
To investigate whether regular departmental, in situ simulation in trauma resuscitation improves time to computerized tomography (CT) in real patients presenting to the Emergency Department following major trauma.
Ten 30-minute in situ simulation sessions were conducted weekly over 10 weeks, involving Emergency Department staff members who typically form a trauma team. Each session included a 5-minute briefing, a 10-minute scenario and a 15-minute debriefing. Simulations were conducted using a combination of Laerdal MegaCode Kelly manikin with a SimPad Plus control device and iSimulate ALSi Patient Vitals iPad Software. The primary outcome measured was the time from the arrival of a patient into the Emergency Department resuscitation area to CT scan initiation.
A total of 78 major trauma cases were included (40 pre-intervention and 38 post-intervention). Median time to CT decreased from 73 to 41 minutes – a 43.8% reduction (p = 0.033) – while the mean time decreased from 88 to 61 minutes. The proportion of patients receiving CT within 1 hour increased from 43% to 66% (p = 0.040). Although the proportion scanned within 30 minutes rose from 28% to 45%, this difference did not reach statistical significance (p = 0.262). The distribution of CT times shifted significantly towards earlier imaging post-intervention.
Regular in situ simulation training significantly reduces the time to CT for actual major trauma patients in the Emergency Department, enhances team performance and improves real-world clinical outcomes.
Computerized tomography (CT) imaging is critical for the accurate diagnosis and definitive management of traumatic injuries, yet Emergency Department (ED) trauma teams often fail to transfer patients to the CT scanner within the timelines set by National Health Service (NHS) guidelines [1]. Delays in obtaining CT imaging can result in missed or late diagnoses, adversely affecting patient outcomes and increasing the risk of morbidity and mortality [2,3]. Despite the recognized importance of rapid imaging, many trauma centres struggle to consistently meet recommended targets, such as performing CT within 1 hour – and ideally within 30 minutes – of patient arrival [4].
A key challenge is whether targeted interventions, such as team-based training, can close this gap between patient arrival and timely imaging. While simulation-based trauma team training has gained popularity and shows promise for improving team performance and efficiency [5,6], its direct impact on measurable clinical outcomes, specifically, time to CT, remains unclear. Understanding the effect of trauma team training on time to CT is an important next step in identifying strategies to improve trauma care and save lives.
This study investigates whether regular departmental in situ simulation (ISS) in trauma resuscitation can reduce time to CT for major trauma (MT) patients in the ED, thereby providing evidence for the role of simulation-based interventions in enhancing real-world clinical outcomes.
MT is the leading cause of death among the population under the age of 45 worldwide, and the fourth main cause of mortality across all ages [7,8]. Trauma resuscitation is a highly specialized, time-critical multidisciplinary process that begins once the patient enters the doors of the ED. Given the complexity of trauma care and initial patient stabilization, modern EDs have adopted the concept of specially designed trauma teams, whose activation facilitates the rapid pooling of resources for patient reception, assessment and treatment. Trauma team performance depends on multiple factors, which include but are not limited to available resources and the workload of the department, clinical knowledge and prior experience of its members, as well as human factors such as teamwork, leadership and communication skills of the staff involved.
The use of simulation-based trauma team training has been increasingly popular in recent years due to emerging evidence that it can improve trauma team performance, clinical efficiency and overall trauma care for patients in the ED [5,6,9,10]. ISS, defined as a ‘team-based training technique conducted in the actual patient care environment using equipment and resources from that department and involving actual members of the healthcare team’, has become a recognized training technique for Emergency Medicine (EM) clinicians and relevant staff within the ED [11]. More recently, a concept of translational simulation has been developed to describe the use of simulation to directly improve patient care and clinical outcomes via delivering simulation-based interventions [11,12].
CT is a diagnostic technique of choice in MT patients presenting to the ED [13]. Timely delivery of a patient to a CT scanner allows for an early diagnosis of relevant pathology, facilitating prompt decisions regarding necessary treatment and disposition. Shorter times to CT in patients presenting to the ED following MT are associated with decreased length of intensive care unit (ICU) admissions and total hospital length of stay [14]. Current NHS guidelines recommend that CT in MT is performed within 1 hour, and ideally within 30 minutes of the patient’s arrival to the ED [15,16].
