
We aimed to detect different types of latent safety threats (LSTs) by using on-site simulations for pregnant women with suspected COVID-19 presenting to the Birthing Unit. We recorded LSTs during on-site simulations. There were three scenarios, which involved the presentation of a suspected patient to the Birthing Unit, donning and doffing, and transportation to the operating room. LSTs were subcategorized into Gaps in Knowledge and Training, Maintenance and Equipment, and System and Processes. Sixty-five participants were involved. Eighty-one LSTs were observed: scenario 1 (n = 42, 51.8%), scenario 2 (n = 14, 17.2%) and scenario 3 (n = 25, 30.9%). Amongst the different themes, Gaps in Training and Knowledge comprised (n = 29, 35.8%), Maintenance and Equipment comprised (n = 46, 56.8%), and Systems and Processes comprised (n = 6, 7.4%). Pre-simulation surveys revealed only 10% of participants felt very prepared to care for these patients, while 92% responded the same way post-simulation.
What this essay adds:
On-site simulation-based exercises can greatly help Birthing Units prepare and care for patients with suspected or confirmed COVID-19. Lessons learnt from exercises are still highly relevant in the post-COVID era.
Latent safety threats uncovered in on-site simulation can reveal specific areas for improvement. Maintenance and equipment issues were the most frequent latent safety threats observed. The scenario with the most latent safety threats was the presentation of suspected or positive COVID-19 patients to obstetric triage. Simulation training should be focused on these areas.
Post-simulation surveys demonstrate significant improvement in preparedness among participants and should be used following these simulations to determine the utility and need for additional training/educational purposes.
Novel coronavirus (SARS-COV-2) is a strain of coronavirus leading to COVID-19 [1]. The current COVID-19 pandemic presented challenges to the medical community on a scale not previously seen [2]. Research has shown that pregnant women do not appear more likely to contract the infection than the general population; however, pregnancy in itself alters the body’s immune system and its response to viral infections, which in general, can cause more severe symptoms [1]. The Centers for Disease Control and Prevention has classified pregnant patients as a group that may be at increased risk [2].
Once maternal infection of COVID-19 is suspected or confirmed, childbirth becomes complicated and poses challenges for numerous reasons [3]. Efficient obstetric management is key in reducing complications for both mother and infant. Special care should be taken in determining the timing of delivery, assessment of the indications for caesarean section, choice of anaesthesia, newborn management and preparedness of the delivery room to prevent the spread of infection, and to protect healthcare workers [3]. Patients presenting in labour or with complications of the disease may require delivery, which presents additional logistical and infection control issues [1].
As simulation-based education (SBE) has become more commonplace in the healthcare system, we believe it can greatly help units prepare and improve readiness [4]. The goal of most SBE activities in health care is to train providers in the proper assessment and management of clinical problems [4]. An important role as well is to practise the psychomotor skills required in the actual situation, through deliberate practice, reflection and debriefing [4]. When simulation-based activities take place in the actual clinical setting, they have the added benefit of providing physical and contextual reality. This may provide an important occasion to assess and address system and process-related issues, otherwise known as latent safety threats (LSTs). LSTs are defined as threats to patient safety or quality care resulting from Gaps in Training and Knowledge, challenges with Maintenance and Equipment and, finally, Processes and System breakdowns, which may contribute to medical errors and have a significant impact on patient safety [4].
The objectives of recording LSTs during these on-site simulates were two-fold. The first objective was to detect the different types of LSTs in the setting of suspected or positive COVID-19 pregnant patients in the Birthing Unit using a training programme involving three on-site simulations. The second objective was to determine whether on-site simulation improved participant’s preparedness to care for suspected or confirmed cases of COVID-19 patients presenting to the Birthing Unit including donning and doffing appropriate personal protective equipment (PPE).
We recorded LSTs between 15 April and 6 May 2020 at secondary-care-level hospital in Canada.
