
Atypical sensory processing is a difficulty in regulating and managing sensory input in a meaningful way. Sensory processing disorder (SPD) is common in individuals with autism spectrum disorders (ASD), pervasive developmental disorders, specific learning difficulties (SpLD) and neurodiversity.
The Experiencing Sensory Overload simulation aims to champion inclusive practice and reduce health inequalities by encouraging student nurses to reconsider their working environments to create sensorily safe spaces for individuals who experience SPD. This paper explores the impact of the transformative simulation on nursing students’ confidence and knowledge of sensory overload and inclusive practice.
A quasi-experimental method with pre- and post-simulation surveys and a written reflection was utilized. A convenience sample of 26 BSc Nursing students was recruited to this evaluative first-stage assessment of a new simulation. Data were gathered from participants about the value of engaging with the simulation. Questionnaires using a Likert score to explore experiences, knowledge and confidence about neurodiversity, ASD, and sensory overload were administered. Participants also submitted a short, written reflection examined via reflexive thematic analysis.
The Likert data show a clear shift in pre- and post-knowledge. The calculated median of pre-experience knowledge was 4.5, rising to a median of 8 post-experience. 90.5% of participants would recommend this simulation. Reflexive thematic analysis of qualitative data derived three themes:
‘The penny dropped’ – Understanding/awareness
‘Walking in someone else’s shoes’ – Appreciation of uniqueness of experience for individuals
‘Ask, listen, do’ – Strategies to adapt and inform practice
The participants enhanced their understanding of the challenges of sensory overload, envisaging reasonable adjustments to ensure inclusive practice. The authors believe that this simulation is effective and will positively impact nursing students’ ability to care for neuro-diverse individuals.
What this study adds:
Champions experiential learning via simulation.
Highlights the importance of reasonable adjustments in practice to ensure equality of access for diverse service-users.
Increases knowledge of autism spectrum disorders, pervasive developmental disorders and sensory processing disorders.
Atypical sensory processing is described as a difficulty in regulating and managing sensory input in a meaningful, ordered way to make sense of the world and environment in which you find yourself [1]. Sensory processing disorder (SPD) is common in individuals with autism spectrum (AS), pervasive development disorders and neuro-divergent conditions [1]. Sensory overload has been described as ‘being tuned into 40 different TV channels at once’, a ‘feeling of fragmentation, when thoughts, feelings and behaviours are scattered or competing for attention’ and a ‘loss of self within all the competing demands’, and can make simple or everyday tasks difficult and emotionally and physically exhausting [2].
This is not a new phenomenon; in 1979, Ayres [3] identified that sensory integration problems were a unique developmental disorder in their own right. Ayres [3] suggested that children with sensory integration problems may be either over- or under-responsive to stimuli and therefore react differently to neurotypical children.
The prevalence of individuals identified as having SPD is marked, with Zhou et al. [4], suggesting rates are as high as 90% in children with autism spectrum disorders (ASD). The World Health Organization [5] estimates that 1 in 160 children have ASD, commenting that this is an average figure as reported prevalence varies across studies and countries and that the actual figures may be higher. In the UK, a total population sample, including all English children and young people aged between 2 and 21 years in state-funded education, was taken from the 2017 Spring School census [6]. Within these 7 million school children, the prevalence of ASD was 1.76%, with males four times more likely to present with neuro-divergence than the females in the cohort [6]. A more recent study from 2023 suggests that there are approximately 750,000 undiagnosed autistic people aged 20 and above in England [7]. If this study is correct, then the number of autistic people in England would exceed 1.2 million.
These compelling statistics highlight that it is likely health professionals will regularly meet and care for individuals with autism, SPD and other neuro-divergent conditions. The National Institute of Clinical Excellence [8] suggests SPDs are often overlooked by education, social and healthcare professionals, leading to health and social inequalities with individuals less able to access ‘support and services that they need to live independently’ [8], (p5). This is further highlighted by the LeDeR report[9], on average, an autistic male will die 22 years earlier and an autistic female 26 years earlier than the general population. An autistic adult is over nine times more likely to consider suicide compared to neurotypical adults.