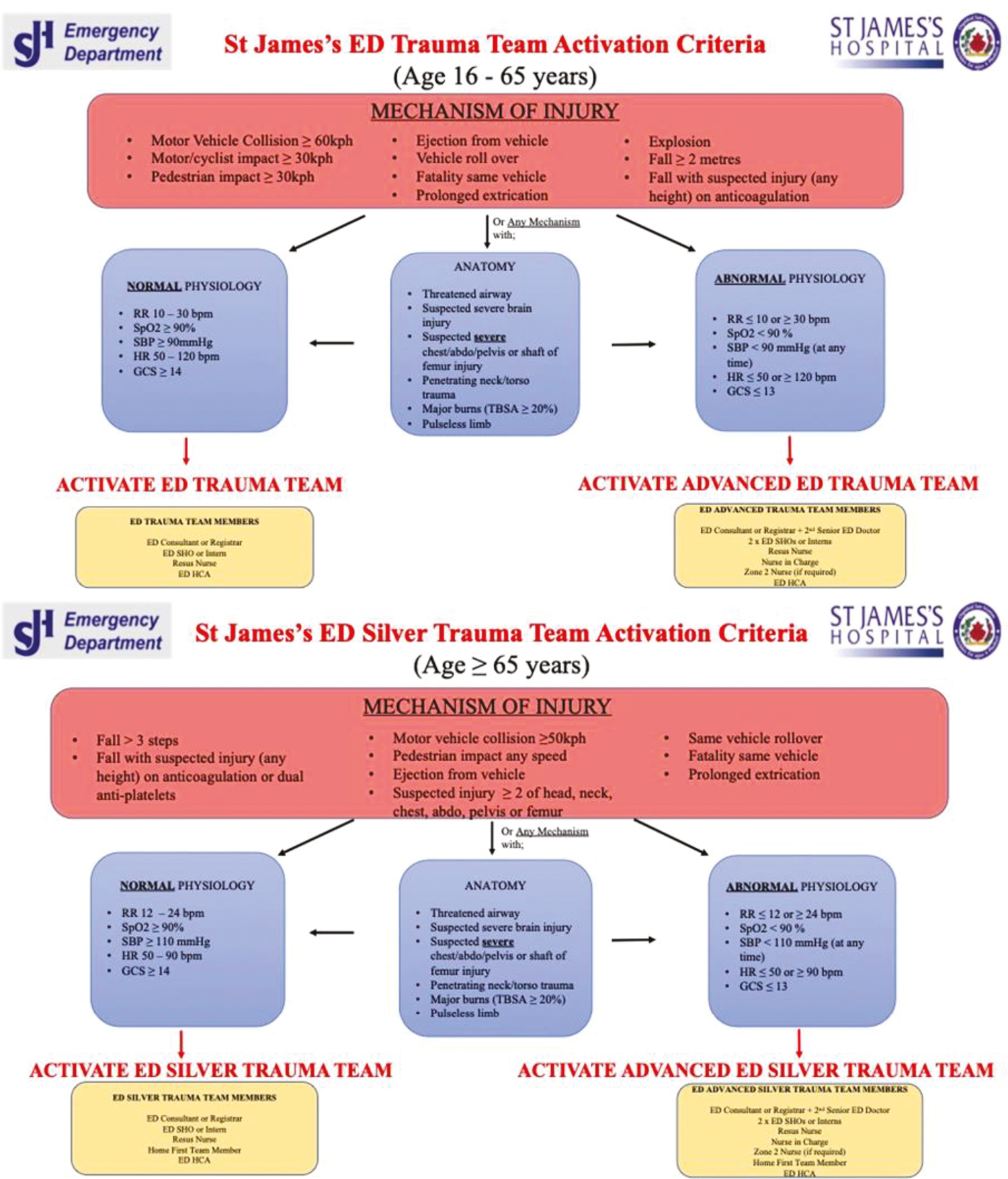
This study was conducted in the ED of St James’s Hospital – Ireland’s largest acute academic teaching hospital based in Dublin’s south inner city. The ED trauma team is assembled whenever a patient who fulfils the St James’s ED Trauma Team Activation Criteria (Appendix 1) arrives at the department. It consists of at least one senior grade and one middle grade or junior EM clinician, an ED resuscitation nurse and a healthcare assistant (HCA). If CT imaging is indicated after the initial resuscitation, the case is discussed with the radiology department, and the patient is taken to the scanner, which is located approximately 5 minutes away from the ED. Time of ED attendance, investigation orders, arrival to CT and scan completion are automatically captured on the hospital’s Electronic Patient Records (EPR) system. Any patient-related documentation is also recorded on EPR.
We conducted two cycles of data analysis performed before and after the planned intervention. The study protocol and intervention design were completed and disseminated to investigators before the first cycle of data collection commenced. Participants were blinded to the objectives of the study until the second cycle of data collection was complete. The need for ethical approval was waived by the hospital’s Research and Innovation office, based on the quality-improvement nature of the study.
The standard clinical rotation year across Irish hospitals runs annually from July to July and includes two major periods of medical staff changeover. The primary rotation of medical staff occurs in mid-July when most middle-grade doctors commence their placements. The second changeover takes place at the beginning of January, when a smaller number of clinicians rotate placements.
We planned the timing and duration of our intervention to accommodate the mid-year change of staff and ensure that both cohorts of physicians received an equal amount of simulation training before we began the post-intervention data collection.
All ISS training sessions were designed, conducted and debriefed by a team of two Specialist Registrars and two Consultants in EM, all of whom had postgraduate training in medical simulation.
We planned and conducted ten 30-minute trauma ISS sessions over the course of 10 weeks. Simulations took place in the ED resuscitation area every Wednesday morning between the last week of November 2023 and the last week of January 2024. Each session consisted of a 5-minute briefing, a 10-minute scenario and a 15-minute debriefing session. To better mimic the real-world conditions, the beginning of every session was marked by an announcement via the departmental Tannoy system that ‘trauma simulation training is taking part in resus’ – a call resembling a standard trauma team activation in the ED.
Participants of each scenario consisted of staff members rostered to work on that day, who would normally form an ED trauma team (Appendix 1) during a real-life event. This typically included at least one EM registrar, Senior House Officer (SHO) and an Intern* who were joined by one or more ED nurses and an HCA. EM consultants did not actively participate in the scenarios but were present to provide a structured debriefing afterwards.
Each simulation session was based on a standard Advanced Trauma Life Support style scenario that was designed to reproduce the most frequent MT presentations to our ED. A total of three scenarios were used interchangeably throughout the intervention phase, which are summarized in Table 1. Expected learning outcomes for each scenario were grouped into medical, nursing and crew resource management (CRM) objectives. CRM refers to the non-technical skills required for effective teamwork and leadership during resuscitation [17]. A sample scenario protocol is shown in Appendix 2.

