
Realism is a quality criterion for simulation. However, its impact on learning remains unclear. There is no consensus on how to assess realism in simulation except for virtual reality. A previous study of Brackney and Priode (Back to reality: the use of the presence questionnaire for measurement of fidelity in simulation, Journal of Nursing Measurement, 2017 Aug 1;25(2):66–73) looked at the evaluation of sense of presence (SoP) in high fidelity. Our study aimed to expand on these results by evaluating SoP in different simulation modalities.
A cross-sectional observational quantitative approach was adopted. We distributed a questionnaire assessing the SoP, personality traits and self-efficacy after simulation sessions of various modalities to students and postgraduate nurses, doctors and midwives.
In our study population of 252 participants (56 nurses, 59 doctors and 137 students), SoP did not differ significantly according to the simulation modalities or simulation experiences. The SoP is positively correlated with a sense of self-efficacy and professional experiences. Personality significantly influences the variation in SoP.
Our work highlights the crucial role of SoP in simulation, regardless of its modality. SoP, particularly emotional presence, should be given greater consideration in research, extending beyond just virtual reality applications.
What this study adds:
A better understanding of the sense of presence in other simulation modalities.
Importance of experiences to enhance interactions with simulated environments.
Requires exploration of other parameters such as narrative or emotional transport.
Realism is increasingly recognized as a cornerstone of effective simulation-based medical education, directly influencing how well learners gain knowledge and skills [1–4]. However, despite its acknowledged importance, the field lacks a universally accepted, validated tool to measure realism comprehensively across diverse simulation modalities. Current tools, often limited to virtual reality (VR) settings, fail to capture the complexity of other simulation methods, such as high-fidelity simulations (HFS), low-fidelity simulations (LFS) and role-playing exercises (RP). This limitation hinders our understanding of how the sense of presence (SoP) – a measure of realism – varies across contexts, leaving significant gaps in both research and practice. Addressing this gap is critical for designing educational interventions that enhance learner engagement and outcomes. We seek to broaden the scope of existing SoP measurement tools to ensure their relevance across diverse simulation methods and to explore how internal factors influence SoP.
While realism refers to learners’ perceptions of how real a simulation feels, fidelity describes how closely the simulation replicates actual conditions. The SoP acts as a measure of realism, reflecting how immersed learners feel in the simulation experience. The guidelines of INACSL emphasize that different types of fidelity – physical, conceptual and psychological – are necessary to achieve the desired level of realism in simulation [5]. Physical fidelity refers to how closely a simulation replicates the real-world environment in which the scenario would naturally take place. This encompasses elements like the patient or standardized patient, the simulator or manikin, the environment, equipment, embedded actors and supporting props. Conceptual fidelity ensures that all aspects of a scenario are logically connected and realistic, allowing participants to engage with a coherent and credible case (e.g. vital signs align with the diagnosis). Psychological fidelity enhances the simulation by replicating contextual elements of clinical settings, such as realistic patient interactions, ambient noise, lighting, distractions, family presence, team dynamics, time constraints and competing priorities [6].
Previous research has highlighted the challenge of lacking a universally accepted and validated tool to measure the complex concept of ‘realism’ in simulation [1,7].
Previous studies have investigated the factors that influence this SoP to better understand how to enhance it in simulations [8–10]. These studies indicate that individual characteristics such as personality, level of experience, occupation and gender play a role in shaping SoP in VR settings. Alongside internal factors like cognitive processing, external elements, including sensory input quality and interactivity level, also contribute to variations in SoP [11]. However, these relationships have primarily been examined in VR environments, which limits our understanding of how these factors might affect SoP in other simulation modalities. Expanding this research to include a wider range of simulation methods is essential to fully grasp the dynamics of SoP across different contexts. However, to expand this research, a reliable tool to measure SoP across various simulation contexts is necessary.
