, Emonts M, Karunaharan N, Meadows C, O’Hara G, Owens S, Payne B, Porter D, Ratcliffe L, Riordan A, Ludwig-Schmid M, Sinha R, Tunbridge, Whittaker A E, Beadsworth M, Dunning J, and NHS England HCID Networks. ‘Clinical Management of Hospitalized Patients With High-Consequence Infectious Diseases in England’ Health Security 2024;22:S1,S50–S65
2. Gurnett P, Weldon S, Spearpoint K and Buttery A: ‘Transformative Simulation: To Patient Safety and Beyond’ in ‘Patient Safety: Emerging Applications of Safety Science’, 1st Ed. Class Publishing 2024

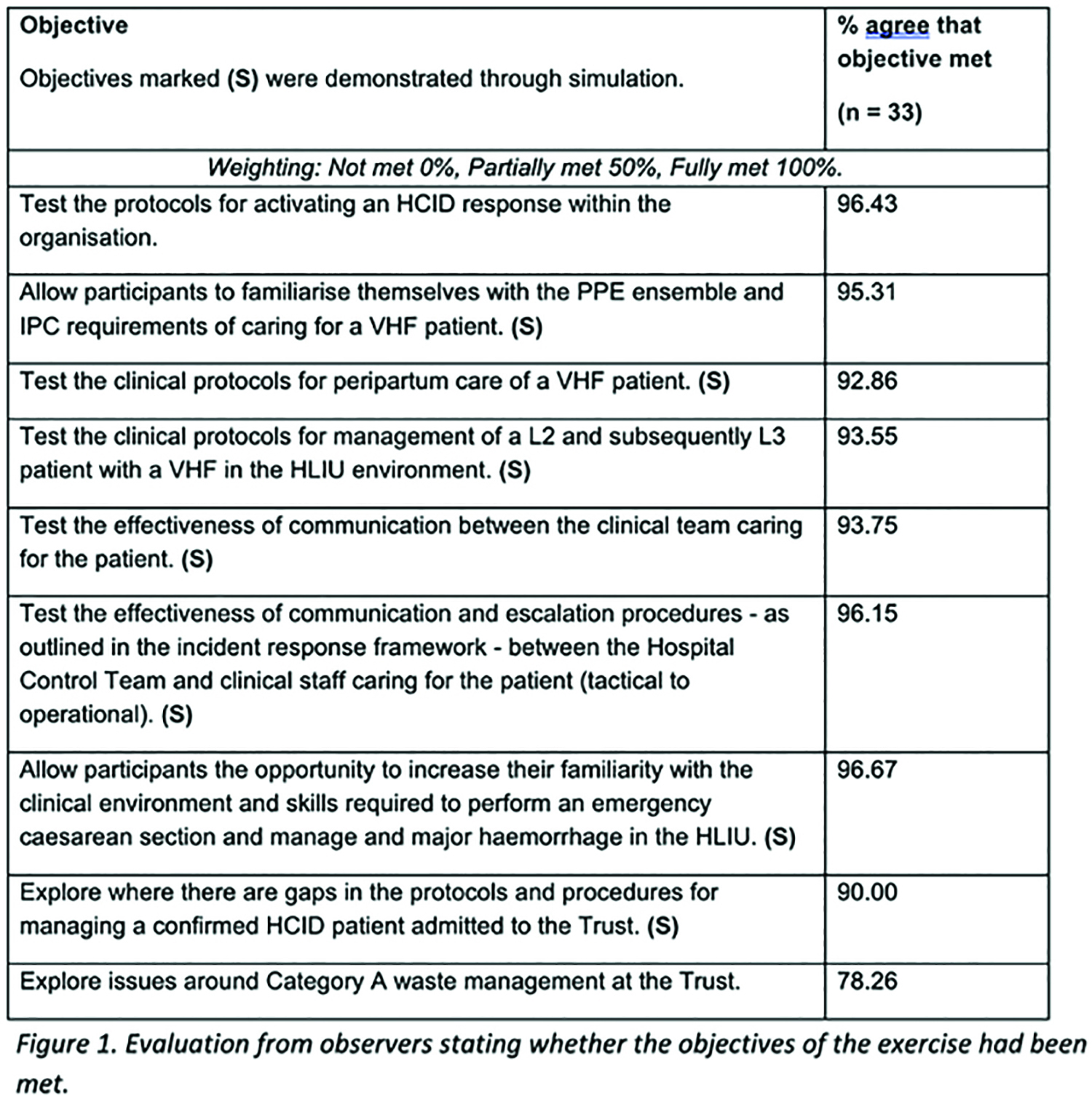
Evaluation from observers stating whether the objectives of the exercise had been met.
Olivia Cole 1, Kirsty Duncan 1, Rose Edwards 1
[1]
University Hospitals Dorset (UHD) relocated maternity services into a newly constructed building. Transformational simulation is an effective method for identifying safety threats and driving healthcare improvements [1]. Research is limited on transformative simulation for maternity relocations. This project aimed to use simulation to identify latent safety threats in a new maternity unit and explore the impact on staff.
Prior to opening, twenty mandatory in situ Multidisciplinary Team (MDT) simulation days were delivered for 682 staff due to work in the new maternity unit. Simulations were co-produced and co-facilitated by simulation, maternity, obstetrics, anaesthetics, transfusion, theatres and porters. Participants received a day’s training, split into three groups of 10–15 people incorporating orientation and rotation through three simulations - Sepsis, Major Obstetric Haemorrhage and Eclampsia – running simultaneously. Simulations required transfers, with locations varied to identify safety risks throughout maternity. MDT debriefs identified safety threats, which were recorded on a risk log and escalated to senior management. Mixed-method data was collected via participant questionnaires after each day to assess impact on staff.
Main safety threats:
Increased time for blood collection, due to increased distance from transfusion.
Removal of dedicated maternity porter.
Staff not trained in blood collection.
Unfamiliarity with department name and location during emergency phone calls.
Lack of adequate signage.
Staff injured during pool evacuations due to new shaped birthing pool.
Improvements:
Increased O-negative blood supply in Maternity emergency fridge.
Automatic printing of blood collection slips to transfusion.
Allocation of general porter for urgent blood collection.
Staff blood collection training.
Location prompt cards adjacent to phones.
Improved flag style wayfinding signage.
Suspension of new birthing pools until alternative evacuation equipment tested.
Impact on staff: Most participants reported increased confidence; 25% reported no change, and 7% reported a decline.
92% felt positive their contributions were valued.
This project identified latent safety threats within a new maternity unit using in situ simulation, leading to real-time improvements. While the overall impact on staff was positive, the decrease in confidence for some - likely due to the identification of safety threats without immediate solutions - suggests the need for further research on managing staff confidence whilst identifying safety threats. Feedback highlighted the value staff placed on orientation simulations, expressing a desire for further sessions. Key lessons for future transformative simulation include the importance of sufficient equipment in proposed locations, formal safety escalation processes and timely feedback to participants.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable
1. Furthmiller A, Sahay R, Zhang B, Dewan M, Zackoff M. Impact of a relocation to a new critical care building on pediatric safety events. J Hosp Med. 2024;19(7):589–595. doi: 10.1002/jhm.13324.
Thank you to Andrew Lawrence, Thomas Randall-Turner, Sam Pask, Lucy Hyde, Julie Flint, Jane Morley-Smith, Kerry Horley, Emma Barton, Fay Tomlinson, Samantha Boullin, Vikki Chandler, Clare Thompson, Bernadette Gowland and all who helped facilitate.