The Department of Health and Social Care published ‘The right to be heard’ [10], a response to consultations on learning disability and autism. This concluded that ‘autistic people continue to experience significant disparities in the quality of care and support they receive, as well as in the outcomes they can expect (p.3)’. In response, the Health and Care Act [11] requires that organizations providing services to individuals with ASD and learning disabilities must provide appropriate training for their staff, specific to their role.
The authors recognized there was insufficient education on SPD and neuro-divergence within the current nursing curriculum [12,13,14], and wanted to explore the creation of a robust, pedagogically sound and immersive learning experience. To address this theory–practice gap, the Experiencing Sensory Overload (ESO) simulation was developed.
The first step was to consider the learning outcomes, aims and objectives for the simulation and ensure that these aligned with the Nursing and Midwifery Council (NMC) [15] platforms within the Future Nurse Standards. The NMC is the regulatory body that promotes and maintains high standards of practice for nurses and midwives within the UK [16]. A key aim within the Future Nurse standards is to develop well-rounded, educated professionals able to provide compassionate, evidence-based, person-centred care [15], (p.3) that is non-discriminatory, sensitive and takes account of any need for adjustments [15], (p.9).
Whilst designing the simulation, the authors kept in mind the underpinning learning theories that provided the pedagogical approach to learning and teaching, aligning with Mezirow’s [17] theory of transformative learning. Mezirow suggests that adult learning is, by its nature, transformative as adults can appreciate how their beliefs, values and attitudes influence their position. The aim of simulation in nursing is to provide learners with a living context that encourages engagement, competency and participation to transform learning through personal experience. Kolb’s [18] theory of experiential learning further supports this approach.
The ESO simulation aims to champion inclusive practice and reduce health inequalities by encouraging professionals to reconsider their working environments to create sensorily safe spaces for individuals who may experience SPD.
ESO is an immersive experience that replicates sensory overload whilst students complete seemingly simple tasks. A confined space with intrusive lighting, sound effects and smells assails students’ visual, auditory and olfactory perception whilst their vestibular and proprioception senses are challenged throughout. Fine motor control and visual perception are altered, impacting dexterity. The tasks are performed under time pressure and rely on swift processing and retention of instructions to complete.
A further immersive Virtual Reality (VR) experience was developed to give the students a sense of how sensory overload might feel from the perspective of a neuro-diverse child navigating an adult world. The simulation helps participants understand the challenges autistic individuals and others with specific learning disabilities (SpLD) may face day to day in a world designed for neurotypical people. The design arose after consultation with experts by experience and in accordance with ASPiH’s taxonomy of Seven Simulation-Based Interventions (Table 1) [19].

| Seven SBIs | ASPiH definition | ESO Simulation Application |
|---|---|---|
| Innovation | Introduction of novelties; the alteration of what is established. | Novel simulation approach to give learners an experience of sensory overload whilst completing ‘simple’ tasks |
| Improvement | Making something better; becoming better; an addition or alteration to make change for the better. | To improve the care of patients with autism and/or learning disabilities, who may experience sensory overload in healthcare settings. |
| Intervention | The action of intervening or interfering in any affair to affect its course or issue. | To reduce anxiety and behaviours of distress in vulnerable patients, to enable safe and effective healthcare delivery. |
| Involvement | The process of involving; being involved; being implicated, entangled or engaged. | Encouraging learners to recognize, through simulation, how they can challenge or intervene in practice to create sensorily safe spaces for care. |
| Identification | The act of identifying; what or who; discovery and recognition. | Encouraging learners to reframe anxiety and behaviours of distress by identifying environmental stressors and/ or stressful care approaches. Identifying simple changes to the environment and/ or approach that can lessen stress responses. |
| Inclusion | The action or an act of including something or someone; the fact or condition of being included. | Including patients, families and carers to identify calming strategies and/ or reasonable adjustments in practice |
| Influence | To exert influence; to work influentially on, upon person(s) or thing(s). | The ESOS aims to influence learners approaches to patients who are experiencing, or who may experience sensory overload in healthcare settings. |
The ESO simulation invited BSc Nursing students to experience and evaluate the simulated learning experience. The purpose was to test the experiential design and provide an impetus for further development and refinement of the simulation. A more detailed account of the simulation is reported within Table 2, and key elements to report for simulation-based research in accordance with the CONSORT/STROBE Guidelines [20].