While there are existing tools to measure SoP, they are often applied within a limited scope, such as VR simulations. This narrow focus makes it difficult to evaluate and compare realism across different simulation scenarios and methods. To address this, Brackney et al. proposed using a validated questionnaire from VR research to assess realism in HFS [1]. Their study offered valuable insights, showing that the questionnaire effectively captured physical fidelity, but further research is needed to explore its conceptual and psychological aspects. Building on these findings, there is a clear need to expand the investigation beyond the usual context of VR and HFS. Simulation-based learning includes many modalities, such as HFS, LFS and RP. Each has its own benefits and challenges, and understanding how the SoP varies across these different methods is key to improving instructional design and learning outcomes. Therefore, this study aims to evaluate how the SoP can be measured and compared across various simulation methods, broadening the scope of existing tools to ensure their relevance in diverse simulation contexts. The secondary goal of this study was to explore how other internal factors, such as occupation, personality, professional experience and self-efficacy, affect the SoP.
Our hypothesis was that the SoP would be similar across different simulation methods [12,13]. However, secondary hypotheses were that the SoP may vary depending on factors like personality [14], occupation [8], professional experience [9], interdisciplinarity and previous simulation experiences. Additionally, a higher SoP is expected to be linked to a higher self-efficacy score [15,16].
We reported the data following the STROBE checklist for cross-sectional studies.
We conducted a quantitative cross-sectional observational study to answer the research question: How does the Sense of Presence (SoP) change based on the type of simulation used?
The study took place in two simulation centres in the province of Liege in Belgium. The first centre is the medical simulation centre of the University of Liège (ULiège), and the second is the simulation centre of the Haute Ecole Libre Mosane (HELMo). The ULiège Centre has five simulation rooms designed for teaching clinical, technical and non-technical skills to medical students and healthcare professionals. These simulations can be conducted with or without high-fidelity mannequins, incorporating VR, standardized patients and role-play. The centre offers a total of 487 courses, led by various instructors trained in simulation. In the past year 2023–2024, approximately 2,044 students participated in simulations at this centre. The HELMo Centre features three simulation rooms, also dedicated to teaching clinical, technical and non-technical skills to paramedical students and healthcare professionals. Like ULiège, the simulations can utilize high-fidelity mannequins, 360° videos, VR and standardized patients or role-play. The team consists of 14 instructors, all trained in simulation. Annually, about 1,000 students undergo simulation training at this centre.
Data were collected from January to March 2024. Prior to the data collection, the staff from the two simulation centres were informed and coached. The standard duration of the simulation sessions was one and a half hours. At the end of the simulation session, the principal investigator collected the data using a questionnaire in paper or electronic format. The principal investigator’s presence at all sessions ensured standardized data collection and adherence to the study protocol through non-interfering oversight.
The sample consisted of three groups: (1) Students (medicine, nurses who did not yet have professional experience, nurses during baccalaureate or specialised training, and midwives) who came from both the ULiège (University) and the HELMo (Nurse school); (2) Postgraduate doctors; (3) Postgraduate nurses. The inclusion criteria were to be enrolled in a training session at the simulation centre of the University of Liège or High School and to have actively participated in the simulation. Participants were excluded if they only observed the simulation or refused to participate in the study. Each participant was involved in only one type of simulation, with no data collection from the same individual more than once.
To achieve our aim, we collected and analysed various variables. The main parameter studied was the SoP, measured using a French-language questionnaire adapted from a tool initially designed for VR simulations. This questionnaire included 24 items into seven subscales: realism, possibility of action, quality of the interface, possibility of examination, self-evaluation of performance, auditive and haptic [17,18]. The analysis does not include the ‘haptic’ and ‘auditory’ subscales, as these items are specific to VR environments or simulations that involve sound or object interaction. The objective was to develop a questionnaire that is as inclusive as possible, making it applicable across all simulation modalities. We reformulated each item to make it relevant to different simulation modalities, and a panel of 15 reviewers from different backgrounds provided general comments to ensure that each item was properly understood by all the participants in the study. The finalized questionnaire received approval from the researchers of this study and used a 7-point Likert scale for responses (1 – Not at all to 7 – Completely), with some items reversed. Responses were analysed following the guidelines from the original study [18].