Our Birthing Unit COVID-19 Pandemic Response Protocol was developed at the end of March 2020. The foundation for our protocol was based on The Ottawa Hospital Policy on Aerosol Generating Respiratory Procedures [5–7], which was designed to help healthcare workers determine the adequate PPE required based on location or procedure in-hospital and COVID-19 patient risk factors.
We involved interprofessional healthcare workers (e.g. obstetricians, residents, nurses, midwives) who were current staff in the Birthing Unit. Small groups of 5–10 healthcare workers were assembled in designated areas of the Birthing Unit. These were also the areas pre-dedicated areas for potential or suspected COVID-19 cases. Simulations were run in the mornings and afternoons spanning over 3 hours.
We decided on three training scenarios given time restrictions which involved presentation of a suspected COVID-19 patient to the Birthing Unit, donning and doffing with observer, and lastly, transportation of a suspected COVID-19 patient to the operating room for non-urgent caesarean section. The mode of delivery of suspected or confirmed COVID-19 patients in the Birthing Unit was based solely on obstetric indication as per our protocol. These scenarios were based on ACOG’s COVID-19 Obstetric Preparedness Manual [2]. Facilitators guided simulation participants during the scenarios by providing a stem detailing the scenario and answering questions regarding areas of confusion. The simulation facilitators also recorded LSTs throughout the sessions. Debriefing and time for questions were provided after each scenario. After each session, we discussed changes needed to our Birthing Unit pandemic protocol.
Once simulations were completed, we counted the number of safety threats observed in each scenario and further subcategorized them into the following themes: Gaps in Knowledge and Training, Maintenance and Equipment, and System and Processes.
Post-simulation surveys were provided once all participants had completed on-site simulations. Surveys were emailed to participants and included questions regarding preparedness before and after having participated in simulations. Additionally, we asked participants about their preparedness regarding donning and doffing droplet and airborne precautions. The results were collected anonymously and reviewed. Please see Supplementary Appendix 1 for the complete survey.
Our training involved a total of 65 participants involved in on-site simulations in the Birthing Unit. Eight runs of the simulation were completed and all runs included the three scenarios. A total of 81 LSTs were observed. In scenario 1 (presentation of a suspected COVID-19 patient to the Birthing Unit), we observed 42 LSTs. This corresponded to 51.8% of all LSTs observed by the scenario. In scenario 2, 14 LSTs were recorded, comprising 17.2% of all LSTs by scenario. Finally, in scenario 3, we observed 25 LSTs, corresponding to 30.9% of all LSTs. Refer to Table 1 for the breakdown of LST by scenario.

| Theme | Number of LST |
|---|---|
| Scenario 1 | n = 42 (51.8%) |
| Scenario 2 | n = 14 (17.2%) |
| Scenario 3 | n = 25 (30.9%) |
| Total latent safety threats | n = 81 (100.0%) |
When analysing LSTs by theme, Gaps in Training and Knowledge comprised 29 and therefore 35.8% of LSTs. There were 46 LSTs within the Maintenance and Equipment theme, therefore comprising 56.8% of LSTs. Finally, we noted six LSTs within the theme of Systems and Processes, comprising 7.4% of LSTs. Table 2 organizes the LSTs by theme. Table 3 further subcategorizes the LSTs by theme and scenario.