| Elements | Sub-elements | Descriptor – ESO Simulation Application |
|---|---|---|
| Participant orientation | Orientation to the simulator | Students were introduced to the instructors and the environment Explanation of using VR and safety considerations explained verbally and via printed instructions |
| Orientation to the environment | Introductions to the confined environment with low lighting and uneven surface Length of simulation clearly set with ‘stop for real’ provision highlighted |
|
| Simulator type | Simulator make and model | Fully immersive confined space Oculus Meta 2 VR headsets |
| Simulation environment | Location | Confined space room within Simulation Centre |
| Equipment | Oculus Meta 2 VR headsets x 4 Wobble cushions x 4 Clinical & gardening gloves x 4 pairs Adapted safety glasses to simulate visual impairment Timers x 4 Pens & notepaper Building blocks sets x 4 Plastic tweezers x 4 |
|
| External stimuli | Alternating coloured lights Intrusive Noise soundtrack Aromatherapy atomizer |
|
| Simulation event/ scenario | Event description | VR film from the perspective of a neuro-diverse child navigating an adult world Confined Space Simulation: Four simple tasks undertaken with time pressure, intrusive lighting sounds and smells. Simulation of vestibular and proprioception senses using a wobble cushion |
| Learning objectives | For professionals to reconsider their working environments to create sensorily safe spaces for individuals who may experience SPD | |
| Group/individual practice | Individual but group discussion encouraged during debrief | |
| Facilitator characteristics | 1: Registered Children’s Nurse, Registered Nurse Educator, MA.Ed, PGCert in Higher Education, PG Cert in Research Methods, SFHEA, SEDA, and Expert by Experience 2: Registered Adult Nurse, Registered Nurse Educator, MA.Ed, PGCert in Higher Education, PG Cert in Research Methods, SFHEA, SEDA, and Expert by Experience |
|
| Pilot testing | This study is an evaluative first stage assessment of a new simulation. | |
| Instructional design | Duration | 1.5 hours Pre-brief: 15 minutes VR Film: 15 minutes Immersive Simulation: 15 minutes Debrief: 45 minutes |
| Timing | Data collected pre-simulation and immediately following debrief Reflective account submitted 10-days after the simulation |
|
| Integration | Evaluative first stage assessment prior to integration into the curriculum | |
| Feedback/debriefing | Source | Verbal discussion |
| Duration | 45 minutes | |
| Facilitator presence and characteristics | Yes x 2 Facilitators as above |
|
| Content | Experience of sensory overload | |
| Structure/method | ASPiH Diamond Debrief | |
| Timing | Terminal | |
| Video | No | |
| Scripting | No |
Ethical approval was granted via the University College of Health, Life and Environmental Sciences Research Ethics Panel, reference HS22230010.
A convenience sample of 26 student nurses was recruited to undertake the simulation, and their consent to participate was recorded. These student nurses represented Adult, Child and Mental Health fields of practice and years 1–3 of study. Participants expressed an interest and submitted a brief rationale on why they should be selected. As the purpose of the research was to test a teaching concept and further develop the learning resources, the authors felt that using a convenience sample, with its inherent problems of generalizability, was acceptable [21] for this first-stage evaluative study.
