
This study investigated how occupational physical activity (OPA) affects cognition and self-reported physical exertion in paramedicine students in simulation.
Eleven paramedic final-year paramedicine students or recent graduates: seven regional male and four regional female students completed two randomized crossover simulations: one preceded by OPA, another by rest (REST). Neurocognitive tests: Paced Auditory Serial Addition Test (PASAT) and Repeatable Episodic Memory Test (REMT) were administered pre-simulation, immediately post-simulation, and 60-minute post-simulation. Participants self-reported Rate of Perceived Exertion (RPE) before and after each simulation. Activity levels (g-force) and physiological parameters were monitored throughout.
PASAT performance demonstrated time-dependent effects independent of physical exertion, while REMT showed no significant differences between OPA and REST. RPE was significantly higher pre-simulation in the OPA arm but showed no significant differences between conditions by simulation end. The OPA simulation produced a significantly higher level of physical activity (g-force) and physiological responses compared to REST at the beginning but no significant differences by the end of simulation.
OPA significantly affects initial perceived exertion in paramedic students, while cognitive performance shows nuanced responses. The timing of cognitive assessments appears more influential than physical exertion. Further research is needed to better understand these relationships.
Modern health care is characterised by a diverse group of providers who work across complex systems to deliver quality care to patients. Among these providers, paramedics stand out due to the unique challenges they face in the out-of-hospital environment. As a result, paramedics arguably have one of the most cognitively and physically demanding jobs in the healthcare field [1]. Paramedics face unique challenges in this environment with evidence of higher rates of injuries and illness markers compared to the general population [2,3]. While younger paramedics may exhibit resilience to physical demands, performing well clinically in scenarios even after acute physical exertion [4], there are concerns about the ability of more experienced but potentially less physically fit paramedics to maintain performance under similar conditions.
In addition to physical challenges, paramedics face cognitive demands that require rapid decision-making under high-stress conditions with limited information. The dynamic and unpredictable nature of emergency medical services demands that paramedics maintain acute situational awareness, process complex information quickly and make critical decisions that can significantly impact patient outcomes [5]. Stressful situations can impair cognitive processes, affecting decision-making, situational awareness and problem-solving abilities [6,7]. Moreover, the constant exposure to time pressure and the need to perform in any circumstance or environment can lead to cognitive fatigue and increased stress levels. This may be further influenced by physical activity associated with patient care [8]. Findings from a systematic review of paramedic cognitive load determined that there is an agreement in terms of what factors influence cognitive load in paramedical contexts, such as cognitive processes, task complexity, level of experience, multiple types of loads and the use of equipment [6] These factors can potentially impair judgement and decision-making capabilities, highlighting the importance of understanding the demands placed on paramedics in their line of duty [9].
High-fidelity simulation provides the optimal arena to observe paramedics’ reactions to contextually valid conditions [10–12]. While simulation effectively supports paramedicine education [13] few studies have examined neurocognitive, perceived exertion and physiological responses to occupational physical activities in this population. The relationship between neurocognitive performance, perceived exertion and physiological markers may differ among professions, necessitating specific investigation in the context of paramedic duties. Understanding these relationships is crucial for enhancing our knowledge of the demands faced by paramedics and their potential impact on performance and well-being.
Building on previously published data from a study of the effects of occupational physical activity (OPA) on paramedic student clinical performance [4], this study examines the effects of contextually valid OPA on key measures of neurocognitive performance (Paced Auditory Serial Addition Test [PASAT] and Repeatable Episodic Memory Test [REMT]), self-reported Rate of Perceived Exertion (RPE) and how these interact with physiological responses (heart rate [HR] and respiratory rate [RR]) in a high-fidelity simulation setting. This pilot study aims to inform research design and methodologies for future studies.
Students or recent graduates (less than 6 months since graduation) were recruited through information distributed on the university paramedic student Facebook page. Approximately 120 students were eligible for inclusion, and those interested were asked to contact the researcher by email. Informed consent was obtained from all participants, who could withdraw from the study at any time. Ethical approval for this study was granted by the Charles Sturt University Human Resource Ethics Committee (number H16006).