We collected socio-demographic data, including age, gender, occupation, seniority and simulation experience. For the purposes of this study, Master’s degree nursing students without prior experience were categorised as students, while others were considered experienced nurses. Internships and student work experience were not counted as professional experience. The type of simulation was classified into four categories based on the dictionary of health simulations [19]: LFS (simple, non-interactive mannequins, e.g. cardiopulmonary resuscitation), HFS (interactive high-fidelity mannequins, e.g. managing an emergency such as anaphylactic shock), procedural (learning specific procedures, e.g. catheter placement or intubation) and RPG (simulated or standardized patients, e.g. breaking bad news or patient education). The simulation theme captured the technical (cardiopulmonary resuscitation or ultrasound) or non-technical (difficult communication or conflict management) objectives of the session, including interdisciplinary aspects. Personality traits were assessed using the Ten-Item Personality Inventory, based on the Big Five personality model, validated in French [20]. Each of the five traits was represented by two items, scored on a scale of 1 (strongly disagree) to 7 (strongly agree), allowing for a balanced assessment. Finally, participants rated their self-efficacy on a 10-point Likert scale (0 = incapable, 10 = fully capable), indicating their confidence in applying concepts learned during the simulation to their current or future professional practice.
A potential bias lies in the lack of exploration of SoP in VR environments, primarily due to the absence of VR simulation sessions at the study sites, which precludes comparison with this modality.
The study’s exploratory nature and the lack of pre-existing data on SoP in non-VR simulation contexts precluded the possibility of performing a sample size calculation. The study included 252 participants, representing all eligible students and professionals present during the study period. This sample size, combined with validated psychometric tools and the inclusion of diverse simulation modalities and participant subgroups, enabled robust inferential statistical analyses. The sample was sufficient to identify trends and generate hypotheses for future research in this underexplored area.
Statistical analyses were conducted using R and Minitab software. Descriptive statistics were employed to characterize the sample, and normality tests were performed to assess data distribution. An ANOVA test was used to evaluate the hypothesis that the SoP is consistent across different simulation modalities while varying according to participants’ personality, occupation, and simulation experience. A correlation analysis was also conducted to investigate the hypothesis that a high SoP correlates with a higher self-efficacy score. A multivariate model was developed to account for potential confounding factors, including age, gender, occupation, simulation experience, work experience, type of simulation, interdisciplinarity and personality traits. Results with a p-value greater than 0.05 were deemed significant. The analysis included 260 questionnaires, excluding 8 with missing data. Psychometric properties were verified, revealing a Cronbach’s alpha of 0.82 for the SoP questionnaire used in this study. The original questionnaire achieved an alpha of 0.84, indicating that internal consistency is maintained after item reformulation.
This study was approved by the ethical committee of Liege University’s Medicine Faculty (reference number: 2023/386). Participation in this study was voluntary and anonymous. Each participant completed and signed a written consent form for approval.
The total sample size for the study consisted of 252 participants, including 59 doctors, 56 nurses, and 137 students from medicine, nursing and midwifery programmes. All students who participated in the simulation agreed to take part in the study. The simulation sessions included 97 simulations with simulated patients (39%), 33 LFS (13%), 84 HFS (33%), and 38 procedural simulations (15%). Table 1 summarizes the socio-demographic and experiential characteristics of the study sample.

