The Nursing & Midwifery Council (NMC) now mandates nursing students to replace 600 clinical hours with simulated practice learning (SPL) [1]. While Higher Education Institutions (HEIs) are incorporating this shift into curricula, aligning simulation with clinical competencies remains a challenge. Traditional skills training is often hands-on but lacks realism and practical transferability [2].
To bridge the gap between theoretical knowledge and clinical application, we developed a procedural simulation model that embeds clinical skills training within structured simulation scenarios. This model aligns with NMC standards and best practice guidelines, supporting the development of core nursing competencies in realistic settings that are replicable in practice.
This study evaluates the model’s effectiveness in enhancing students’ clinical competence, knowledge, and skills while meeting SPL requirements.
The procedural simulation model was embedded within the curriculum to align with NMC proficiencies for each academic year [1]. Procedural Simulation (Pro Sim) sessions included hands-on practice with equipment and high-fidelity mannequins, scenario-based learning, and structured debriefing with facilitators [2].
Pro Sim was delivered during the first two days of each SPL week, with students grouped by field of practice. To accommodate individual learning styles, students participated in small-group simulations reflecting real-life clinical scenarios [2]. Each three-hour session included a theoretical overview, tutor-led demonstrations, supervised hands-on practice, and debriefing to support reflective learning and knowledge retention.
Informal feedback from students highlighted significant improvements in clinical skills competence and confidence as independent practitioners following Pro Sim sessions. Evaluation data also indicated enhanced communication skills, stronger teamwork abilities, and improved responses to real-life clinical situations, with a noticeable reduction in anxiety about clinical placements.
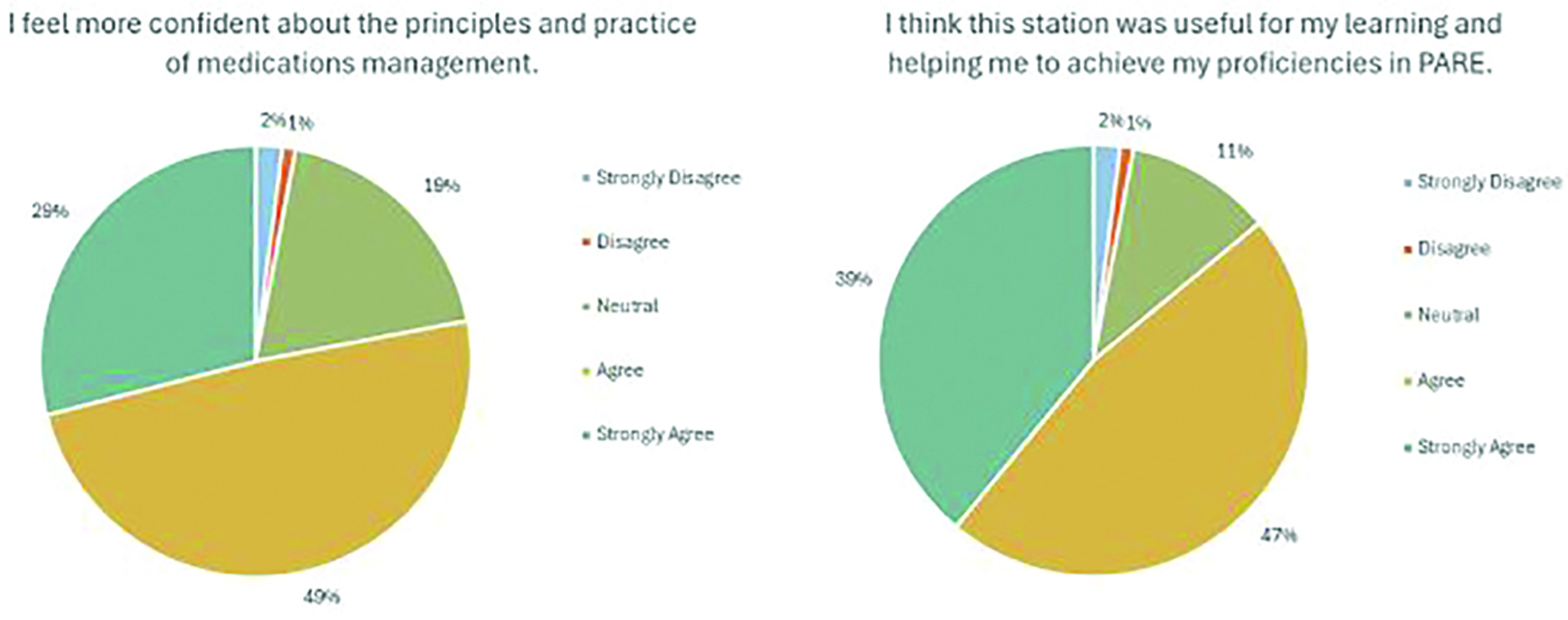
For example, feedback on the Medication Management Pro Sim reflected these overall positive outcomes (Figure 1). Additionally, the Pro Sim model fostered a supportive, culturally competent, and inclusive learning environment.
The Pro Sim model integrates simulation into traditional instructional methods, strengthening existing simulation-based education by allowing students to practice, evaluate, and refine their clinical competencies [1]. A comprehensive plan is in place to collect both qualitative and quantitative data to evaluate the model’s sustained impact on students’ clinical practice.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Holt P. Simulated practice learning in pre-registration nursing programmes [Internet]. 2024 [cited 2025 March 26]. Available from: https://www.nmc.org.uk/globalassets/sitedocuments/simulated-practice-learning/reports/2024/evaluation-of-simulated-practice-learning-in-pre-registration-nursing-programmes.pdf
2. Gent D, Kainth R. Simulation-based procedure training (SBPT) in rarely performed procedures: a blueprint for theory-informed design considerations. Adv Simul. 2022;7:13. doi: 10.1186/s41077-022-00205-4