This pilot randomized cross-over design had each participant acting as their own control. The intervention involved physically exerting participants immediately prior to a high-fidelity simulation (OPA) involving the management of a medically ill patient, compared to having the same participants rested prior to a similar simulation (REST). All testing was completed on the same day. The methodology for this study has been published previously [4].
There were 11 participants in total: 7 regional male (mean ± standard deviation [SD]: age 23.12 ± 2.12 years., BMI 25.11 ± 3.18 kg/m2) and 4 regional female (23.33 ± 3.30 years, BMI: 26.0 ± 5.16 kg/m2) final-year paramedicine students or recent graduates. There were no significant differences by gender in age or body mass index (BMI) results.
1.The 11 participants were selected based on the following inclusion/exclusion criteria and orientated to the research project. Paramedic students and recent (within 6 months of graduation) graduates were invited to participate in the study by advertisement on the paramedic student Facebook page of a regional Australian university. Those interested were asked to contact the lead researcher by email. Exclusion criteria were:
a.Gravid females; b.Student paramedics either not undertaking their final year of study or not recent (within six6 months) graduates; c.Those reporting a musculoskeletal injury within the past 6 months; d.Those currently taking HR-limiting medications, specifically beta-blockers and/or calcium channel blockers; e.Those not deemed fit to participate in high-intensity physical activity via an Adult Pre-Exercise Screening Tool (Exercise and Sports Science Australia).
The research team organized a time for each participant to attend the university simulation centre for orientation and simulation performance. Participants were given a detailed briefing on the study’s objectives, procedures and the use of simulation equipment. Each participant was tested in both simulations on the same day with a minimum rest period of 3 hours between simulations (see Figure 1).

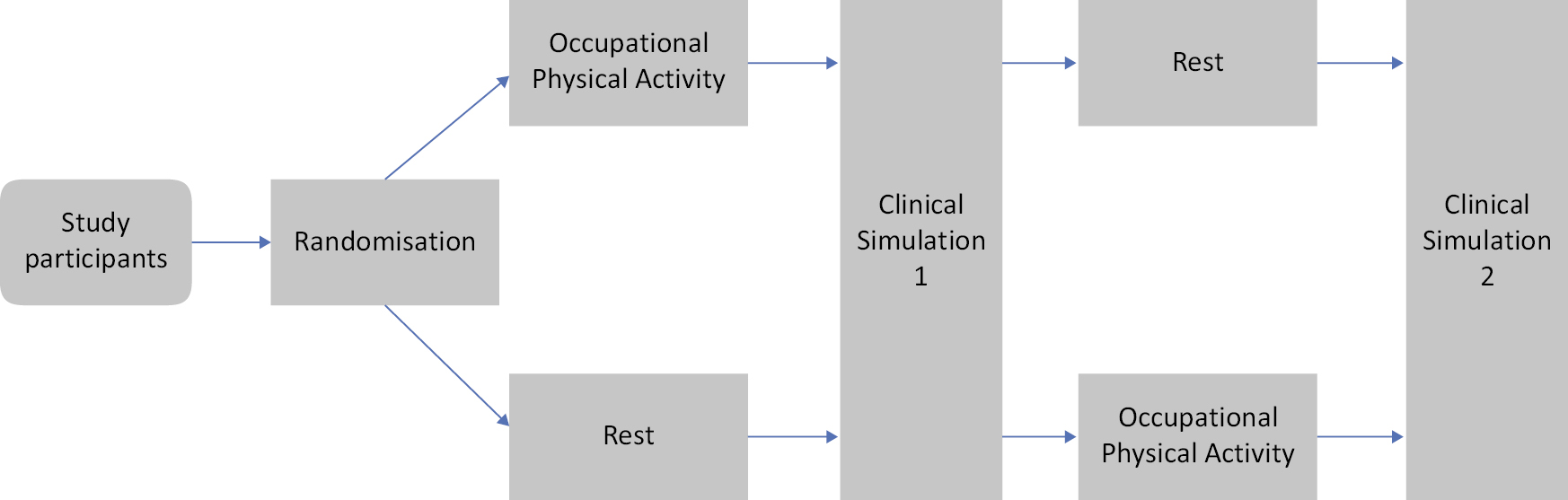
Flowchart of study protocol.