| Scenario/summary | Medical objectives | Nursing objectives | CRM objectives |
|---|---|---|---|
| All scenarios: The patient is brought to ED by ambulance following the MT event. The mechanism of injury and abnormal physiology warrant an ED Trauma Team activation. |
1) Conduct a structured primary survey, prioritizing tasks and performing life-saving interventions in a timely manner. 2) Arrange an urgent trauma CT and expedite the transfer once the patient is stable, ideally within 30 minutes of arrival. |
1) Perform the primary nursing work-up of a trauma patient, starting with the rapid application of key vital signs monitors. 2) Co-operate with the medical team and HCA to ensure efficient patient preparation and timely transfer to the CT. |
1) Activate, prepare and lead ED Trauma Team during the resuscitation of an unstable MT case. 2) Demonstrate the ability to plan and prioritize tasks, manage workload and utilize available resources. 3) Establish a clear and effective communication strategy within a team. |
| MT with a head injury: A 28-year-old male has crashed his e-scooter. Primary survey is concerning for a significant head injury. Patient warrants a Rapid Sequence Induction with the neuroprotective measures consideration. |
Demonstrate a safe and tailored approach to the intubation of a patient with severe head injury: ○ C-Spine control ○ Tailored choice of induction agents. ○ Early involvement of Anaesthetics and Radiology. ○ Post-intubation care |
Assist an airway doctor with preparing and safely conducting an RSI, including completion of an RSI checklist. | |
| MT – stabbing injury: A 52-year-old male who is assaulted with a knife. Primary survey reveals an intra-abdominal stab injury with free fluid in the abdomen. Patient gradually goes into haemorrhagic shock and will require a blood transfusion with consideration of permissive hypotension. |
Recognize the presence of haemodynamic compromise from an intra-abdominal injury and perform appropriate interventions: ○ FAST Scan ○ Volume resuscitation (blood products) ○ TXA, vasopressors. ○ Early involvement of General Surgery and discussion regarding theatre transfer. |
Set up the Rapid transfuser device and assist in the correct transfusion of blood products to the patient. | |
| MT with pelvic injury: A 31-year-old female has fallen off a horse. Primary survey is concerning for an unstable pelvic fracture. Patient gradually goes into haemorrhagic shock and will require a blood transfusion and consideration of vasopressor use. |
Recognize the presence of haemodynamic compromise from a pelvic injury and administer appropriate interventions: ○ Application of a pelvic binder ○ Volume resuscitation (blood products), TXA. ○ Early involvement of Orthopaedic Surgery. |
Set up the Rapid transfuser device and assist in the correct transfusion of blood products to the patient. |
Simulations were conducted using a combination of Laerdal MegaCode Kelly manikin with a SimPad Plus control device and iSimulate ALSi Patient Vitals iPad Software. Any medical equipment required during the simulation was taken from the resuscitation bay where the training took place.
All scenarios were followed by a two-part structured debriefing, led by an EM consultant and a senior member of the nursing staff. The diamond debriefing tool was chosen as a default method; however, debriefer(s) were able to follow their own structure if they preferred [14]. At the start, all participants were debriefed together as a group by promoting a structured conversation designed to follow three sequential phases. The first phase is the case description, allowing candidates to reflect on their performance as a team and construct a shared mental model among the group. This was followed by a detailed analysis of the scenario and individual actions aimed at validating effective responses, identifying mistakes and exploring opportunities for improvement. The final phase of discussion focused on the potential application of gained experience into real-world situations and breaking down behaviours into specific actions promoting positive practice changes.
At the end of the group discussion, participants were split into two groups, allowing clinicians to scrutinize professional aspects of medical objectives, while nursing and HCAs were debriefed on their performance by senior members of the nursing staff.
The target clinical outcome of this study was the time to CT from the time of arrival of the real-life MT patient to the ED. This information is automatically recorded on the hospital’s EPR system for every patient, along with other relevant data. When the patient is brought to the resuscitation area by ambulance, one of the crew members communicates relevant details to a member of clerical staff, who registers them on the EPR, enabling subsequent patient tracking, placement of clinical orders and electronic documentation. This time point of initial patient ED registration was used as an indicator of the patient’s arrival to the ED throughout the study. When the patient arrives to CT and the scan begins, radiographer changes the order status to ‘exam started’ on the EPR. This event was chosen as an endpoint for measuring the patient’s actual time to CT in this study.
The two cycles of patient data collection took place between 15 July 2023 and 3 December 2023 (pre-intervention), and from the 1 February 2021 to 23 June 2024 (post-intervention), representing a period of just over 20 weeks for each cycle.
Relevant data of all patients presenting to St James’s Hospital ED is systematically recorded and electronically stored using the Microsoft Power Bi software. It contains information regarding patient’s time and date of arrival, presenting complaint, Manchester triage score (MTS), medical record number and various demographic data. This system was used to search for and identify all MT presentations to the ED relevant to this study.
The following criteria were used as search parameters:
•MTS 1 (immediate) or 2 (very urgent); AND
•Presenting complaint containing one of the following terms – ‘Major Trauma’, ‘RTA’ (road traffic accident), ‘assault’, ‘stabbing Injury’, ‘chest injury’, ‘torso injury’.
•In addition, we searched for MTS of 1 with a presenting complaint of ‘head injury’.
An initial search within the defined period generated a list of potential MT attendances. The EPR system was then used to manually examine medical records, before deciding whether it could be classified as a MT case. The following presentations were excluded from the list: patients who did not undergo CT imaging, overnight patients who were deemed well enough to receive imaging the following day, single limb injuries or isolated head injuries with a Glasgow Coma Scale of 15.
In addition, we calculated an Injury Severity Score of potential cases using the information from ED notes, imaging results and discharge summaries. Cases with a score of less than 4 were excluded from the study, as the only injuries sustained were minor. The Injury Severity Score calculation was done by two independent investigators (NV and SM), both experienced EM clinicians. If there was a disagreement among the scores that potentially determined the decision to exclude the case from the study, a third opinion was sought from an EM consultant (DS) with regards to the final score.
Statistical analyses were conducted using R (version 4.2.3 [2023-03-15]). Descriptive statistics were used to summarize patient characteristics and outcomes. Continuous variables, such as age, were reported as means with standard deviations (SD) for normally distributed data and as medians with interquartile ranges (IQR) for non-normally distributed data. Categorical variables, including the proportion of patients meeting time-based targets, were reported as counts (n) and percentages (%).
The primary outcome – median time to CT – was compared between the pre- and post-intervention groups using the non-parametric Mann–Whitney U test. To evaluate differences in the overall distribution of time to CT between groups, a Kolmogorov–Smirnov (K-S) test was also performed.