A quasi-experimental survey method with pre- and post-session survey was chosen. Groves et al. [22] suggest this is a pragmatic, systematic approach to data collection for the purposes of evaluating a learning experience. This allowed quantitative and qualitative data to be gathered from participants about the perceived value of engaging with the simulated learning experience. The ease and user-friendly nature of a short survey was deemed an important consideration for both participants and the researchers [23].
This questionnaire was developed by the authors and piloted through this first-stage evaluation to ensure its reliability and validity, to ensure it was clear and comprehensible, and gleaned quality responses [24]. The questionnaire used a Likert score to answer a series of questions about experiences, knowledge and confidence about ASD and sensory overload, and was administered before and after engagement with the simulation. Likert scores are a simple scale that asks respondents to rate their strength of feelings or attitudes across a range [25]. Students were asked to rate their knowledge and understanding of ASD and SPD before and after the simulation using a Likert score to produce ordinal data. The Likert score ranged from 0, depicting no knowledge, to 10 expert knowledge. In this context, the authors use the term expert to denote an expert by experience. The Care Quality Commission defines an expert by experience as someone using health and social services themselves or caring for someone who is [26].
Students were also asked to submit a short reflective piece about their learning and its application to their practice 10 days after the simulation experience occurred. Some guidance and prompt questions were given for the students to consider within their reflections so that across the submissions, there would be some commonalities to build from. Reminders were sent by email on day 5 and day 8 post-simulation. Reflective accounts are extensively used in nursing and education to encourage the writer to build competence by focusing on tacit knowledge and inspecting what they know and how they know it [27] (p.266), [28]. Reflection as a qualitative methodology allowed the researchers to cross-examine the learning links that students made for themselves. Rolfe [29] suggests that the unique body of knowledge that an individual builds can only be accessed by writing. Smith [30] further qualifies this, explaining that writing reflexively encourages a cognizant dialogue between lived experience and knowledge.
Braun and Clarke’s [31,32] method of reflexive thematic analysis was employed to analyse the reflections as qualitative data. The 22 reflective accounts were read several times by each researcher, firstly to familiarize themselves with the ‘data corpus’ and later to highlight key words and phrases from ‘data items’ [31]. The researchers shared and discussed their approaches to the student reflections, highlighting key themes and then cross-referencing with the other researchers’ set. This initial examination of the data set by each researcher and subsequent dialogue between the researchers was an important first step to identify and describe the data. The authors continued discussions of their positionality, preconceptions and assumptions informing their interpretation of the data. Koch [33] comments that this is an important step in reflexive thematic analysis, as it cannot be assumed that there would be perfect agreement between two interpretations of the data. The ‘active role’ the researchers take in identifying themes should be acknowledged, particularly if researchers are claiming a reflexive thematic analysis approach [32].
Following this first step, commonalities and differences in the researcher’s interpretations of the data were highlighted in accordance with Braun and Clarke’s [32] reflexive thematic analysis approach. Surprisingly, differences were relatively few and quickly resolved within the reflexive process. This homogeneity confirmed the authors’ alignment and gave some reassurance that the students’ reflective accounts were understood.
Twenty-six participants consented to participate in the study. Twenty-two students returned the survey and associated reflection (n = 22), an 84% response rate.
The Likert data show a clear shift in students’ pre- and post-knowledge levels (Figure 1). Quantitative data analysis using the Mann–Whitney U test [34] supports that the difference between pre- and post-test is large enough to be statistically significant with a P-value of 0.004 [35] with a confidence interval of 95% [36]. The calculated median of pre-experience knowledge was 4.5, rising to a median of 8 post-experience. As the pre-test scores were lower than the post-test survey, which were conducted immediately after the simulation[35], the authors can assume that this is attributable to the educational intervention.