2.Simulation testing took place at the Interprofessional Simulation Centre at the Bathurst campus of Charles Sturt University and involved two separate scenarios: a male with chest pain and a female with shortness of breath. Scenarios were developed by the lead author and validated by two other paramedic academics and drawn from scenarios previously used in the programme. The chest pain scenario involved assessing and managing a patient with suspected myocardial infarction, while the shortness of breath scenario involved managing a patient with acute respiratory distress.
3.Participants wore student uniforms with a previously validated [14] Hexoskin biometric shirt (Carre Technologies, Montreal, PQ) underneath their uniform shirt to continuously record HR, RR and physical activity (g-force).
4.Participants’ mean arterial pressure (MAP) was measured immediately before and after each simulation using the iHealth blood pressure cuff (iHealth, Pomona, CA). Each participant also reported RPE at these same time points using the scale of Borg [15].
5.Patient care equipment, including a monitor/defibrillator (Lifepak 15, Medtronic Physio Control, Redmond, OR), Oxyviva and stretcher, was supplied. Participants were oriented to the manikin and its features prior to starting each simulation. The equipment supplied was identical to that used by each participant during their undergraduate paramedic training.
6.Participants were then given pre-arrival patient information consistent with that which would be relayed by dispatch for a medical call, via two-way radio.
7.Participants had a paramedic partner who assisted with equipment operation and patient care tasks but did not make clinical decisions, ensuring the participant remained the primary decision-maker. The partner was knowledgeable in how to operate all patient care equipment.
8.Each call was a medical scenario developed in consultation with, and validated by, paramedic educators at the university. Assessments and treatments followed NSW Ambulance protocols. Each participant was randomised to either the OPA or REST first.
9.After a washout period of 3 hours, the participant took part in the second call. The call was either OPA (if REST completed first) or REST (if OPA completed first).
10.Participants completed two cognitive tests prior to each simulation (Time 1): the PASAT [16] to measure sustained and divided attention, and the REMT [17] to measure short-term memory. Each of these tests was repeated immediately after each simulation (Time 2) and then at a time point 60 minutes post-simulation (Time 3). These tests are useful in measuring cognitive function in emergency services subjects and the general population [17,18].
OPA compared to rest (REST): The OPA protocol comprised the participant being provided with two 18-kg-weighted bags (a total of 36 kg) and instructed to walk approximately 100 m and then ascend and descend one flight of stairs twice as per the NSW Ambulance Trainee Paramedic Physical Fitness Assessment [19]. They were then dispatched to the simulation of a medically ill patient immediately upon completion. The REST protocol began with the participant sitting quietly in a chair for at least 5 minutes prior to being dispatched to a similar medical call with no participant significant physical activity during that period.
Physical and physiological measures: HR and RR were collected using a previously validated biometric shirt (Hexoskin, Carre Technologies, Montreal, PQ, Canada) [14]. The biometric shirt was worn by participants throughout the simulations to continuously record HR and RR. Wrist-based non-invasive blood pressure was measured using the iHealth device (iHealth, Pomona, CA) immediately before and after each simulation.
Participants’ height (in metres) and weight (in kilograms) were measured to calculate BMI utilizing the formula BMI = weight/height2 [20].
RPE was measured using the 0–10 Borg RPE scale before and after each simulation [15].
The PASAT and REMT were scored according to methods reported previously [16,21].