The combined use of the Mann–Whitney U and K-S tests was chosen to ensure a robust comparison of the time-to-CT distributions. While the Mann–Whitney U test is sensitive to differences in central tendency (median), the K-S test complements this by detecting differences in the overall shape, spread and location of the distributions, which is particularly useful in studies with smaller sample sizes where assumptions of normality may not be met [18]. Key assumptions for both tests, including the independence of observations, were met by the study’s pre-test/post-test design with different patient cohorts. The analysis was performed using statistical software that automatically applies corrections for tied ranks.
Differences in the proportions of patients achieving the 30-minute and 60-minute imaging targets were assessed using the chi-squared (χ²) test for independence.
All statistical tests were two-tailed, and a p-value of <0.05 was considered to indicate statistical significance.
A total of 78 MT cases met the inclusion criteria: 40 in the pre-intervention group and 38 in the post-intervention group. The demographic and clinical characteristics of both cohorts were comparable (Table 2), with a similar distribution of age, sex and Injury Severity Scores.

| Pre-intervention, N = 40 | Post-intervention, N = 38 | |
|---|---|---|
| Age, years | ||
| Mean | 38.15 | 37.84 |
| SD | 14.39 | 16.41 |
| Sex | ||
| Male | 83% (n = 33) | 84% (n = 32) |
| Female | 17% (n = 7) | 16% (n = 6) |
| Injury Severity Score | ||
| Mean | 8.5 | 8.9 |
| Median | 7.0 | 6.0 |
| IQR | 6 | 6 |
Following implementation of the ISS intervention, there was a substantial reduction in the time from ED arrival to initiation of CT imaging. The mean time to CT decreased from 88 minutes (SD 66) pre-intervention to 61 minutes (SD 60) post-intervention. The median time to CT fell from 73 minutes (IQR 58–95) to 41 minutes (IQR 26–87), representing a 43.8% reduction (Figure 1). This difference was statistically significant (Mann–Whitney U test: W = 546, p = 0.033).

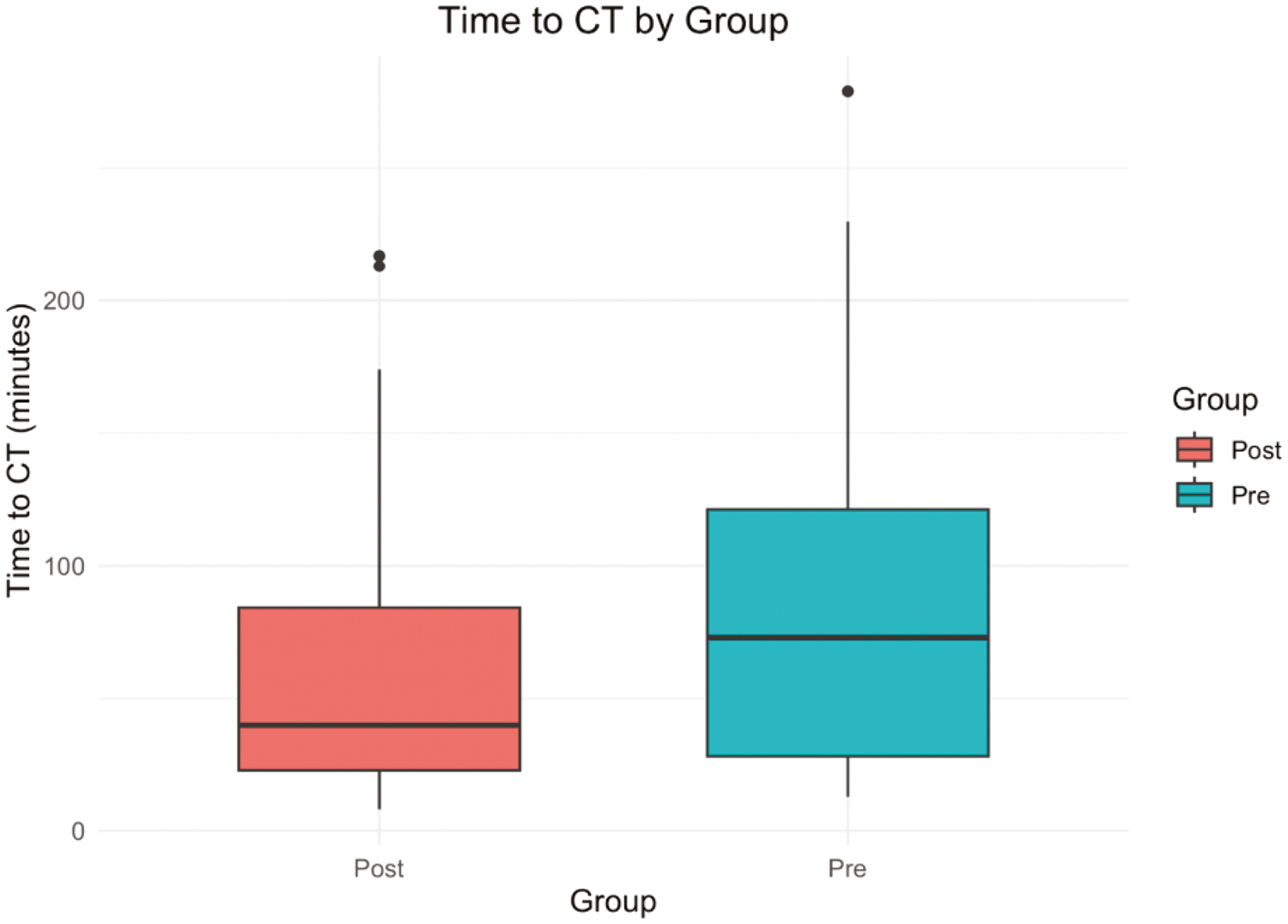
Boxplot showing the distribution of time to CT in pre- and post-intervention groups. The median time to CT was significantly lower in the post-intervention group (Mann–Whitney U test, p = 0.033).