| Variable | Doctors, n = 59 | Nurses, n = 56 | Students, n = 137 | Total, n = 252 |
|---|---|---|---|---|
| Gender n (%) | ||||
| Male | 24 (9%) | 25 (10%) | 27 (11 %) | 76 (30%) |
| Female | 35 (14%) | 31 (12%) | 110 (44%) | 176 (70%) |
| Age (years) IQR | 28 (26–30) | 31.5 (25.75–36) | 22 (21–23) | 24 (22–30) |
| Pro. Exp IQR | 4 (2–6) | 7 (2–9) | 0 | 4 (2–5) |
| Simu. Exp. n (%) | ||||
| 0 | 1 (0.4%) | 1 (0.4%) | 1 (0.4%) | 3 (1.2%) |
| 1–5 | 13 (5.2%) | 18 (7.1%) | 103 (40.9%) | 136 (53.2%) |
| 6–10 | 29 (11.5%) | 8 (3.2%) | 29 (11.5%) | 64 (26.2%) |
| >10 | 16 (6.4%) | 29 (11.5%) | 4 (1.6%) | 49 (19.5%) |
| Type of simulation n (%) | ||||
| LFS | 17 (51.5%) | 11 (33.3%) | 5 (15.2%) | 33 (13.1%) |
| HFS | 30 (11.9%) | 12 (4.8%) | 42 (16.7%) | 84 (33.3%) |
| RPG | 12 (4.8%) | 27 (10.7%) | 58 (23%) | 97 (38.5%) |
| Procedural | 0 (0%) | 6 (2.4%) | 32 (54.4%) | 38 (15.1%) |
Pro. Exp. = professional experience in years; Simu. Exp. = previous simulation experience (number); IQR (P25–P75) = interquartile range.
HFS, high-fidelity simulation; LFS, low-fidelity simulation; RPG, role-playing game.
No significant difference was found based on the simulation modalities (p = 0.55). However, the ‘realism’ subscale showed a significantly smaller LFS difference than the other modalities (p = 0.04). Figure 1 compares the SoP and its subscales across the different simulation modalities. All subscales of the questionnaire are positively correlated with the SoP (p < 0.0001), except for the subscale ‘quality of the interface’.

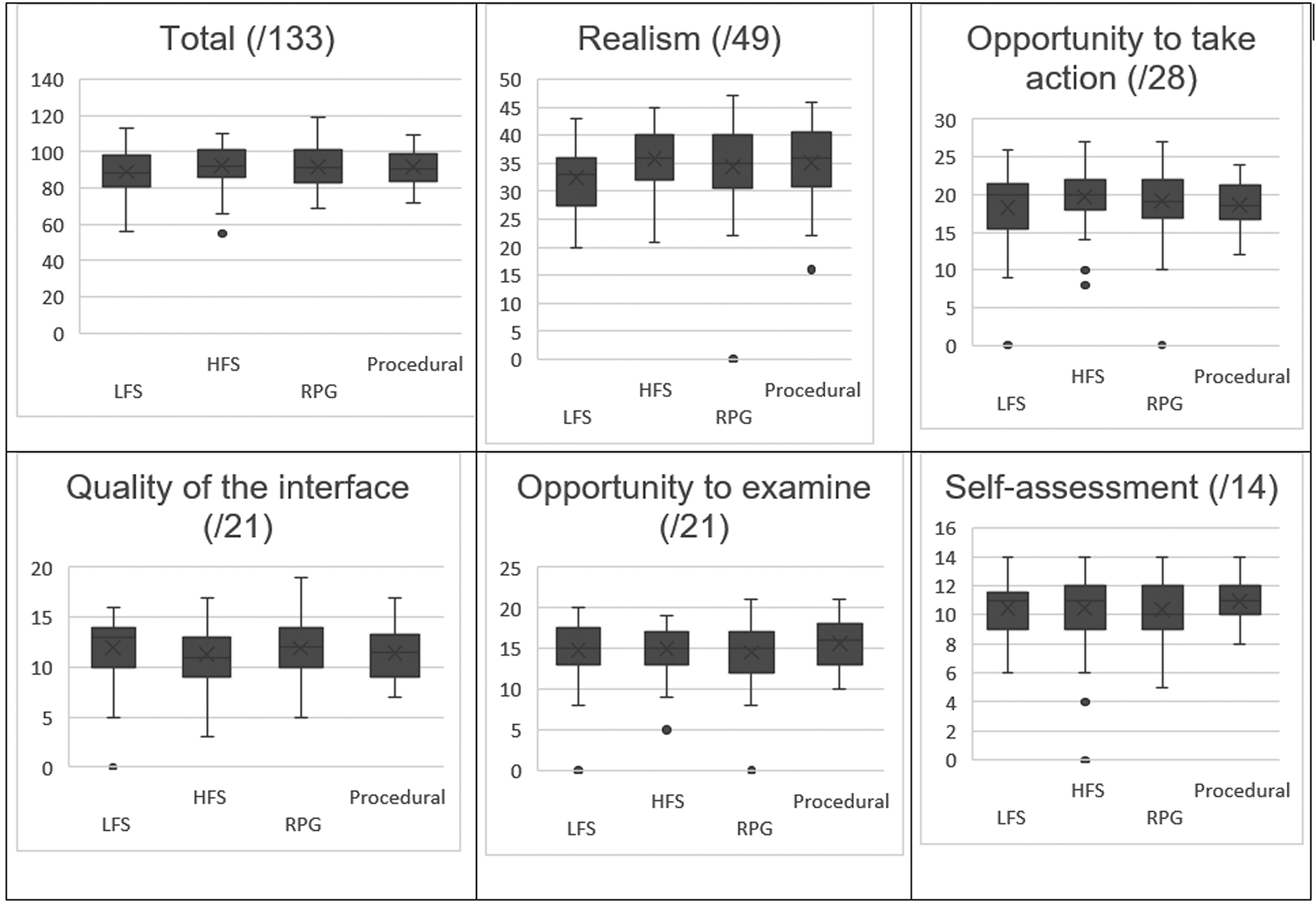
Comparison of SoP and its subscales across the different simulation modalities. LFS: low-fidelity simulation; HFS: high-fidelity simulation; RPG: role-playing game; (/Y): maximal score for each item of SoP scale or total score of SoP scale. Line in the box: mean. Lines of the box: confidence interval.: non-standard values. In our study, the sense of presence scale (score out of 133) was divided into five subscales: realism (score out of 49), opportunity