Data were inspected visually and statistically for normality using visual inspection of Q–Q plots and the Kolmogorov–Smirnov test prior to analysis. Results are presented in graphs as mean and 95% confidence intervals. Neurocognitive test results (PASAT and REMT) were analysed using repeated-measures analysis of variance (ANOVA), comparing the OPA and REST groups across time (Pre, Post and 60 minutes post). When a significant main effect was found, post hoc comparisons were conducted using the Tukey HSD test to identify specific group differences. Null hypotheses were rejected at p < 0.05. Statistical analysis was carried out using Jamovi v 2.3 (The Jamovi Project, 2023).
Physiological responses (HR, RR, MAP) to the OPA and REST conditions have been previously reported [4]. Briefly, mean HR (p = 0.001), maximum HR (p = 0.04) and mean RR (p < 0.001) were significantly higher in the OPA simulations than the REST simulations. Blood pressure (MAP) was significantly higher at the start of the OPA simulations than at the start of the REST simulations (p = 0.01), but not significantly different post-simulation (p = 0.36). Here, we focus on the novel neurocognitive outcomes of this study.
There was no significant main effect of study arm (F (1,10) = 1.36, p = 0.271, η²p = 0.120), nor was there an arm × time interaction (F (1,10) = 1.47, p = 0.254, η²p = 0.128). There was an effect of time (F (1,10) = 3.57, p = 0.047, η²p = 0.263). Figure 2 shows that this effect was largely driven by a reduced PASAT score in the OPA group before the simulation started. Simple-effects analyses revealed that the effect of time was only significant in the OPA group (p = 0.049) not in the REST group (p = 0.982). Repeated contrasts revealed a significant increase in PASAT from pre-simulation to post-simulation (p = 0.020), suggesting that a reduced PASAT from the physical exertion showed recovery during the medical simulation. See Figure 2.

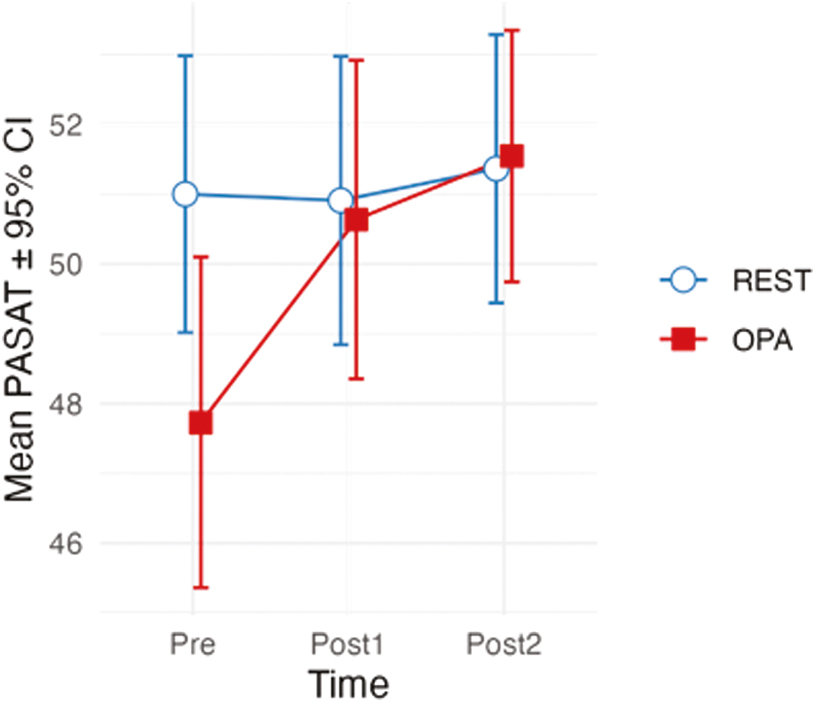
Mean PASAT scores with 95% confidence intervals before a simulation (pre), after the first simulation (post1) and after the second simulation (post2).
