Simulation-based interprofessional (IP) education programs at the undergraduate level remain limited both worldwide [1] and within the Portuguese educational context [2]. The LINKS workshop - Lifting INterprofessional Knowledge through Simulation - is a novel initiative designed for IP teams of healthcare students (medicine and nursing). It aims to enhance team-based behavioural competencies that are essential for effective IP teamwork. This pilot study aims to assess the impact of the LINKS workshop on communication skills within IP undergraduate teams.
This quasi-experimental study involved final-year medical and nursing students participating in a 4-hour, simulation-based IP workshop. Working in mixed teams, students managed two clinical scenarios designed to promote interprofessional communication, each offering equivalent challenges and opportunities to practice key communication strategies. Each scenario was followed by a structured debriefing led by experienced facilitators, focusing on teamwork skills, including key communication strategies. A total of thirteen IP teams participated. The scenarios were video recorded for subsequent analysis of the teams’ performance.
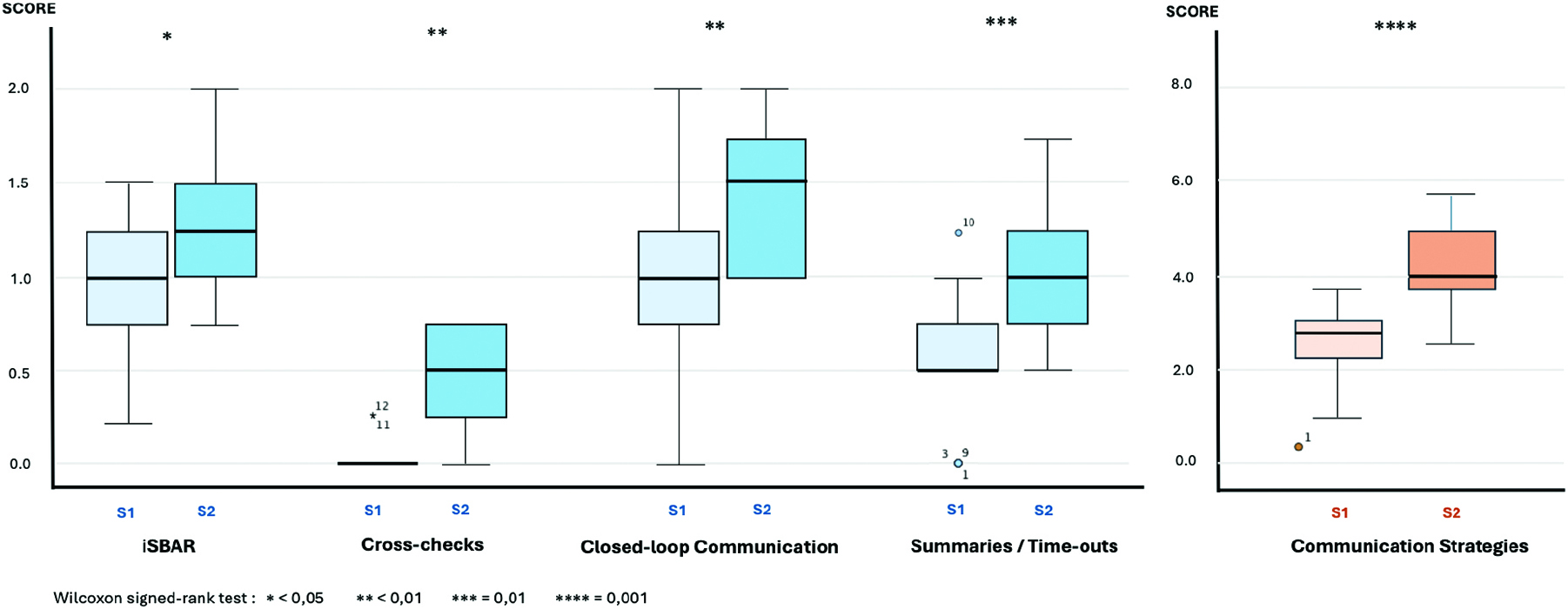
Interprofessional communication was assessed using an observational tool for monitoring non-technical skills [3], focusing on four communication strategies: (1) iSBAR (e.g., identification, situation, background, assessment and request/recommendation); (2) cross-checks; (3) closed-loop communication; and (4) summaries/time-outs. Four independent observers reviewed the recordings and scored team performance on each communication skill, using a 3-points scale: 0 - Not observed; 1 - Observed but inconsistent or incorrect use; 2 - Observed consistently and correctly used.
The Wilcoxon signed-rank test was used to compare performance in both scenarios. Inter-rater reliability was assessed using Cronbach’s alpha. This study was approved by the ethical committee of the Faculty of Medicine of the University of Porto, and written informed consent was obtained from all participants.
Internal consistency of communication strategies scores was acceptable (Cronbach 0.7 ≤ α < 0.8), for both scenarios. Statistically significant improvements were observed in all four communication strategies and in the overall communication score between the two scenarios (p<0.05, Figure 1).
Teams demonstrated improved use of communication strategies in the second scenario, suggesting a positive effect of the IP simulation activity combined with a structured debriefing. This pilot study reinforces the value of simulation-based IP educational at the undergraduate level in clarifying professional roles and enhancing team communication. Continued implementation of such programs within clinical training can foster essential teamwork competencies and drive meaningful curriculum reform, preparing students for effective collaborative practice in healthcare settings.
As the submitting author, I can confirm that all relevant ethical standards of research and dissemination have been met. Additionally, I can confirm that the necessary ethical approval has been obtained, where applicable.
1. Choudhury RI, Salam Mau, Mathur J, et al. How interprofessional education could benefit the future of healthcare – medical students’ perspective. BMC Med Educ. 2020;20:242.
2. Sa-Couto C, Fernandes F, Pinto CC, Loureiro E, Cerqueira C. Impact of a simulation-based interprofessional workshop (LINKS) on Portuguese healthcare students’ perception of roles and competencies: a quasi-experimental pilot study. Int J Healthc Simul. 2024;XX(XX). doi: 10.54531/PRHF1746
3. Rosário L, Sá-Couto CD, Loureiro E. An observational and action-based tool for non-technical skills monitoring in Simulation-Based Training. SESAM 2019 Proceedings.