The intervention also led to a significant increase in the proportion of patients meeting recommended time targets. The proportion of patients receiving a CT within 1 hour increased from 43% (n = 17) to 66% (n = 25), a statistically significant improvement (χ² = 4.22, p = 0.040). Furthermore, the percentage of patients receiving a CT within the ideal 30-minute window increased from 28% (n = 11) to 45% (n = 17); however, this difference was not statistically significant (χ²(1) = 1.25, p = 0.264) (Figure 2).

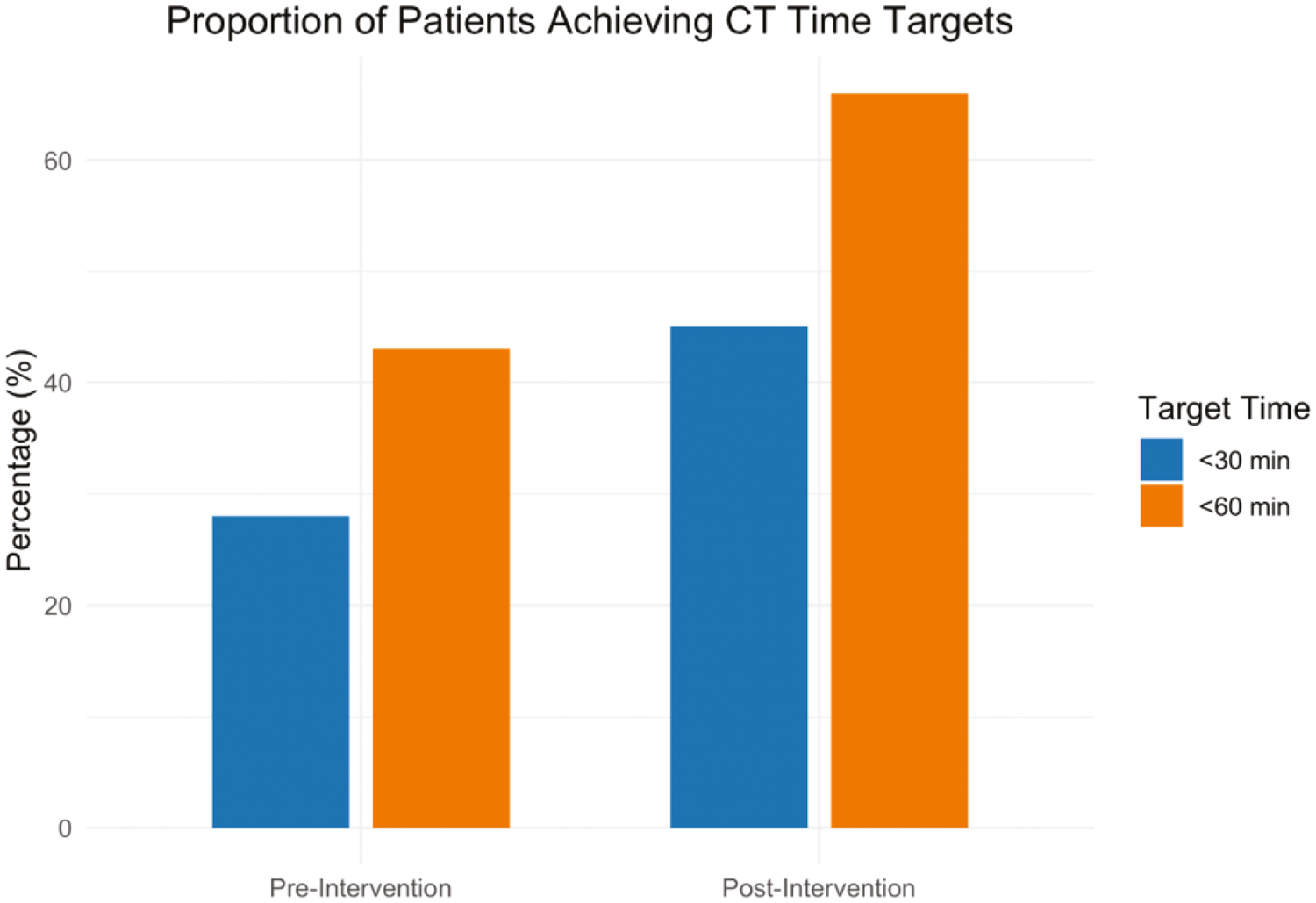
Bar chart showing the proportion of patients achieving CT time targets (<30 and <60 minutes) in pre- and post-intervention groups.
To further evaluate the impact on overall distribution, a K-S test comparing the continuous distributions of time to CT demonstrated a statistically significant difference between groups (D = 0.33, p = 0.019), indicating that the intervention affected not only the median time to CT but also the broader pattern of imaging times (Figure 3).
The cumulative distribution plot (Figure 2) illustrates this shift, showing that a higher proportion of patients in the post-intervention group received CT within shorter time intervals.
These findings suggest that ISS training contributed to both a reduction in median time to CT and a shift towards more consistent and timely imaging performance.