There was no significant main effect of study arm (F (1,10) = 3.72, p = 0.083, η²p = 0.271) or time on REMT scores (F (1,10) = 1.15, p = 0.336, η²p = 0.103), nor was there an interaction (F < 1, η²p = 0.058).
There was a significant and strong main effect of study arm (F (1,10) = 15.70, p = 0.003, η²p = 0.611), but no main effect of time (F < 1, η²p = 0.015). Figure 3 shows a strong significant interaction (F (1,10) = 17.97, p = 0.002, η²p = 0.642). Simple-effects analyses revealed that the OPE group reported significantly higher RPE before the simulation (Mdif = 2.72, p = 0.002) but no difference post-simulation (Mdif = 0.09, p = 0.676). Across the simulation, there was a significant increase in RPE for the REST arm of the design (Mdif = 1.46, p = 0.005), but a significant decrease in RPE for the OPA arm (Mdif = −1.18, p = 0.046).

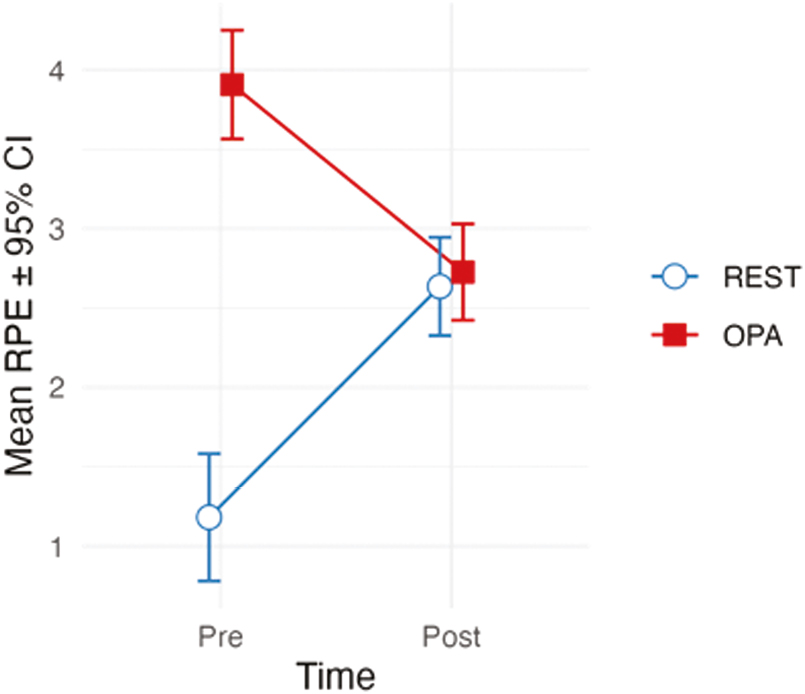
Mean RPE with 95% confidence intervals pre- and post-simulation.
There was a significant difference in average g-force by study arm (p < 0.001), indicating higher average physical activity for OPA compared to REST (d = 1.66; medium effect size). The difference in maximum g-force approached but did not reach statistical significance (p = 0.059), with a medium effect size (d = 0.516). See Figure 4.