to take action (score out of 28), quality of the interface (score out of 21), opportunity to examine (score out of 21) and self-assessment (score out of 14). The total scores for the SoP and each of the subscales are shown in the figure for each of the simulation modalities studied. There was no significant difference in the total SoP score according to the simulation modality (p = 0.55). There was no significant difference for the scores of the subscales: opportunity to take action (p = 0.25), quality of the interface (p = 0.35), opportunity to examine (p = 0.26) and self-assessment (p = 0.37) according to the simulation modalities. Only the realism subscale showed a significantly lower difference in SBF compared with the others (p = 0.04).
The findings reveal that the SoP (p = 0.007) is significantly lower among students compared to nurses (Table 2). The SoP also does not change based on previous simulation experience (p = 0.25). Furthermore, a higher SoP is associated with an increased sense of self-efficacy (p < 0.0001). Work experience also has a significant effect on the SoP (p = 0.014). The results indicate that the interdisciplinary nature of the simulation does not significantly affect the SoP (p = 0.09).

| Variables | SoP (Mean ± SD) | p-value | |
|---|---|---|---|
| Interdisciplinarity | 0.09 | ||
| No | 91 ± 11.68 | ||
| Yes | 94.08 ± 9.93 | ||
| Gender | 0.8 | ||
| Male | 91.85 ± 10 | ||
| Female | 91.55 ± 11.9 | ||
| Profession | 0.007 | ||
| Student | 89.69 ± 11.56 | ||
| Nurse | 94.94 ± 10.61 | ||
| Doctor | 93.31 ± 10.85 | ||
| Simulation experience | 0.25 | ||
| 1–5 | 90.73 ± 1.5 | ||
| 6–10 | 91.86 ± 12.39 | ||
| >10 | 92.11 ± 11.24 | ||
| Variable | r | r2 | p-value |
| Age | 0.1 | 0.01 | 0.12 |
| Professional experience | 0.06 | 0.018 | 0.014 |
| Sense of self-efficacy | 0.38 | 0.15 | <0.0001 |
Lastly, while all personality traits are linked to the SoP (Table 3), individuals with an ‘openness’ personality trait tend to report a higher SoP than those with other personality traits.