| Theme | Number of LST |
|---|---|
| Gaps in Training and Knowledge | n = 29 (35.8%) |
| Maintenance and Equipment | n = 46 (56.8%) |
| Systems and Processes | n = 6 (7.4%) |
| Total latent safety threats | n = 81 (100.0%) |

| Theme | Number of LST | |
|---|---|---|
| Scenario 1 | Gaps in Training and Knowledge | n = 14 (33.3%) |
| Maintenance and Equipment | n = 24 (57.1%) | |
| Systems and Processes | n = 4 (9.5%) | |
| Total latent safety threats | n = 42 (100.0%) | |
| Scenario 2 | Gaps in Training and Knowledge | n = 5 (35.7%) |
| Maintenance and Equipment | n = 7 (50.0%) | |
| Systems and Processes | n = 2 (14.3%) | |
| Total latent safety threats | n = 14 (100.0%) | |
| Scenario 3 | Gaps in Training and Knowledge | n = 10 (40%) |
| Maintenance and Equipment | n = 15 (60.0%) | |
| Systems and Processes | n = 0 (0.0%) | |
| Total latent safety threats | n = 25 (100.0%) |
As select examples of LSTs recorded within the Gaps and Training in Knowledge theme, we noted that healthcare provider (HCP) did not have a good understanding in general of how COVID-19 affects pregnancy and childbirth – namely symptoms and effects in pregnancy. HCP found it difficult to distinguish between COVID-19 symptoms and normal labour symptoms such as nausea and vomiting, for example. HCPs did not know how to test a patient for COVID-19 nor how to find and complete Public Health Forms. HCPs themselves did not know their N95 mask size. In terms of patient flow, we noted that often HCP forgot to make the team (i.e. Charge nurse) aware of the presence of a suspect or confirmed COVID-19 patient upon presentation. There was difficulty in being able to securely transport a patient from the obstetric triage to the dedicated isolation room in the Birthing Unit while maintaining physical distance. HCPs often would bring paper, pens or charts in isolation rooms that were not authorized to enter the room.
Examples of LSTs recorded within the Maintenance and Equipment theme included difficulty obtaining and localizing PPE in the obstetric triage and missing surgical masks. The glass pane in front of the obstetric triage made it difficult to hear the patient’s answers to screening questions. We also noted within isolation rooms that there were missing plastic covers on the keyboards, as well as glove boxes and hand sanitizer stations were not frequently refilled. Pens were missing from isolation rooms as well. We also noted that there were excessive laundry bins outside of isolation rooms which made it difficult for HCPs to know where donning and doffing should occur. Soiled bins were also found to be overflowing. From a communication perspective, there was a limited supply of portable phones.
When reviewing LSTs within the System and Processes theme, we noted that paper Non-Stress Test strips could pose a contamination risk, there is no dedicated place to document the time of medication administration, especially in an emergency situation such as post-partum haemorrhage. HCP also brought concerns regarding fatigue while staying in the room with the labouring patient with prolonged PPE use. Finally, there were concerns raised by our midwifery colleagues who normally practise solo when assisting a patient in the first stage of labour and therefore would be missing a runner in case there were not enough obstetric nurses available.
Fifty participants completed post-simulation surveys. Pre-simulation, only 10% of participants felt completely prepared to care for these patients, while 92% responded in the same way post-simulation (Figure 1). Pre-simulation, only 24% of participants felt completely prepared to don and doff contact and droplet precautions, while 66% responded in the same way post-simulation (Figure 2). Finally, pre-simulation, only 12% of participants felt completely prepared to don and doff airborne precautions, while 48% responded in the same way post-simulation.

