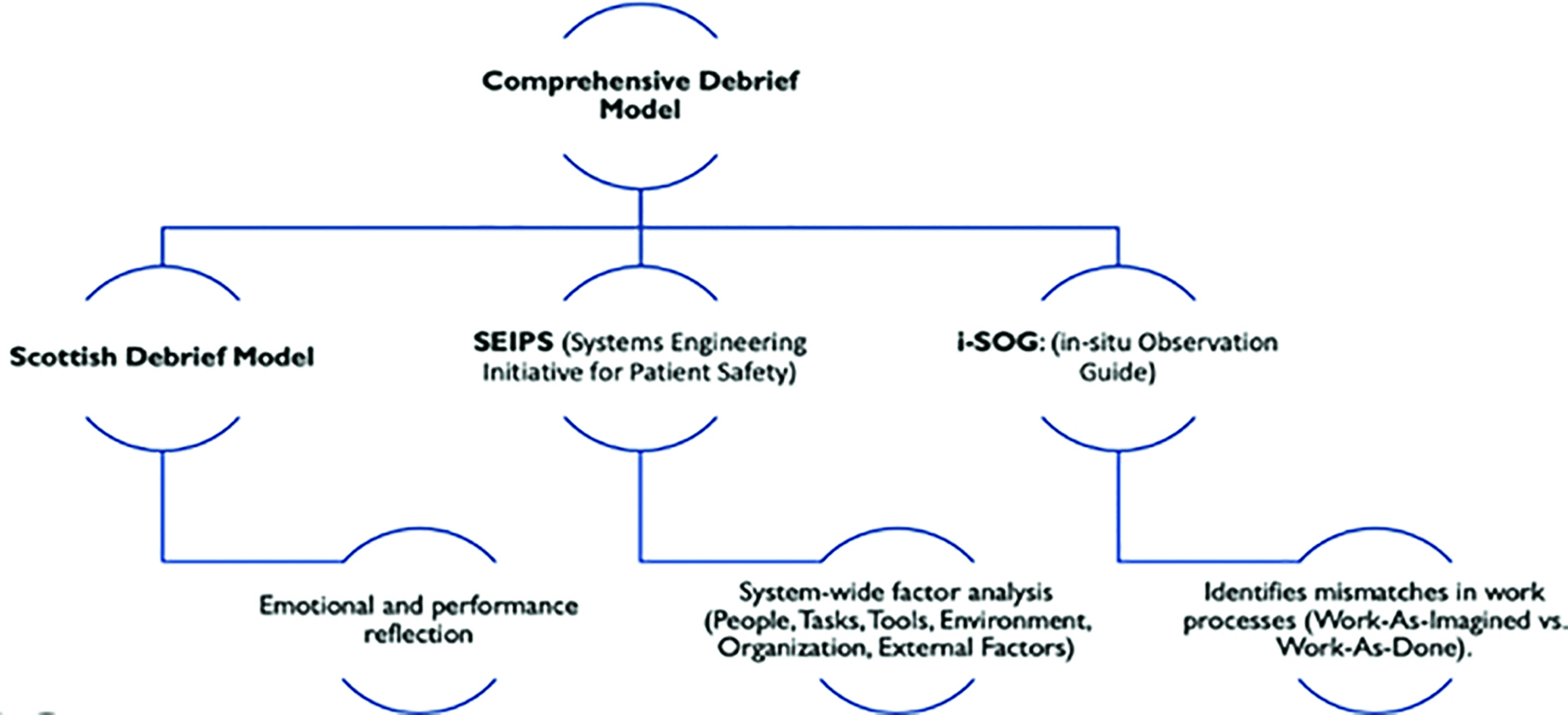
Managing anticoagulation in emergencies requires swift decisions, collaboration, and precision. Despite existing guidelines, real-world practice often suffers from delays and inconsistencies. This Quality Improvement Project (QIP) at the Royal Victoria Hospital (RVH) used in situ simulation combined with a novel debriefing model integrating, Figure 1:
•Scottish Debrief Model – for emotional processing and team reflection.
•SEIPS framework – to analyse system-level safety factors.
•i-SOG – to highlight gaps between intended and actual workflows.
This structured debriefing enabled identification of performance and system issues while aligning with the four Meta-Debriefing pillars:
1. Theory-based – rooted in established models.
2. Psychologically safe – fostering open discussion.
3. Context-dependent – focusing on ED-specific anticoagulation challenges.
4. Formative – driving practical improvements and learning.
Three in-situ simulation sessions simulated major haemorrhages in anticoagulated patients. ED doctors, nurses, and pharmacists participated; senior clinicians and QI leads observed. Each session was followed by structured debriefs assessing: Individual/team performance (Scottish Model), System inefficiencies (SEIPS), and Workflow discrepancies (i-SOG).
First simulation exposed major issues:
•Delays due to poor access to reversal agents
•Uncertainty around guideline interpretation
•Environmental constraints like poor layout
Interventions included:
•Improved drug storage and accessibility
•Simplified, more visible guidelines
•Environment redesign for better workflow
•Targeted team training
Second simulation (post-intervention):
•Better protocol adherence
•Quicker, more confident drug handling
•Stronger communication and teamwork
Third simulation (with new pathway):
•Marked improvement in protocol compliance
•Reduced drug preparation delays
•Closure of key workflow gaps
This debrief model provided a comprehensive view of individual and system-level issues. It led to the creation of a practical, ED-specific anticoagulation reversal pathway, addressing both human and systemic challenges. The method upheld the four Meta-Debriefing principles, ensuring simulations were safe, relevant, and improvement-oriented.
By validating the interventions through measurable improvements, this approach proved effective. It offers a scalable model for embedding into routine emergency training, enhancing clinician readiness, workflow efficiency, and patient safety in high-risk scenarios.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Holden RJ, Carayon P, Gurses AP, Hoonakker P, Hundt AS, Ozok AA, Rivera-Rodriguez AJ. SEIPS 2.0: a human factors framework for studying and improving the work of healthcare professionals and patients. Ergonomics. 2013 Nov 1;56(11):1669–86.
2. Patterson MD, Geis GL, Falcone RA, LeMaster T, Wears RL. In situ simulation: detection of safety threats and teamwork training in a high risk emergency department. BMJ quality & safety. 2013 Jun 1;22(6):468–77.
3. Kumar P, Collins K, Oliver N, Duys R, Park-Ross JF, Paton C, Laws-Chapman C, Eppich W, McGowan N. Exploring the Meta-debrief: Developing a Toolbox for Debriefing the Debrief. Simulation in Healthcare. 2024 Oct 17:10–97.
We would like to extend our sincere gratitude to the Emergency Department team at the Royal Victoria Hospital for their invaluable support and collaboration throughout this Quality Improvement Project. Their commitment to excellence, openness to innovation, and active participation in simulation-based learning were instrumental in driving meaningful change. This work would not have been possible without their enthusiasm, expertise, and dedication to improving patient safety and clinical practice.