| Personality trait | r | 95% CI | p-value |
|---|---|---|---|
| Extroverted | 0.14 | 0.0–0.26 | 0.03 |
| Sympathetic | 0.13 | 0.01–0.2 | 0.04 |
| Conscientious | 0.14 | 0.01–0.26 | 0.03 |
| Emotionally stable | 0.15 | 0.03–0.27 | 0.02 |
| Open | 0.25 | 0.12–0.36 | <0.0001 |
The multivariate model results, detailed in Table 4, indicate that the variables studied explain 9.5% of the variability in SoP (p = 0.0014). Notably, nurses demonstrate a significant increase in SoP (coeff = 5.32, p = 0.03) compared to students, while doctors also show a positive but not statistically significant trend (coeff = 4.14, p = 0.07). Personality traits such as ‘extroverted’ (coeff = 0.48, p = 0.04) and ‘sympathetic’ (coeff = 0.71, p = 0.04) positively influence ‘SoP’. Age, gender, professional experience, simulation experience and interdisciplinarity do not significantly impact ‘SoP’.

| Variable | Coeff | SD | p-value |
|---|---|---|---|
| Age | −0.18 | 0.2 | 0.35 |
| Gender (male) | 0.3 | 1.78 | 0.87 |
| Profession | |||
| Student | - | - | - |
| Nurse | 5.32 | 2.43 | 0.03 |
| Doctor | 4.14 | 2.28 | 0.07 |
| Pro. Exp. | 0.21 | 0.24 | 0.38 |
| Simu. Exp. | |||
| 0 | - | - | - |
| 1–5 | −7.02 | 11.70 | 0.65 |
| 6–10 | −1.82 | 1.8 | 0.64 |
| >10 | −1.55 | 1.72 | 0.54 |
| Simulation | |||
| LFS | - | - | - |
| HFS | 5.01 | 2.61 | 0.06 |
| RPG | 4.72 | 2.69 | 0.08 |
| Procedural | 5.98 | 3.18 | 0.06 |
| Interdisciplinarity (yes) | 2.92 | 2.29 | 0.20 |
| Conscientious | 0.37 | 0.38 | 0.32 |
| Emotionally stable | −0.05 | 0.32 | 0.87 |
| Extroverted | 0.48 | 0.24 | 0.04 |
| Open | 0.44 | 0.31 | 0.16 |
| Sympathetic | 0.71 | 0.35 | 0.04 |
Adjusted R²: 9.5%. p: 0.0014.
HFS, high-fidelity simulation; LFS, low-fidelity simulation; Pro Exp.: professional experience in years; RPG, role-playing game; SD, standard deviation; Simu. Exp.: simulation experience (number of simulations already experienced).
The present study aimed to explore the SoP in simulation modalities beyond VR. Our internal factors analysis provided insights into questions that remain in the literature. We identified several key points that require further discussion.
This study confirmed our main hypothesis that the SoP remains constant across different simulation modalities. We found that the SoP scores were similar in all four modalities examined. This consistency highlights the significance of feeling present during each simulation, regardless of the technology used. It also suggests that the effectiveness of various modalities regarding learning outcomes may be comparable, as a positive relationship exists between these two factors [12,15].
