In situ simulation improves participants’ ability to respond to high-stress situations, increases confidence, and enhances interprofessional communication [1]. Simulation has increasingly been recognised by senior medical leadership as a valuable tool in enhancing patient safety. However, our experiential understanding showed that ad hoc simulation sessions across wards were often subject to cancellations and last-minute changes. Additionally the use of generic scenarios did not always reflect the specific clinical challenges faced by individual teams. These issues prompted a reassessment of our approach. We aimed to explore whether embedding a collaborative, ward-specific in situ simulation course would improve engagement, reduce cancellations, and better meet learning needs.
We selected one cardiology ward (6D) to pilot a focused, 6-week in situ simulation programme. A multidisciplinary working group was formed, including members of the simulation team, the ward manager, the practice development nurse (PDN), and a consultant cardiologist. Together, we conducted a targeted learning needs analysis and co-designed six bespoke simulation sessions. A fixed time and location were agreed upon in advance to ensure consistency and support from the ward. Simulations were run every 2 weeks over a 3-month period. Key learning points and safety issues identified during debriefs were compiled in a patient safety report and shared with the wider team. In parallel, we continued to run single, one-off simulation sessions on seven other wards, scheduled at the ward’s most suitable time by corresponding ward managers.
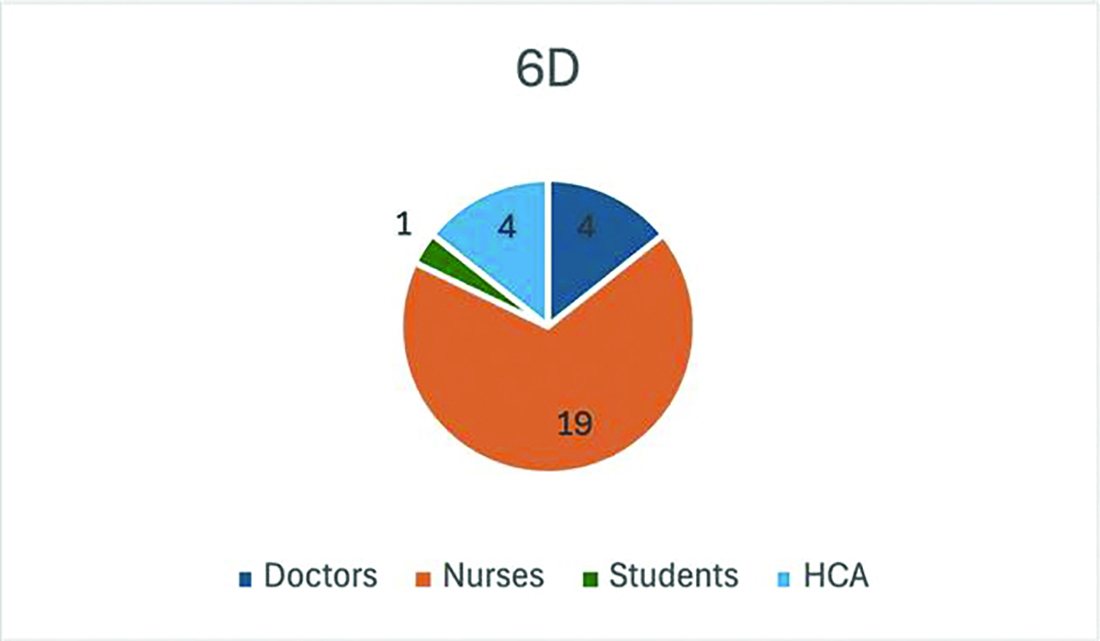
Our dedicated 6D programme achieved a 0% cancellation rate, with strong and consistent attendance across multidisciplinary team (MDT) members, Figure 1. In contrast, the ad hoc sessions across other wards experienced a 57% cancellation rate, with reasons including staffing shortages, lack of available space, or staff being committed to other teaching. Attendance records also showed a greater number of staff and spread of the MDT trained on 6D when compared to the rest of the hospital. Subjective feedback demonstrated that in general all staff recognise the benefit of in situ sim education to the clinical team and were willing to take part finding it both “useful” and “exciting”.
This project demonstrates that co-designing simulation with stakeholders leads to better attendance, fewer cancellations, and more bespoke learning. Structured, ward-integrated simulation not only enhances engagement but also supports a culture of continuous learning and safety. Moving forward, we aim to evaluate whether this approach contributes to sustained behavioural change within ward teams, using the Kirkpatrick evaluation model.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Manggala SK, Tantri AR, Sugiarto A, Sianipar IR, Prasetyono TOH. In situ simulation training for a better interprofessional team performance in transferring critically ill patients with COVID-19: a prospective randomised control trial. Postgraduate Medical Journal [Internet]. 2022 Aug 1;98(1162):617–21. Available from: https://pmj.bmj.com/content/98/1162/617