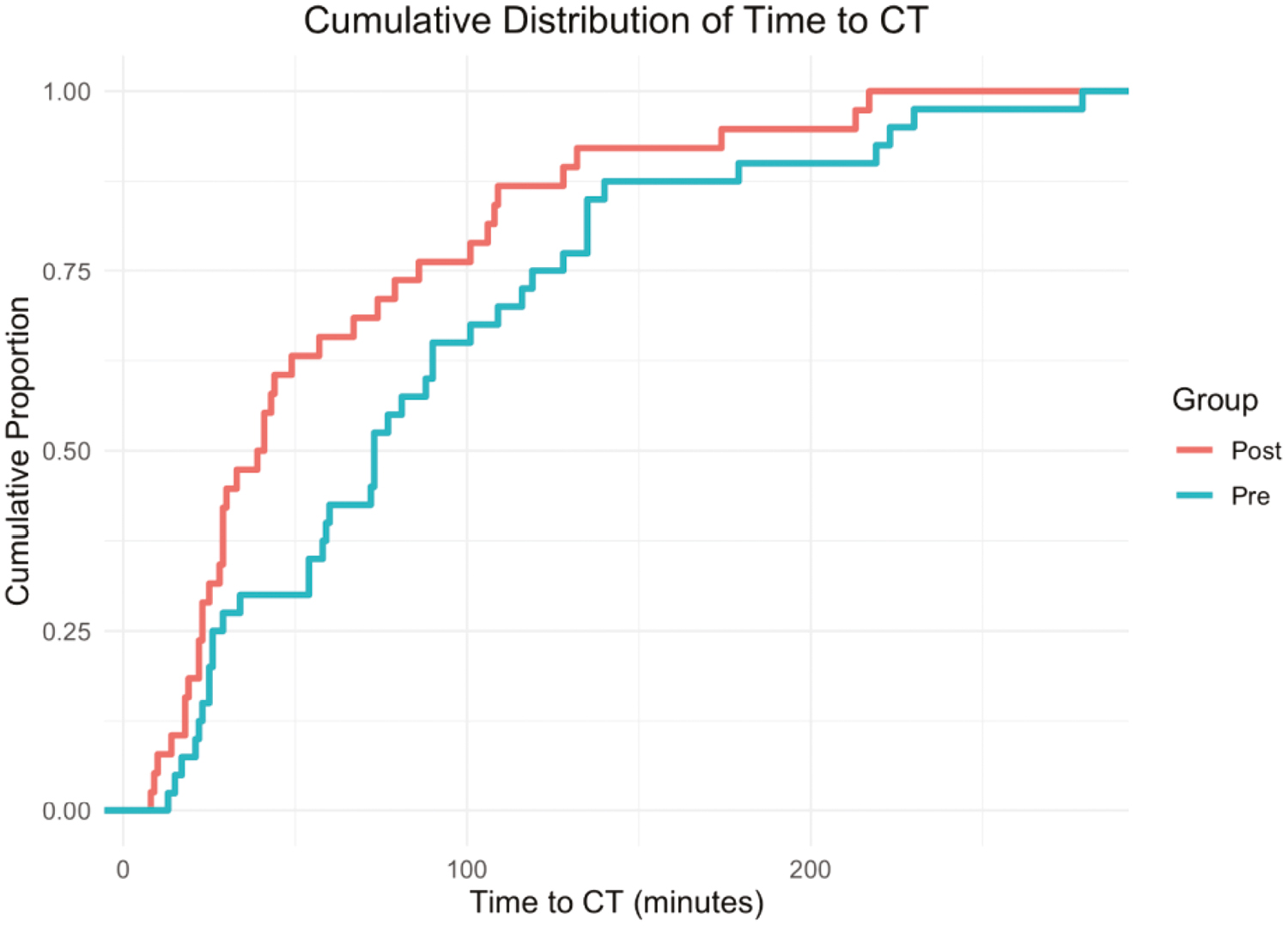
Cumulative distribution plot illustrating the proportion of patients undergoing CT imaging within given time intervals. The distribution shifted significantly towards shorter imaging times in the post-intervention group (Kolmogorov–Smirnov test, p = 0.019)
The key results are summarized in Table 3.

| Pre-intervention | Post-intervention | p-Value | |
|---|---|---|---|
| Time to CT, minutes | |||
| Median (IQR) | 73 (58–95) | 41 (26–87) | <0.01 |
| Mean (SD) | 88 (66) | 61 (60) | |
| CT within 1 hour | 43% (n = 17) | 66% (n = 25) | 0.031 |
| CT within 30 minutes | 28% (n = 11) | 45% (n = 17) | 0.177 |
The objective of this study was to determine whether regular departmental ISS in trauma resuscitation could improve time to CT in real patients presenting to our ED with MT. The results demonstrated a significant improvement, with a 43.8% reduction in the median time to CT following the intervention. In parallel, the mean time to CT decreased from 88 to 61 minutes. While the mean provides a general overview of performance, it is sensitive to outliers and, in this case, likely overestimates the typical patient experience due to the skewed nature of the data. However, the mean has been reported alongside the median to ensure transparency and comparability with other quality improvement studies and institutional metrics.
The proportion of patients receiving CT within one hour increased from 43% to 66%, a statistically significant improvement that aligns with NHS performance standards. Although the percentage of patients receiving CT within 30 minutes also increased – from 28% to 45% – this difference did not reach statistical significance, likely reflecting limited statistical power due to the sample size. Nonetheless, the trend suggests that ISS contributed to earlier imaging and improved workflow efficiency.
Beyond these improvements in central tendency and target achievement, the K-S test demonstrated a statistically significant shift in the overall distribution of CT times between groups. This finding indicates that the intervention not only reduced the median time but also influenced the broader pattern of imaging times, with a higher proportion of patients in the post-intervention group undergoing CT within shorter intervals. The cumulative distribution plot further illustrates this effect, suggesting that ISS helped create a more consistent and efficient trauma care pathway by reducing prolonged delays and improving the reliability of timely CT access.
The substantial reduction in time to CT observed in this study aligns with the primary goal of utilizing ISS to enhance clinical efficiency in trauma resuscitation. This improvement is clinically significant, considering that timely CT imaging is crucial for the early diagnosis of traumatic injuries and the prompt initiation of appropriate treatment. The findings suggest that incorporating regular ISS sessions into the ED’s routine training can lead to measurable improvements in actual time-sensitive clinical outcomes.
Previous studies have highlighted the benefits of simulation-based training in improving trauma team performance and patient outcomes. For instance, Steinemann et al. [4] reported that in situ multidisciplinary simulation-based teamwork training enhances early trauma care, which is consistent with our findings. Similarly, Knobel et al. [3] demonstrated that regular in situ team-based training in trauma resuscitation enhances confidence and clinical efficiency among team members. Our study adds to this body of evidence by showing that such training can specifically reduce time to CT in a real-world ED setting.
Several factors likely contributed to the observed improvement in time to CT:
1.Enhanced team coordination and communication: Regular simulation training likely improved the coordination and communication skills of the trauma team, enabling them to perform more efficiently during actual resuscitations.