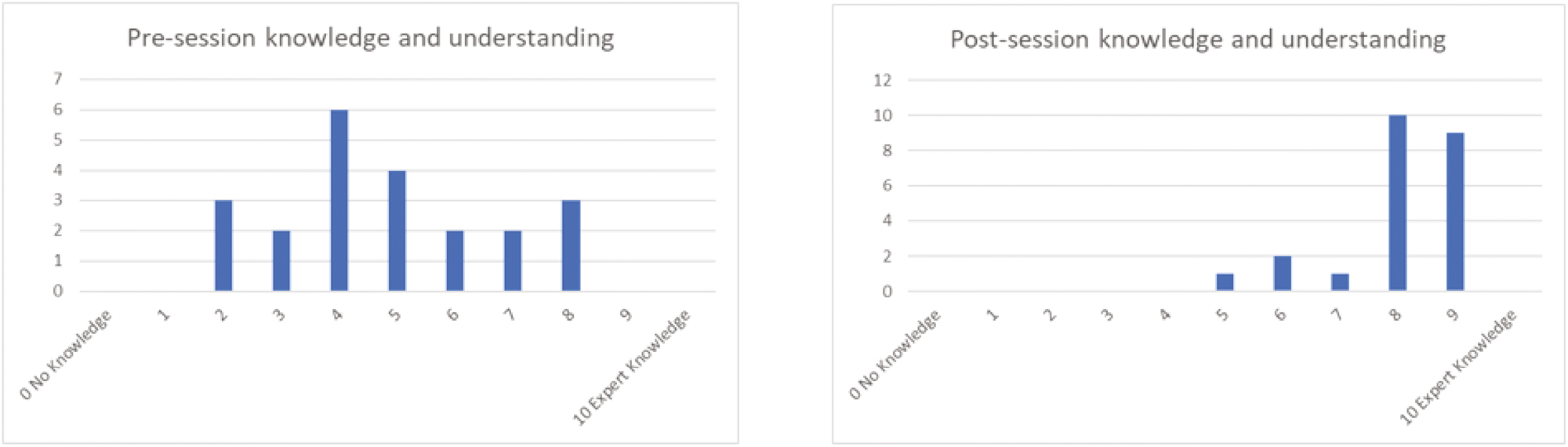
Prior knowledge and post sim knowledge shift
When participants were asked if they would recommend this experience to others, 86% would most definitely recommend, 5% would recommend and 9% failed to answer this item.
The reflective accounts were submitted 10 days after the simulation occurred. Twenty-two students (n = 22) submitted a reflection, an 84% response rate. The six-step reflexive thematic analysis method developed by Braun and Clarke [32] was utilized to provide a systematic approach to the data. The cognitive schema that led to the final themes is evidenced in Figure 2.

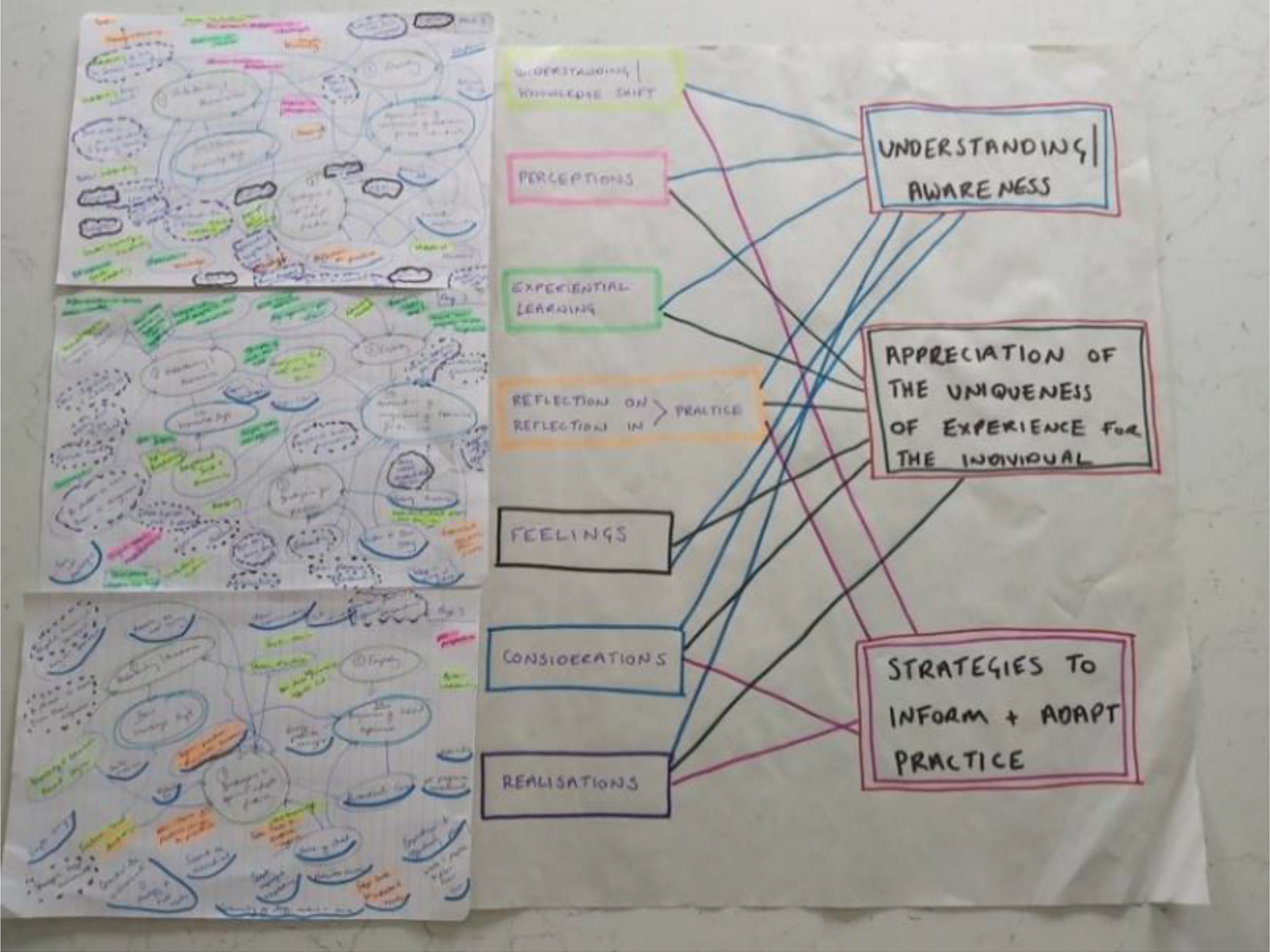
Cognitive schema
The final agreement resulted in the themes of:
‘The penny dropped’ – Understanding/awareness,
‘Walking in someone else’s shoes’ – Appreciation of uniqueness of experience for individuals
‘Ask, listen, do’ – Strategies to adapt and inform practice
Once the three themes were agreed, the reflections were re-read, using unsullied papers to confirm that the themes were truly reflective of the data set. The researchers again identified and recoded the reflections using the three established themes. Braun and Clarke [31] describe this as level two refinement; ‘the need for recoding from the data set is to be expected as coding is an ongoing organic process’ [31] (p.21). Once refinements no longer added substantial meaning the process was concluded.
The researchers conclude with some certitude that the themes reflect the students’ accounts following this process.
Considering the research question and focus of this piece, ‘Walking in someone else’s shoes – Can a transformative simulation help student nurses comprehend sensory overload’? It is important to consider the resultant data and final themes, in the context of the students’ experience of the learning resource, to ascertain its effectiveness.
All students reported a clear shift in their knowledge of ASD and SPD, and some insightful observations were shared. Students documented a ‘Penny dropped’ moment of clarity and a new appreciation of the experience of individuals with SPD.
A student highlighted how their awareness and outlook had been altered following the experience ‘Even though I live with someone, I didn’t understand’. The authors found this particularly poignant and felt it reinforced the need for immersive education and simulation that challenges the individual’s affective domain to create a conscious change [29]. Students identified that their pre-perceived expectations were challenged throughout the experience. Greater insight, appreciation, and a heightened sense of knowledge and understanding were reported.