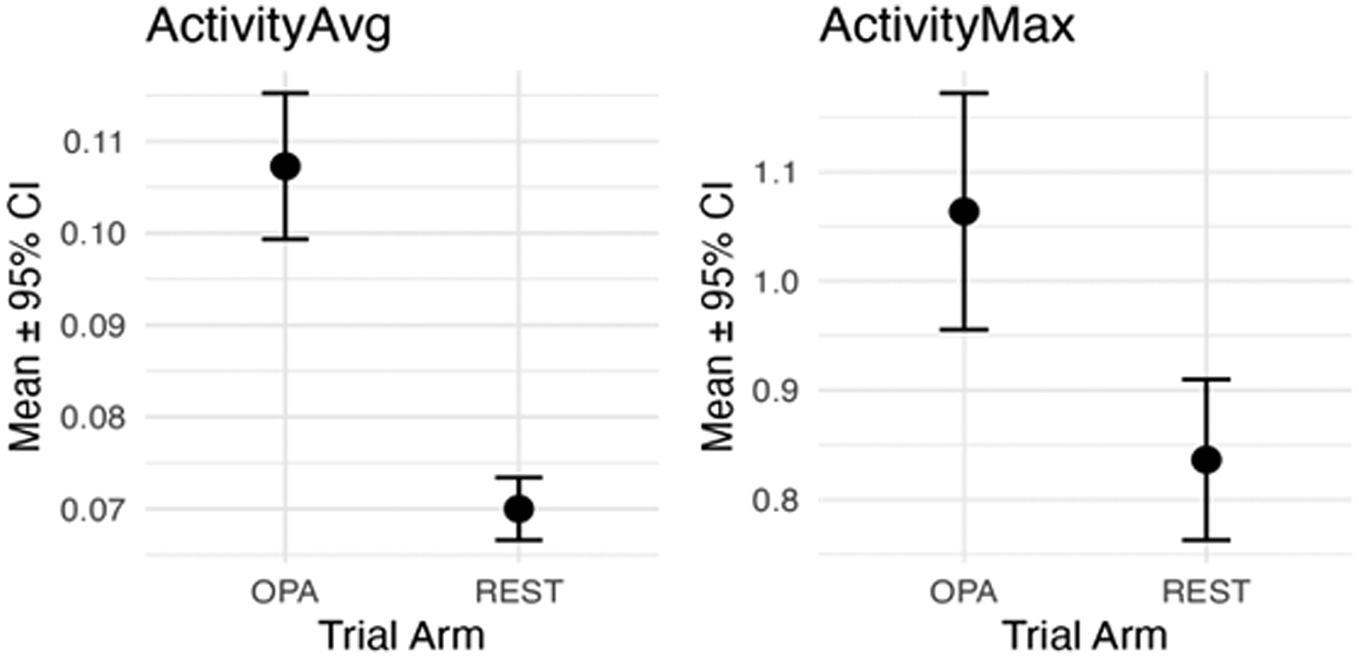
Activity data expressed as units of average (left panel) and maximum (right panel) g-force (mean with 95% confidence intervals) for the OPA group and REST group.
This pilot study aimed to build on previous work by examining the effects of contextually valid OPAs on paramedic students’ neurocognitive performance, self-reported exertion and physical activity (g-force) in a high-fidelity simulation setting. The findings demonstrate nuanced responses in cognitive performance following OPA, with significant differences in perceived exertion at the start of each trial arm. OPA, as measured by g-force production, significantly impacts physiological parameters in participants.
The cognitive performance results reveal a complex relationship between physical exertion and mental function over time. PASAT scores showed significant time-dependent effects, while REMT performance was not influenced by trial arm, time or their interaction. This suggests that different cognitive domains may respond distinctly to physical stress in paramedic settings.
The timing of cognitive assessments appeared more influential than physical exertion for PASAT scores, which measure sustained and divided attention. This finding contrasts with studies in other emergency service professions. For instance, Hemmatjo et al. (2018) found significant decreases in PASAT scores among firefighters following simulated firefighting activities [22]. The discrepancy may be due to differences in the intensity and duration of physical exertion between paramedic and firefighting tasks. Firefighting activities typically require higher levels of aerobic fitness, muscular strength and endurance compared to standard physical paramedic activities.
Using more physically demanding paramedic tasks (e.g. extricating a heavy adult patient from a difficult location) prior to conducting a neurocognitive assessment such as REMT or PASAT may be more appropriate. While comparisons to firefighting activities are informative, they may not fully capture the distinct cognitive challenges faced by paramedics.