2.Familiarity with protocols and equipment: Repeated practice in a realistic environment using actual department resources and equipment may have increased the team’s familiarity and comfort with the processes and protocols required for rapid patient assessment and transfer to CT.
3.Crisis Resource Management (CRM) Skills: The focus on CRM objectives during simulations, such as planning, prioritization and resource utilization, likely contributed to better team performance during real trauma cases.
Implementing regular ISS in our ED provided valuable insights beyond measurable outcomes. One of the most significant lessons was the importance of tailoring scenarios to reflect the actual workflow, equipment and interprofessional dynamics of our trauma team. Conducting simulations in the real clinical environment fostered greater engagement and realism, but also posed logistical challenges, such as coordinating staff schedules and minimizing disruptions to patient care. Ensuring buy-in from all team members, particularly during busy clinical periods, required clear communication about the objectives and value of the training.
A notable challenge was the initial design of our simulation program by physicians only, which may have limited the focus on nursing and allied health perspectives. In future iterations, involving nursing educators and other team members in scenario development and debriefing would likely enhance relevance and inclusivity. Additionally, while our sessions focused on training and improving team performance, we recognize that simulation can also be a powerful tool for system exploration – identifying latent safety threats, workflow bottlenecks or equipment needs that impact time to CT [19]. Incorporating an explicit ‘exploration’ component, such as structured feedback on environmental or process barriers, could further optimize trauma care pathways.
While the results are promising, several limitations should be acknowledged. This study was conducted at a single academic hospital, which may limit the generalizability of the findings to other settings with different resources, patient populations or organizational structures.
Our post-intervention data collection period was relatively short. Longer follow-up periods would be needed to assess the sustainability of the observed improvements. In addition, a sample size of 78 patients, though sufficient to demonstrate significant differences, is relatively small. While the improvement in times to CT was demonstrated, continuous ongoing training is likely required to ensure sustained quality of care.
Our study’s design team consisted solely of physicians, which may have influenced scenario focus and limited the integration of nursing or allied health perspectives. Future programs should incorporate nursing and interprofessional educators to ensure a more holistic approach. Furthermore, our ISS sessions were primarily designed as training interventions rather than as opportunities for environmental or process exploration. While this approach improved team performance, it may have missed opportunities to identify and address system-level barriers to timely CT, such as equipment placement or workflow inefficiencies.
Future research could address these limitations by conducting multicentre studies and extending the follow-up period would help determine whether the improvements in time to CT are maintained over time and translate into better long-term patient outcomes.
In addition, investigating the effect of ISS on other important clinical outcomes, such as morbidity, mortality and length of hospital stay, would provide a more complete picture of its benefits. Finally, evaluating the cost-effectiveness of ISS programs would help justify their implementation in resource-limited settings in the future.
This study demonstrates that regular ISS training significantly improves the time to CT for MT patients in the ED. By enhancing team coordination, communication and familiarity with protocols, ISS serves as an effective tool for improving actual clinical outcomes in trauma care. Future research should aim to validate these findings in larger, multicentre studies with longer follow-up periods and explore additional clinical and economic benefits of ISS.
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
The learning outcomes for the scenario are divided into medical objectives and CRM. Medical objectives are based on evidence-based clinical standards focused on a patient or a particular task. They are derived from the pre-requisite knowledge sources described earlier. CRM refers to the nontechnical skills required for effective teamwork and leadership during resuscitation. These include communication, planning and prioritization, situational awareness, workload management, and utilization of available resources [17]. Table A1 summarizes the learning outcomes.

| Learning outcomes | |
|---|---|
| Medical objectives | 1) Conduct a structured primary survey, prioritizing and performing life-saving interventions in a timely manner. 2) Recognize the presence of haemodynamic compromise from a pelvic injury and administer appropriate interventions: ❏ Application of a pelvic binder ❏ Volume resuscitation (blood products), Tranexaminc Acid ❏ Early involvement of General Surgery and Orthopaedics 3) Arrange an urgent trauma CT and expedite the transfer once the patient is stable, ideally within 30 minutes of arrival. |
| CRM objectives | 1) Activate, prepare and lead ED Trauma Team during the resuscitation of an unstable trauma patient. 2) Demonstrate the ability to plan and prioritize tasks, manage workload and utilize available resources. 3) Establish a clear and effective communication strategy with your team and relevant specialities. |
| Nursing objectives | 1) Perform the primary nursing work-up of a trauma patient with a focus on rapid application of key monitors and equipment. 2) Set up the Rapid transfuser device and assist in the correct transfusion of blood products to the patient. 3) Co-operate with the medical team and HCA to ensure efficient patient stabilization and timely transfer to the CT. |
A 31-year-old female patient is brought to the ED by ambulance after falling off a horse. She shows signs of haemodynamic compromise pre-hospital and warrants an ED Trauma Team activation. The primary survey is concerning for an unstable pelvic fracture. As a result of an open-book pelvic fracture, the patient gradually goes into haemorrhagic shock and will require blood transfusion and consideration of vasopressor use to improve.
The scenario will start with the ED team receiving an ambulance pre-alert about the patient, giving them about two minutes to prepare for the patient’s reception. All participants will be present in the resuscitation room from the beginning. The team leader will be expected to allocate roles, conduct a primary survey, and administer life-saving treatments promptly. Participants will need to effectively communicate within their team and when involving relevant specialities. Scenario ends when the patient is stabilized and ready for a CT.