A strand of discussion related to the understanding that each child or individual is unique, with individual needs. ‘A person is more than their diagnosis’ and the opportunity to ‘experience a short time in someone else’s shoes’ through this experiential learning affected the participants’ understanding in a transformative way.
Theme two overlapped with theme one, but was perceptible in that students particularly emphasized the uniqueness of experience. One student summarized ‘If you have met one person with SPD, you have met one person with SPD’.
Students had an appreciation that you need to ‘meet people where they are at’ and that you ‘must listen to their story and give them a voice’. It allowed them to ‘walk in someone else’s shoes’.
The experiential element of the simulation particularly impacted, giving students a ‘heightened sense of awareness of what people with sensory overload experience on a daily basis’, and how ‘overwhelming’ and ‘distracting’ this can be. One student commented that ‘I could tell myself it was a temporary experience; it would soon be over’. ‘It gave a new appreciation of how unfair global expectations are’.
The authors consider this theme as the culmination of the students’ learning that offers them a new conceptual framework when caring for individuals with SPD, ultimately impacting clinical practice. Students recognized that they would adapt and adjust their practice to ‘consider the environment to meet the needs of an individual’. They would ‘share new ideas for positive change to inform those around them’.
Students highlighted the power of ‘simple, impactful adaptations’ that could positively affect the experience of healthcare for an individual with SPD.
Students emphasized the importance of ‘support for the individual’, ‘stepping back and giving a voice to a patient’s preference when planning care rather than assuming the clinician knows best’,
The clear message of ‘Ask, listen, do’ was recurrent in the student’s narratives, with the emphasis being on personalized care that considers reasonable adjustments, resulting in safe, effective health care.
It was clear from the thematic analysis of the reflective accounts that the simulation was impactful on the students’ learning and positionality. The shift in knowledge, thinking and outlook that was evidenced in participants’ narratives aligns nicely with Krathwohl, Bloom and Masia’s [37] affective domains, where experiential learning effects a shift [17], directly impacting a participant’s behaviours, attitudes and awareness. In causing a shift in the students’ affective domain, the learning becomes transformative.
The authors felt reasonably confident that in terms of the affective domains, students were ‘organizing’ and ‘combining’ a new value to give it priority. What is less certain is whether students would consistently act utilizing their new values to adjust their practice in the longer term. It is beyond the scope of this first-stage study to make such claims, particularly in the longer term; however, it is hoped this might be the subject of future research.
Reflection was an essential element of the learning process, with students encouraged to reflect and discuss their learning with peers during the simulation. This was supported by the later written reflection so that the students could make links between the experience and the content, integrating these with their prior skills and knowledge to ensure the development of a more complex, nuanced understanding of how sensory overload can impact an individual. Mezirow and Taylor [38] note that ‘engaging with reflection in concert with experience ... provides the means by which learners transform the way they think ... [38] (p.285).
In developing the learning experience, the authors were mindful of the learning outcomes and their constructivist learning and teaching approach. Aligning to the five values espoused by Langan, Sheese and Davidson [39], Figure 3 helped guide the simulation design and was useful in creating a transformative learning resource. All five of these values are intrinsically placed within the learning experience and align with ASPiH’s four core values [40].

![Constructive teaching and learning: five values (Langan et al. [39])](/dataresources/articles/content-1755092404266-bb8f1ba7-847e-4583-bdc1-a9df4f2e6c6f/assets/kfcd4381_f0003.jpg)
Constructive teaching and learning: five values (Langan et al. [39])
As the student sample was small, caution should be exercised when analysing the quantitative data. Denscombe [41] comments that a sample size of less than 30 should not be used for statistical analysis without exceptional care. However, as the intention is to use the same data collection method in future evaluations of the simulation, further evidence will be added to the data set with larger sample sizes.
