Simulated patients (SPs) are widely used in healthcare professions education (HPE) to enhance experiential learning, support assessment, and provide realistic, safe environments for developing clinical and communication skills [1,2]. Despite the acknowledged value of SPs in simulation-based education, there is limited consensus on what constitutes effective SP training [3]. The absence of standardised curricula raises concerns about consistency, educational outcomes, and quality assurance. This scoping review sought to explore: What does current literature reveal about the content, methods, and gaps in SP training within HPE?
A systematic scoping review was conducted following the PRISMA-ScR guidelines. Six electronic databases (MEDLINE, PubMed, CINAHL, Scopus, Web of Science, Cochrane Library) and grey literature were searched for English-language studies published up to May 2023. Studies were screened for relevance using pre-defined inclusion/exclusion criteria. Eligible sources reported on SP training in HPE. Data were extracted and analysed thematically to identify trends, gaps, and key training components.
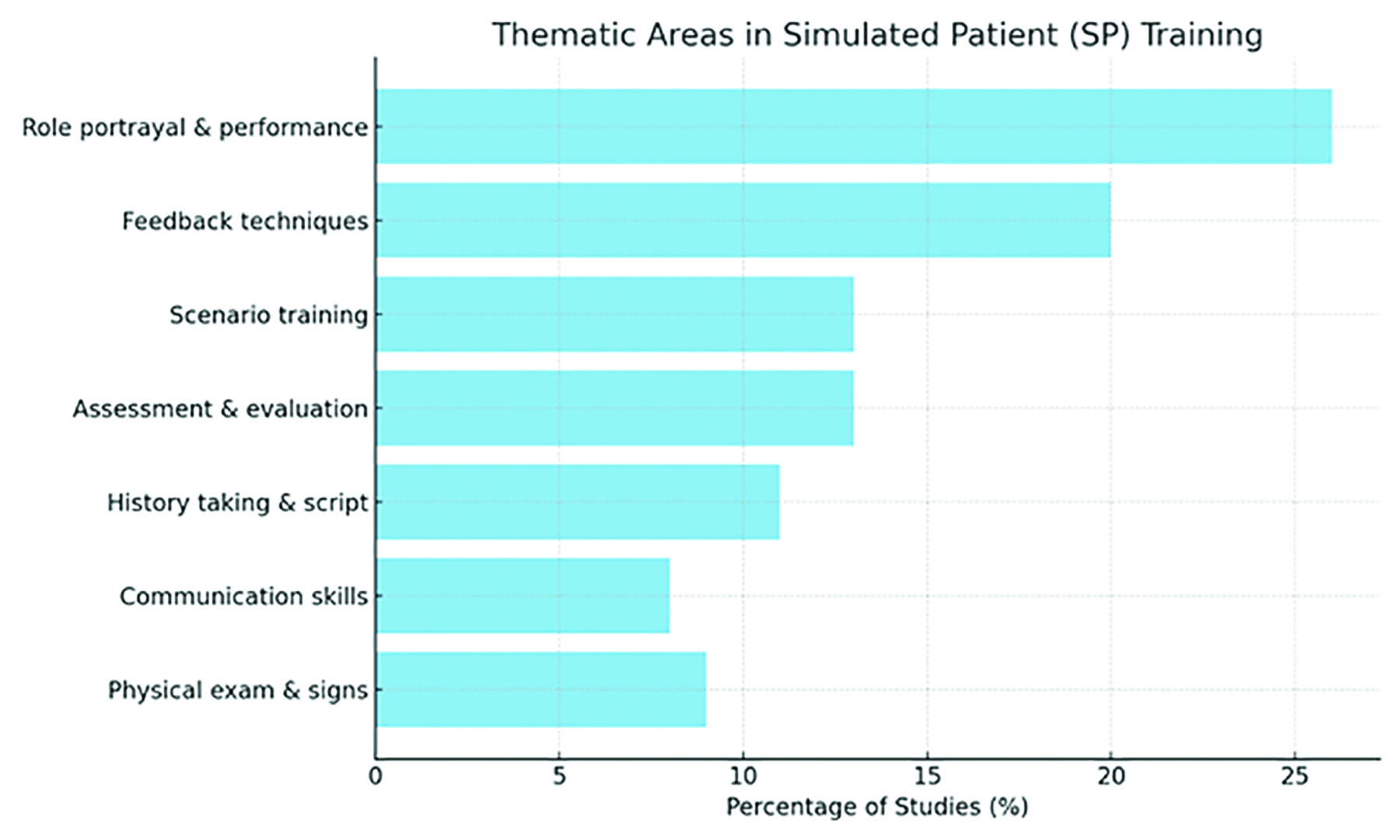
Of the 886 records screened, 25 studies met the inclusion criteria. Thematic analysis identified seven key areas of SP training (Figure 1): role portrayal and performance (26%), feedback techniques (20%), scenario engagement and patient interaction (13%), assessment and evaluation (13%), history taking and scripting (11%), communication skills (8%), and physical examination and signs (9%). Five categories of training methods emerged: structured training sessions, scripted briefs, technology integration, group activities, and observational feedback. Considerable variation in duration, content depth, and assessment methods was noted across studies. No universal framework for SP training was identified.
This review reveals broad variability in how SPs are prepared for simulation roles across institutions. While common training domains exist, there is a lack of standardised curricula, structured assessment tools, and reporting on long-term training outcomes. This variability may limit fidelity, learner experience, and inter-institutional benchmarking. Findings suggest an urgent need for evidence-informed, consensus-driven guidelines to improve SP training quality, consistency, and scalability across HPE.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Cleland JA, Abe K, Rethans JJ. The use of simulated patients in medical education: AMEE Guide No 42. Med Teach. 2009;31(6):477–486.
2. Nestel D, Bearman M. Simulated patient methodology: theory, evidence and practice. Wiley-Blackwell; 2014.
3. Greene G, Gough S. Train-the-simulated-patient programme: a UK evaluation. Clin Teach. 2015;12(6):403–407.