| Simulation timeline | ||
|---|---|---|
| Preparation: 5 minutes | Scenario: 15 minutes | Debriefing: 10 minutes |

| I. Clinical vignette – to be read out to participants at the beginning of the case. | |||||
|---|---|---|---|---|---|
| You are the EM registrar on night duty in St James’s Hospital. ED CNM informs you that she received an EMS pre-alert about a 31-year-old female patient who fell from a horse. Ambulance crew requesting ‘Resus on arrival’. The Pre-Alert information is as follows: | |||||
| Source: | DFB | Category: | Trauma | Condition | (vitals provided) |
| Age: | 31 | Resp: | 24 bpm | ||
| Sex: | Female | Sats: | 95% on room air | ||
| History: | Fell off a horse during a jumping competition. Landed on hard ground, helmet present. Had two syncopal episodes with the DFB. | HR: | 124 | ||
| BP: | 82/41 mmHg | ||||
| Temp: | 36.5°C | ||||
| Injuries: | Limb shortening, suspected pelvic fracture. | GCS: | 14/15 | ||
| ETA: | 3 minutes from now (call received 1 min ago) | BSL: | 5.5 mmol/L | ||

| II. Baseline patient condition and physical exam at the beginning of the scenario. | |||||
|---|---|---|---|---|---|
| General state: | Covered in dirt, moaning in pain. Appears unwell. | ||||
| Vital signs: | HR: 124 | BP: 80/40 | RR: 24 | SpO2: 95% | Temp: 36.5 |
| Airway | Patent, no abnormal sounds, or signs of compromise | NORMAL | |||
| Breathing | Good air-entry bilaterally; midline trachea; symmetrical expansion; resonant. No chest bruising or deformity. | NORMAL | |||
| Circulation | In shock; cold, clammy peripheries. abdomen soft, tender in the lower regions. No external bleeding. S-tachy; S1-S2. | ABNORMAL | |||
| Disability | GCS=14 [E4V4M6]; PEARLA; No lateralizing neuro deficit. | ABNORMAL | |||
| Exposure | Abrasions over limbs. Bruising around the perineum. No long bone deformity, but LL length appears asymmetrical. | ABNORMAL | |||

| III. Scenario stages, patient states, actions, modifiers and triggers. | ||
|---|---|---|
| Stage/patient status | Learner actions | Modifiers and triggers |
| Stage 1. Pre-Alert | ❏ Activates ED Trauma Team ❏ Allocates roles ❏ Anticipates potential problems and verbalizes action plan |
❖ All actions are complete or 2 minutes pass ➣ Stage 2. |
| Stage 2. Arrival HR: 124 BP: 80/40 RR: 24 SpO2: 95% RA Temp: 34.5 GCS = 14 [E4V4M6] PEARLA Appears unwell, moaning in pain. |
❏ Primary survey ❏ Monitors attached ❏ IV access 2x ± IVF bolus ❏ Bloods, VBG, X-match, B-hCG ❏ CXR + Pelvic XR ❏ FAST scan ❏ Pelvic binder ± C-Spine collar ❏ TXA ❏ Blood products requested ❏ Analgesia ❏ Trauma CT ordered and discussed ❏ Gen Surg/ Ortho/ ICU called |
❖ VBG taken ➣ Results given ❖ Imaging requested ➣ Results shown ❖ IVF bolus ➣ BP: 86/42 |
| ❖ 5 minutes’ pass ➣ Shock |
||
| Stage 3. Shock HR: 130 BP: 75/35 RR: 28 SpO2: 94% RA Temp: 36.5 GCS = 12 [E3V4M5] |
❏ Recognizes and verbalizes haemorrhagic shock state ❏ Administers blood products ❏ Vasopressors ❏ Rapid transfuser ❏ Considers MTP ❏ Gen Surg/ Ortho/ ICU called ❏ Reassessment and summary |
❖ 1 unit of RCC ➣ ↑ BP by 10 mmHg ❖ Vasopressor use ➣ ↑ BP by 15 mmHg ❖ Transfusion started ➣ Response |
| Stage 4. Response HR: 105 BP: 102/64 RR: 20 SpO2: 95% RA Temp: 36.5 GCS = 14 [E4V4M6] |
❏ Verbalizes CT as the next priority in patient management ❏ Calls HCA ❏ Prepares for transfer: ❏ Oxygen ❏ Emergency drugs ❏ Sedation ❏ Airway back-up ❏ Reassessment and summary |
★ Verbalizes CT as a priority ➣ Call from CT as ‘ready’ ➣ END OF SCENARIO |
| End of scenario! | ||

| Type of feedback: | Group debrief | ❖ 10-minute structured group discussion immediately after the end of the scenario. ❖ Led by a simulation lead |
| Debriefer role: | Facilitator/ guide | ❖ Enable a structured conversation. ❖ Lead the group to useful debriefing outcomes by promoting effective learning. |
| Debriefing model: | Diamond debrief [20] | ❖ Three-phase conversation structure: ❖ Description, analysis, application. |

| Phase and underlying principles | Sample questions |
|---|---|
| 1) Description ❖ Reinforce a safe learning environment. ❖ Construct a shared mental model. |
❖ What happened? And then? ❖ Do you think you managed this case of MT well as the ED Trauma Team? ❖ What issues/diagnoses did the patient have? |
| 2) Analysis ❖ Explore what happened in detail. ❖ Validate effective responses. ❖ Keep the discussion positive. |
❖ How did you handle the primary survey? ❖ What are the management priorities in a trauma patient with haemorrhagic shock? ❖ What guides your decision to do CT versus OT? ❖ Within what frame does CT need to be performed? |
| 3) Application ❖ Move to the more general world of practice. ❖ Break behaviours down into specific actions. |
❖ What will you do differently when you see a major trauma patient in real life? ❖ How can you reduce your cognitive load when leading complex cases? ❖ How can the time to CT be expedited? |

| Key concepts and take-home points | Further reading |
|---|---|
| Importance of a structured assessment and management in major trauma. | https://bulletin.facs.org/2018/06/atls-10th-edition-offers-new-insights-into-managing-trauma-patients/ |
| Recognition and management of haemorrhagic shock in patients with pelvic fractures. | https://www.rcemlearning.co.uk/reference/pelvic-injuriesv2/#1669399706852-6839d2cc-eb61 |
| Importance of urgent imaging in MT. | https://www.england.nhs.uk/wp-content/uploads/2014/04/d15-major-trauma-0414.pdf |