The authors recognize that the lower the response rate, the more likely the findings are to be biased, which will in turn limit generalizability. Burkell [42] suggests that the widely accepted level of response that is required for generalizability is 75%. The authors, therefore, consider the response rate of 84% to be a high return. This might be explained as the participants self-selected to take part and were likely to have an interest in the subject matter; therefore, they may differ from those who did not volunteer [43]. It is also important to note that there is no intention to generalize these results to the wider student population. They are intended to further develop the simulation and test the outcomes to ensure that learning was experiential and transformative as intended by the pedagogical approach.
The authors also acknowledge that the shared reflections could prove problematic; it could be argued that the students will respond in a positive way, knowing the researchers would be reading their reflective accounts, a form of social desirability bias [44]. That notwithstanding, the student’s accounts seemed genuine, offering personal perspectives and interpretations of the learning that occurred. It would be naïve to present these as anything other than a version of events and subjective in nature, but they do provide rich accounts and have the potential to be a source of additional data. Jasper[28] states that there is little debate in nursing and education about how reflection contributes to understanding, but cautions that there is limited evidence of its use as a data collection method. If, however, as Schon [45] postulates, reflection enables practitioners to draw on knowledge gained from experience, which contributes to understanding, then using reflections as data may illuminate that knowledge and how it was gained.
To aid confidence in the methods, findings and interpretation of the research, the criteria of the Mixed Methods Appraisal Tool 2018 were considered and addressed with a resultant 80% quality score (Table 3) [46]. This scoring tool should be used with caution, as in isolation it does not fully capture all nuances of the study design. However, as this is an evaluative first-stage study, it was a useful exercise to increase confidence in the process, credibility and reliability of the employed methods [46].

| 1. Qualitative | Quality Criteria 1.1 | 1.2 | 1.3 | 1.4 | 1.5 | Quality Metric |
| 1 | 1 | 1 | 1 | 1 | 100% | |
| 4. Quantitative Descriptive | Quality Criteria 4.1 | 4.2 | 4.3 | 4.4 | 4.5 | |
| 1 | 0 | 1 | 1 | 1 | 80% | |
| 5. Mixed Methods | Quality Criteria 5.1 | 5.2 | 5.3 | 5.4 | 5.5 | |
| 1 | 1 | 1 | 1 | 1 | 100% |
Each quality criteria scores 1 or 0, depicting yes or no on the MAAT. Each section has 5 quality criteria. Each score within these quality criteria gives 20%, totalling a possible 100% for each section.
As mixed methods quality indicators utilize 15 criteria to rate, 5 each of qualitative, quantitative and mixed methods, the overall quality score must be the lowest of the study components. Therefore, the overall quality metric for this first stage evaluative questionnaire is 80%.
Given the prevalence of autistic people, those with SpLD, pervasive development disorders and neurodivergent conditions, student nurses will inevitably meet individuals who are sensitive to sensory overload in acute and community care settings. To address health inequalities and prevent unnecessary deaths, it is essential that student nurses consider how and when to adjust practice to suit an individual’s needs. It is vital that consideration is given to the environments where care takes place, that potential triggers for sensory overload are reduced or removed, and that, as far as possible, a sensorily safe space is created.
The authors believe that this first stage evaluative study of a newly developed transformative simulation has been successful, confirming that the ESO simulation is an effective learning resource. It is clear from the data that the students who engaged with the simulation expanded their understanding of sensory overload and ASD. Students were able to propose reasonable adjustments to ensure inclusive practice as a result.
Although the authors recognize that further evaluative research needs to be undertaken before claims to a positive impact on practice can be made, they envisage the transformative simulation has the potential to impact positively on patient care; reducing health inequalities and challenging disparities in provision.
None declared.
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
None declared.
None declared.
None declared.
The Association for Simulated Practice in Healthcare (ASPiH) has supported the publication of this work through their fee waiver member benefit.
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
37.
38.
39.
40.
41.
42.
43.
44.
45.
46.