Ambulance services are seeing an increase in PEoLC patients electing to remain at home, with a focus on supportive care [1]. A challenge exists in how to suitably equip and empower ambulance services to adapt their culture, shifting from survival focussed care to supportive care for this patient group. Addressing this need through the implementation and development of simulation workshops, which are proven to be effective [2], aims to explore the impact on clinicians and consider the potential for further programme development.
Simulation workshops with professional actors were facilitated by the service’s PEoLC team in partnership with Advanced Paramedic Practitioners in Urgent Care (APP-UC). The programme was developed over a two-year period; feedback and reflections on year 1 informed the design of year 2. Scenarios each year were designed based on current themes in local clinical practice including recent incidents. A total of 66 clinicians participated (42 in 2023 and 24 in 2024). They were asked to complete a contemporaneous and retrospective survey. Questions explored confidence and learner perceptions around how the course design and delivery influenced their educational experience.
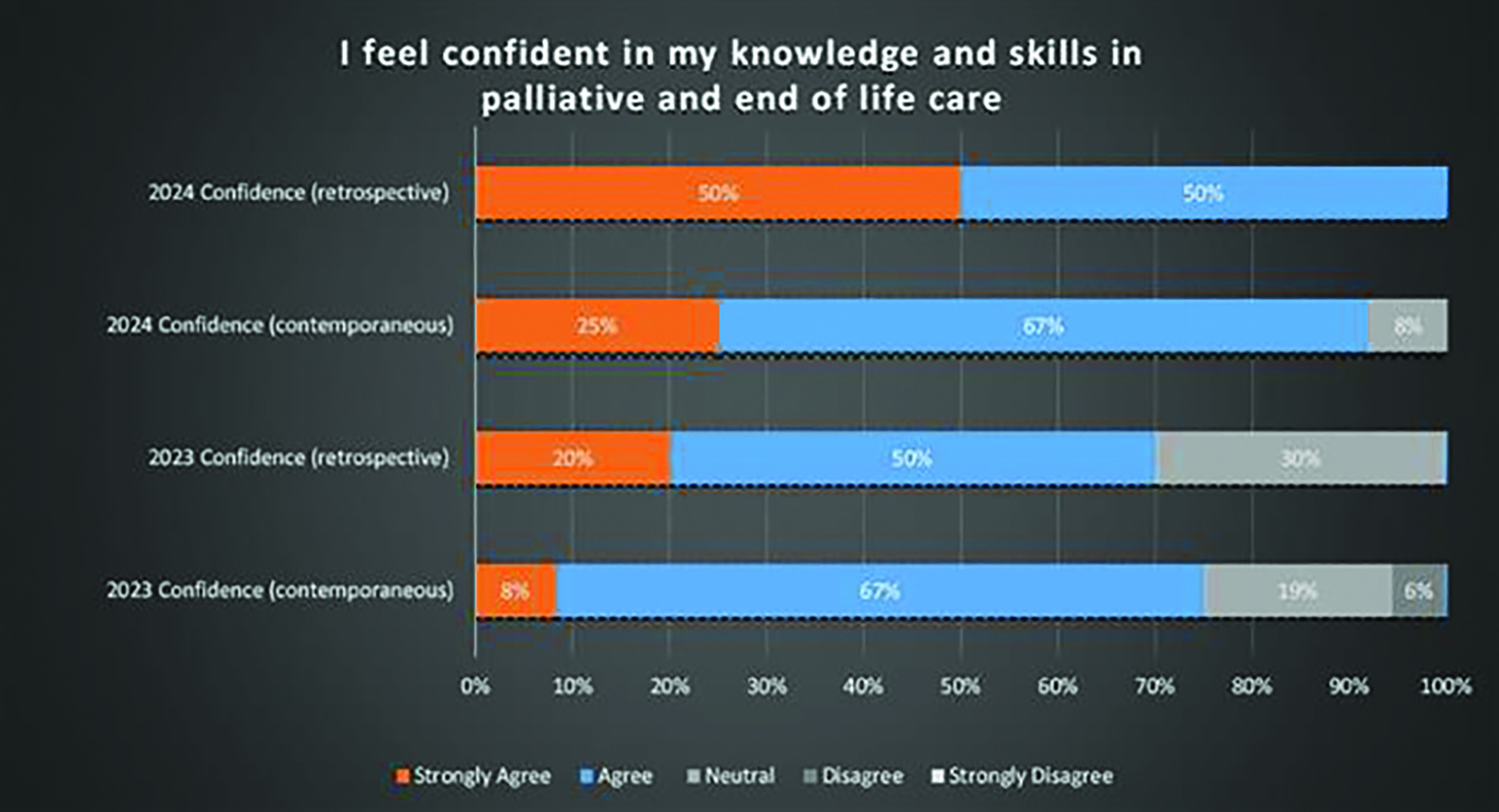
Of 66 participants across two cohorts, contemporaneous survey results were gathered from 91%. Of the 42 participants in 2023 only 24% responded to the retrospective survey, of 24 participants in 2024 only 17% responded. This low response level is a limitation, alongside the subjective nature of recollections of educational experiences. Results demonstrate high levels of confidence sustained into practice across both participant groups (Figure 1).
The majority of participants (89% in 2023; 96% in 2024) felt that the simulation design, particularly the use of actors, contributed to the realism of scenarios.
Smaller groups were identified as an element influencing comfort when participating in simulation, with a 20% increase in participant comfort where this was implemented in 2024.
A high level of comfort participating in debriefs (86% in 2023; 96% in 2024) was reflected through the main theme of fostering a safe learning environment through a non-judgemental, non-assessment focussed approach. This seeks to transform education delivery beyond the current testing and assessment based approach [3].
Emergent themes from surveys and the delivery teams own reflections highlight the effectiveness of simulation in PEoLC education evidencing high levels of confidence, allowing clinicians to practice important and underutilised skills in a psychologically safe environment. Further development of the design and delivery, driven by feedback will allow for improved educational experiences.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Johansson T, Pask S, Goodrich J, Budd L, Okamoto I, Kumar R, et al. (Time to care: Findings from a nationally representative survey of experiences at the end of life in England and Wales. Research report. London (UK): Marie Curie. (September 2024). Available from: www.mariecurie.org.uk/policy/better-end-life-report
2. Elendu C, Amaechi DC, Okatta AU, Amaechi EC, Elendu TC, Ezeh CP, et al. The Impact of simulation-based Training in Medical education: a Review. Medicine [Internet]. 2024;103(27):1–14. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC11224887/
3. Abelsson A, Rystedt I, Suserud BO, Lindwall L. Learning by simulation in prehospital emergency care - an integrative literature review. Scandinavian Journal of Caring Sciences [Internet]. 2015 Aug 29;30(2):234–40. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1111/scs.12252