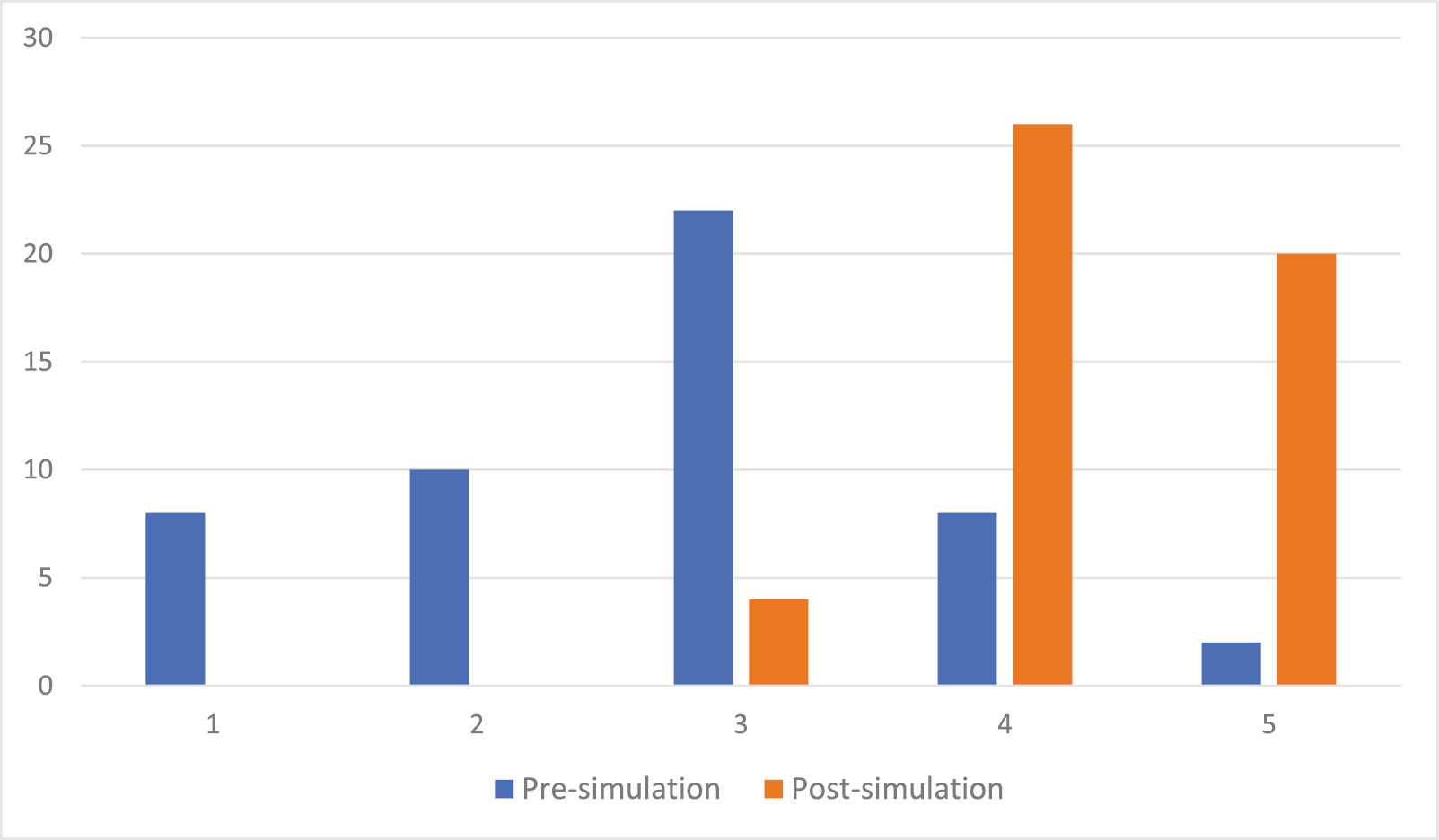
Preparedness to care for a suspected or positive COVID-19 patient in the Birthing Unit (1 – Not at all prepared, 2 – Completely prepared)

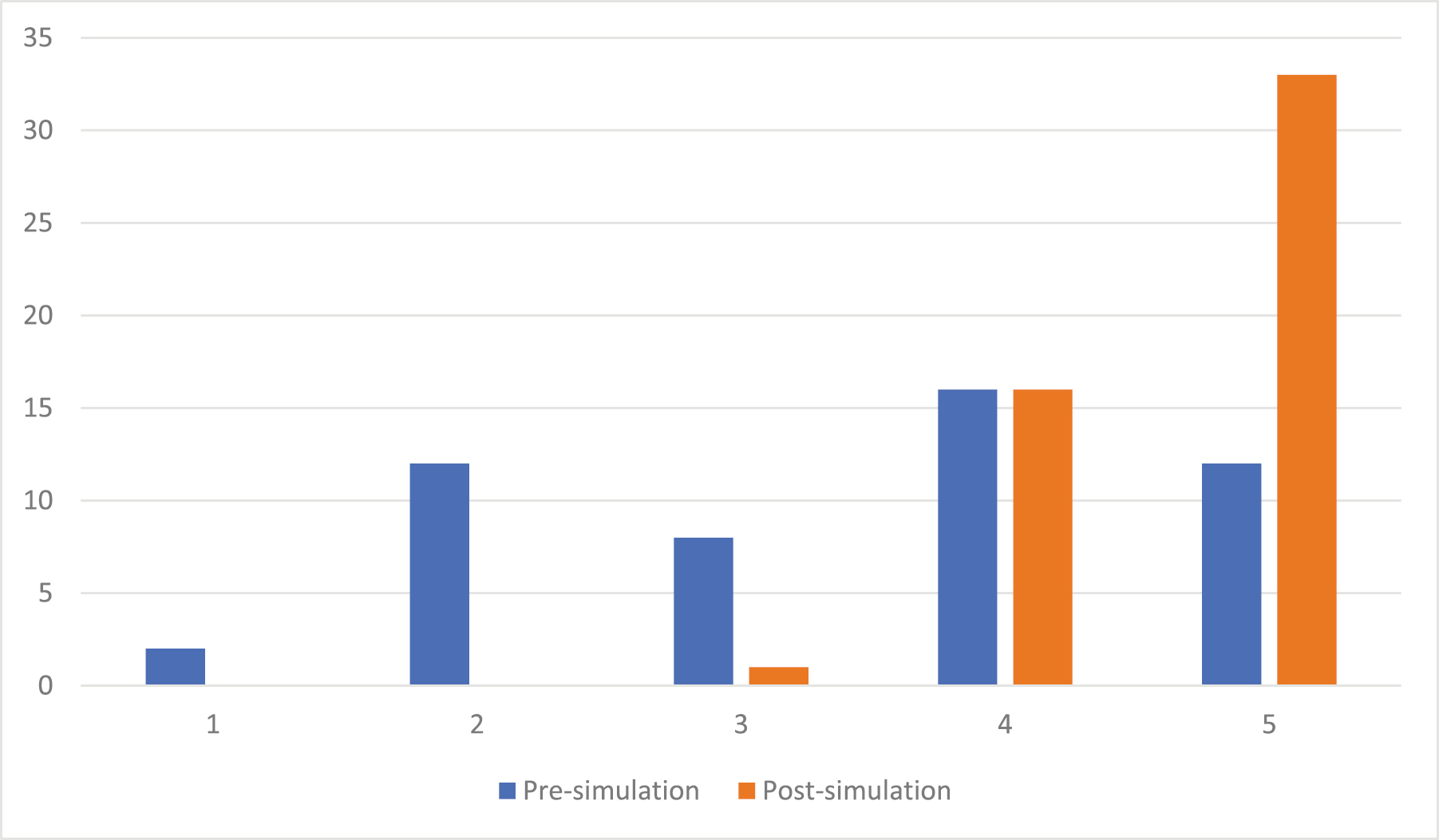
Preparedness to don and doff contact and droplet precautions (1 – Not at all prepared, 2 – Completely prepared)
Recording LSTs during on-site simulations in our Birthing Unit reinforced that on-site simulation-based exercises greatly help units prepare and help identify areas for infection-control protocol improvement and ongoing staff training. Our findings demonstrated that the most frequent simulation scenario that poses LSTs is at the initial presentation of a suspected or confirmed COVID-19 pregnant patient to the Birthing Unit. This may intuitively pose the greatest number of LSTs given that the way the patient is initially triaged sets the stage for subsequent management. Moreover, this was the first scenario presented to participants and therefore allowed them the opportunity to review initial questions or concerns.