Brackney and Priode adapted the SoP questionnaire to measure fidelity in HFS [1]. Their study demonstrated that the SoP questionnaire could effectively assess physical fidelity, reinforcing the idea that the SoP is a valuable metric in simulation training. The findings of our study align with their conclusions, suggesting that adapting the SoP questionnaire can provide a robust framework for evaluating fidelity across different simulation modalities [1]. This approach not only supports the assessment of presence but also enhances our understanding of how realism influences learning outcomes. By establishing a valid measurement tool, we can further explore the relationship between ‘SoP’, realism and educational effectiveness in simulation-based training.
Another hypothesis suggested that the SoP would vary depending on the learner’s occupation [8]. This was partially supported by our findings. The SoP was similar for nurses and doctors but significantly lower for students. We also found a statistical correlation between work experience and SoP. This aligns with the study by Servotte et al., which reported lower SoP in undergraduate students compared to postgraduates [9]. These results imply that previous clinical experience helps learners engage better in the VR environment, thus improving their SoP [21]. Accumulated experiences seem to enhance interactions with simulated environments, making simulations more effective and immersive. In a related study, Brackney and Priode hypothesized that experienced students might see simulations as less realistic than those without experience [1]. However, their results showed that both experienced and inexperienced students scored similarly on realism [1]. Realism can be influenced by three types of fidelity: psychological, conceptual and physical. While physical fidelity’s impact on realism is relatively straightforward to measure, psychological fidelity is more challenging to assess. Previous positive experiences can enhance psychological fidelity, potentially reducing unrealistic elements in the simulation. The variability in the relationship between experience and fidelity may be influenced by the measurement tools used. For example, Brackney and Priode’s scale is effective at measuring physical fidelity but may lack sensitivity to psychological and conceptual fidelity. Our scale, however, may be better suited to evaluate these other dimensions of fidelity.
Our results do not confirm the hypothesis that the SoP fluctuates based on individual personality traits. All traits show positive correlations, indicating no strong link between personality and SoP. This suggests the need to explore other factors like emotional involvement [22–25], motivation, commitment [25], cognitive load, pleasure [12] or narrative techniques [23,26,27]. For example, research into the development of empathy emphasises that it is not personality but emotional transport that can significantly improve this skill of empathy [23]. This raises questions about how we can promote emotional transport in simulations to support skill acquisition. Additionally, the role of narrative in conceptual fidelity remains underexplored; targeted narrative feedback has been shown to improve learning outcomes in surgical trainees [27]. Overall, these factors of emotional transport and narrative feedback may significantly influence the experience of presence, indicating a need for a holistic approach to understand the underlying mechanisms better.
Further studies are needed to explore the psychological impacts and interactions between prior experiences and SoP. This observation highlights this teaching method’s importance, allowing students to practice in simulations before their first patient contact. However, we must consider how to engage and foster an SoP among students who lack professional experience in these environments. While the necessity of training is well established, it is crucial to improve basic training quality to help reduce hospital mortality rates [28,29]. In that sense, when implementing simulations for first contacts, the primary aim should be to ensure safety and help students become familiar with the clinical environment. Early simulations should not place undue demands on students, as they may not possess the prior psychological fidelity necessary for more ambitious learning goals. Instead, these sessions should serve to demystify the clinical setting, providing a supportive foundation for future learning. As students gain clinical experience, we can then introduce more challenging objectives that build on their growing competence and confidence.
Only one type of questionnaire was used to examine SoP, potentially biasing the results, as no validated questionnaire exists for SoP beyond VR.
This study enhances our understanding of the SoP by looking beyond traditional simulation methods like VR. We found that SoP remains consistent, regardless of technical sophistication, indicating a need to prioritize conceptual and emotional fidelity over technical features. Further exploration of the interdisciplinary aspect could reveal how collaboration impacts learning outcomes and self-efficacy. Understanding these factors can help us optimize simulation-based education, tailoring it to maximize its educational impact and better prepare students for professional practice
None declared.
This research did not receive any specific grants from funding agencies in the public, commercial or not-for-profit sectors.
None declared.
None declared.
The authors declare no conflict of interest.
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.