Higher initial RPE scores in the OPA condition suggest that participants were acutely aware of their increased physical exertion prior to beginning the simulation. This self-awareness is important for understanding the relationship between physical demands and cognitive function in paramedic settings. The measurement of activity (g-force) confirms that physical activity was significantly higher in the OPA arm compared to REST. Interestingly, while initial RPE scores were elevated in the OPA condition, they did not correspond to decrements in cognitive performance as measured by the PASAT and REMT tests at time points 2 and 3. This discrepancy aligns with previous research suggesting that the relationship between RPE and cognitive function is complex and influenced by various factors. The lack of significant difference in RPE scores at the end of the simulations suggests that participants may have recovered from the initial exertion during the course of the simulation. This recovery pattern is consistent with findings from MacQuarrie et al., who observed that younger paramedics exhibit resilience to physical demands in simulated clinical scenarios [4].
The OPA simulation elicited significantly higher pre-simulation physiological measures (HR and RR) compared to the REST condition. This aligns with previous research showing that physical exertion in emergency responders leads to acute increases in cardiovascular and respiratory parameters. Interestingly, these differences normalised by the end of the simulation, suggesting a rapid physiological recovery in this young, relatively fit cohort.
There are few simulation-based studies of paramedics or paramedic students to compare these results with. While studies have examined the effect of alarms on physiological arousal for responding paramedics and firefighters [23], the addition of physical tasks could be expected to increase HR, BP and RPE, although this has not been empirically demonstrated.
Both simulations were designed to present the participant with a seriously ill patient, ensuring significant cognitive and physical demands [including Cardiopulmonary Resuscitation (CPR)]. It is anticipated that more gravely ill patients elicit a higher physiological response in healthcare providers [24]. The evidence of increased HR, RR and MAP scores in participants was higher in the OPA simulation, indicating that the physical workload prior to the simulation made a significant contribution. Additionally, there were no significant differences in Global Rating Score (p = 0.07, Effect Size = 0.03) or CPR efficacy between arms; however, Patient Care Report accuracy was higher after the OPA versus REST simulations [4].
While this pilot study provides valuable insights, it has several limitations. The homogeneous sample of young, relatively fit paramedic students may not represent the broader paramedic population. Future research should include larger, more diverse paramedic cohorts, including experienced professionals with varying fitness levels.
The study included 11 participants instead of the 12 determined a priori, so results should be interpreted with caution. Additionally, the OPA protocol used in this study, based on a pre-employment fitness test, may not fully reflect the range of physical demands encountered in real-world paramedic work. Future studies could incorporate more varied and realistic physical tasks to better simulate occupational demands.
While a 3-hour washout period was used in this pilot study, recent research suggests longer recovery times may be needed when assessing paramedic cognitive performance after stressful simulations. Future studies should consider extending the washout period to account for prolonged physiological stress responses.
This pilot study establishes a sound methodology for investigating the complex interplay between physical exertion, cognitive performance and physiological responses in paramedic settings. The findings highlight the nuanced effects of occupational physical activities on neurocognitive function and perceived exertion, providing valuable insights for paramedics and paramedic services about the anticipated demands of job performance. The observed relationship between physical exertion and cognitive performance suggests that incorporating physical tasks before simulation training could better prepare students for real-world demands These insights can guide the development of targeted training programs aimed at enhancing paramedic operational resilience and performance under stress.
While this pilot study included 11 participants from a relatively homogeneous group of young, fit paramedic students, future research should examine a broader demographic spectrum of paramedics. Studies with larger sample sizes and a more diverse cohort should investigate how factors such as age, experience level, and varying fitness levels influence the relationship between physical exertion and cognitive performance. This expanded scope would provide more comprehensive insights into paramedic performance under occupational stress.
The authors wish to acknowledge Mr Duncan Webley, Ms Clare Sutton, Ms Samantha Sheridan and Ms Amanda Hlushak for assistance in data collection and scoring. We also wish to thank the Interprofessional Simulation Centre staff at Charles Sturt University for their technical support during the study.
None declared.
None declared.
None declared.
None declared.
The authors report there are no competing interests to declare. The authors did not use a generative artificial intelligence (AI) tool or service to assist with preparation or editing of this work. The author(s) take full responsibility for the content of this publication.
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.