We also found that the most frequent LST theme overall was among those concerning Maintenance and Equipment (56.8%). Given that the management of suspected or confirmed COVID-19 patients presenting to the Birthing Unit requires a large amount of PPE and dedicated areas, on-site simulation is very helpful in uncovering hospital areas that are missing equipment needed to manage real-life situations. Staff practising on-site can help us identify if the equipment is placed appropriately and whether the correct supplies are easily available.
One explanation as to why the recorded LSTs for System and Processes were so low (7.4%) could be that by definition on-site simulations are not designed to uncover issues regarding the system breakdowns [4]. The recorded LST within the System and Processes category in our findings were mainly due to midwifery practices in our centre. These were considered System and Process issues as they existed prior to the COVID-19 pandemic. For example, midwifery works as a separate service in our labour and delivery unit, and therefore patients often present to the obstetric triage prior to their midwife’s arrival. Typically, these patients are roomed in triage by the midwife and not the obstetric nurse. We felt that this posed a problem within the System and Process category as this was a recurring issue even outside of the pandemic in our center.
Post-simulation surveys further allowed us to see the benefits specifically in areas of overall preparedness and donning and doffing of both contact, droplet and airborne precautions.
It is important to note that our Birthing Unit COVID-19 Pandemic Response Protocol is in keeping with the objectives and recommendations of other protocols in the literature. The literature highlights key areas of training including correct use of PPE and transportation of patients for urgent caesarean section [8]. Another study further reinforces the importance of a standardized birthing unit protocol and tracking the staff’s attendance in simulation training to ensure adequate training [7]. Other essential steps noted were clearly demarcating donning and doffing areas with sufficient supplies of PPE, as well as ‘Dofficers’ to assist HCPs [8].
In terms of LSTs observed in other COVID-19 Birthing Unit Simulations, a study by Muhsen et al. demonstrated areas of concern to be floor plan adjustments, communication with portable phones and notifying the team of a suspected/confirmed case on the unit, all of which were similar LSTs observed in our study [9].
When examining the impact of cognitive load on participant’s overall performance and contribution to the number of LSTs, we definitely believe this may have played a role. In a study by Tremblay et al., the authors argue that learning complex skills in a complex environment is likely to be overwhelming for novice learners. This is likely due to their lack of experience with both the new task and environment [10]. This directly relates to the complex and new situation presented to our simulation participants as this was just the beginning of the COVID-19 pandemic and our hospital protocols were so new. Moreover, we were constantly adapting our protocols given feedback from simulation sessions.
Reflecting on these sessions as a department, simulations of this calibre have never been done at our community hospital site and demonstrated a number of benefits. There are clear advantages showing that simulation education also demonstrates great potential as a training method and quality improvement initiative. Moreover, the development of this protocol using a multidisciplinary team, including anaesthesia, helped us to refine the protocol from different perspectives. We also noted the great academic and cultural impact in our department namely in terms of preparedness and overall unity of the Birthing Unit team members. We would also like to mention that renumerated nursing staff as part of their ongoing Continuing Medical Education greatly helped in the recruitment process as well as supplemental hours provided by the simulation session facilitators.
Limitations of this training include reproducibility depending on resources, protocols layouts of different healthcare sites and obstetric units. We note that there was also potential in missing LSTs as these were only recorded by two facilitators. Future areas of research would include performing in-situ simulations which would take place in actual clinical settings with teams that are currently on shift, to help uncover more LSTS in relation to System and Processes. We would like to provide post-simulation surveys to better understand the needs of the Labour and Delivery staff at this time now that several years have passed since the pandemic.
In conclusion, pregnant women with suspected or confirmed COVID-19 presenting to Birthing Units pose numerous infection control issues. Simulation-based exercises greatly help units prepare by identifying LSTs. LSTs were mostly uncovered at the moment of presentation of suspected COVID-19 patients to the Birthing Unit. The largest proportion of LSTs involve Maintenance and Equipment issues. Post-simulation surveys further allowed us to see the benefits of this type of training in terms of preparedness and donning and doffing.
None declared.
None declared.
None declared.
None declared.
None declared.
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.