Microsurgical training is a specialist area of surgical skill with multiple existing simulation models previously proposed to facilitate its acquisition, such as live animal models and bench models. Extended reality-based training methods are a rapidly growing area within surgical education, including microsurgery. However, there is a notable gap in the current literature examining the impact of these novel modalities in comparison to more established models and other educational interventions.
This systematic review aims to examine the following question: what effect do extended reality-based educational interventions have on microsurgical skills training of healthcare professionals and students compared to other educational interventions?
A systematic search of five literature databases will be undertaken using a clearly defined search strategy. Studies utilizing extended reality simulation methods to teach microsurgical skills to healthcare professionals undertaking this form of surgery will be included. Studies considering any quantitative or qualitative educational outcome assessment will be accepted for inclusion. Two authors will independently screen, select, extract and appraise the resultant literature based upon agreed data extraction templates, overseen by a senior author. The systematic approach includes the use of established frameworks and will be reported in accordance with best practice guidelines.
A comprehensive protocol for a systematic review examining the impact of extended reality training modalities compared to existing simulation methods is needed to assess and synthesize the current knowledge status of this field. The subsequent report will be a pivotal step in understanding the role and effectiveness of extended reality-based education within microsurgical training.
With growing pressure placed on both surgical educators and learners due to the restriction of working hours [1], increasing number of undergraduate medical school places [2] and ever-increasing demands within healthcare services globally [3], trainee in vivo operative experience is decreasing [4]. This, combined with an evolution from the traditional apprenticeship model of surgical training towards a more objective, competency-based programme [5], has resulted in a growing emphasis on the role of simulation training for skill acquisition. The rationale for the use of simulation in surgical training is well established due to its positive impact on patient safety [6] in addition to gaining psychomotor skills [7]. The use of simulation training prior to intraoperative skill application results in a reduced rate of intra-operative and postoperative complications as well as a shorter duration of hospital stay [8], whilst trainees completing laparoscopic simulation training demonstrate greater speed, efficiency and security of surgical knot tying [9].
Despite this, surgical trainees in the United Kingdom have reported low levels of access to surgical skills simulation facilities especially outside of working hours or when free of clinical commitments [10]. This is a trend mirrored internationally; half of surveyed European urology trainees reported no current access to simulation facilities [11] and 85% of Canadian surgical residents reported less than monthly access to simulation training opportunities [12]. In addition, equitable access to simulation is not achieved across subspecialties, with UK trainees in plastic surgery, neurosurgery, and oral and maxillofacial surgery reporting lower levels of simulation training availability compared to peers in urology and paediatric surgery [10]. This is likely due to simulation training being a compulsory aspect of the curriculum for some surgical specialities [13]. Where simulation is not a required element, the variable geographic provision of simulation facilities negatively impacts access for trainees, despite many expressing a clear desire to undertake regular simulation training [14]. Subsequently, there is increasing focus on more accessible models of simulation which do not require the use of large and immobile equipment (for example, robotic consoles or operating microscopes) thereby removing additional barriers to learner usage. Tablet-based simulation models, which utilize a tablet in lieu of laparoscopic screens for instance, are well accepted by trainees due to their ease of use and ability to utilize technological equipment which they already own [15]. By allowing trainees to continue to develop surgical skills outside of clinical working hours through self-directed learning, practice occurs in a more distributed way and at each trainee’s own pace; as trainees are not constrained by time pressures, learning can occur in a more outcome-based way [16] improving skill acquisition and consolidation [17].
Microsurgery utilizes high-power magnification to perform intricate surgical procedures such as vessel and nerve repair [18]. Microsurgical training is particularly affected by the high-stress conditions and low margin of error associated with its application, leading to the suggestion that all initial microsurgical skill acquisition should occur within a simulated setting [19]. Similar to other surgical modalities [20], acquired microsurgical skills also experience decay during periods of disuse [21], adding further support to the need for microsurgical simulation training.
The current gold-standard simulation model for microsurgical anastomosis training is live animal models due to their similar physiology to human tissue [18] thus increasing the fidelity of the simulation experience through replication of events such as thrombogenesis, blood flow and inflammatory processes [22]. However, the ethical and financial implications of using live animals, including cost of care and facilities during rearing, intra-procedural anaesthesia and subsequent requirement for terminal euthanasia [23] mean that substitutes are required. Multiple alternative models currently exist, such as chicken thigh models [24], silastic tubing [25] and Japanese noodles [26], with varying strengths in differing aspects of validity (for example, content, construct, predictive) [27, 28]. Increasing accessibility to virtual, augmented and mixed reality technologies means that the use of extended reality simulation is a rapidly increasing subfield of interest.
Key definitions for augmented reality (AR), virtual reality (VR) and mixed reality (MR) are given in Table 1. Extended reality (XR) encompasses these three modalities as a continuum [29].

| Term | Definition | Example use |
|---|---|---|
| Augmented reality | Use of technology to superimpose digital elements onto a view of the real-world environment [30]. | Clinical: Identification of feeding vessels in arteriovenous malformation clipping [31]. Educational: Intra-ocular microsurgical instrument manipulation [32]. |
| Virtual reality | An interactive three-dimensional reality exclusively within a computer simulated environment [30]. | Educational: Dental endodontic resections [33]. |
| Mixed reality | The merger of real and virtual worlds, allowing physical and digital objects to co-exist and interact [34]. | Clinical: Identification of free flap vessel perforators intra-operatively [35]. Educational: Learning curve assessment of intracranial aneurysm clipping [36]. |
Previous literature has considered the role of XR modalities in both clinical contexts and for educational interventions within several fields of microsurgery, including plastic surgery, ophthalmology, neurosurgery and endodontic dentistry (Table 1). A preliminary literature search has identified the existence of narrative reviews assessing the current scope of XR modalities specifically within microsurgical education [37] alongside focused systematic reviews within a single ophthalmological procedure [38]. This initial exploration also highlighted that there is a breadth of robust existing primary research allowing for the evaluation of a variety of training techniques and research methodologies in isolation; however, there appears to be a paucity of any broader comparison of the effectiveness of XR educational methods against other methods of education. Completion of a systematic review with this as its main objective will allow for the identification of all relevant literature within this field, and greater assessment of XR microsurgical simulation training in comparison to other educational interventions across all surgical specialities.
The aim of this systematic review is to undertake a methodical search and appraisal of the existing literature to explore the use of XR in microsurgery training. This is to answer the following question: What effect do extended reality-based educational interventions have on microsurgical skills training of healthcare professionals and students compared to other educational interventions?
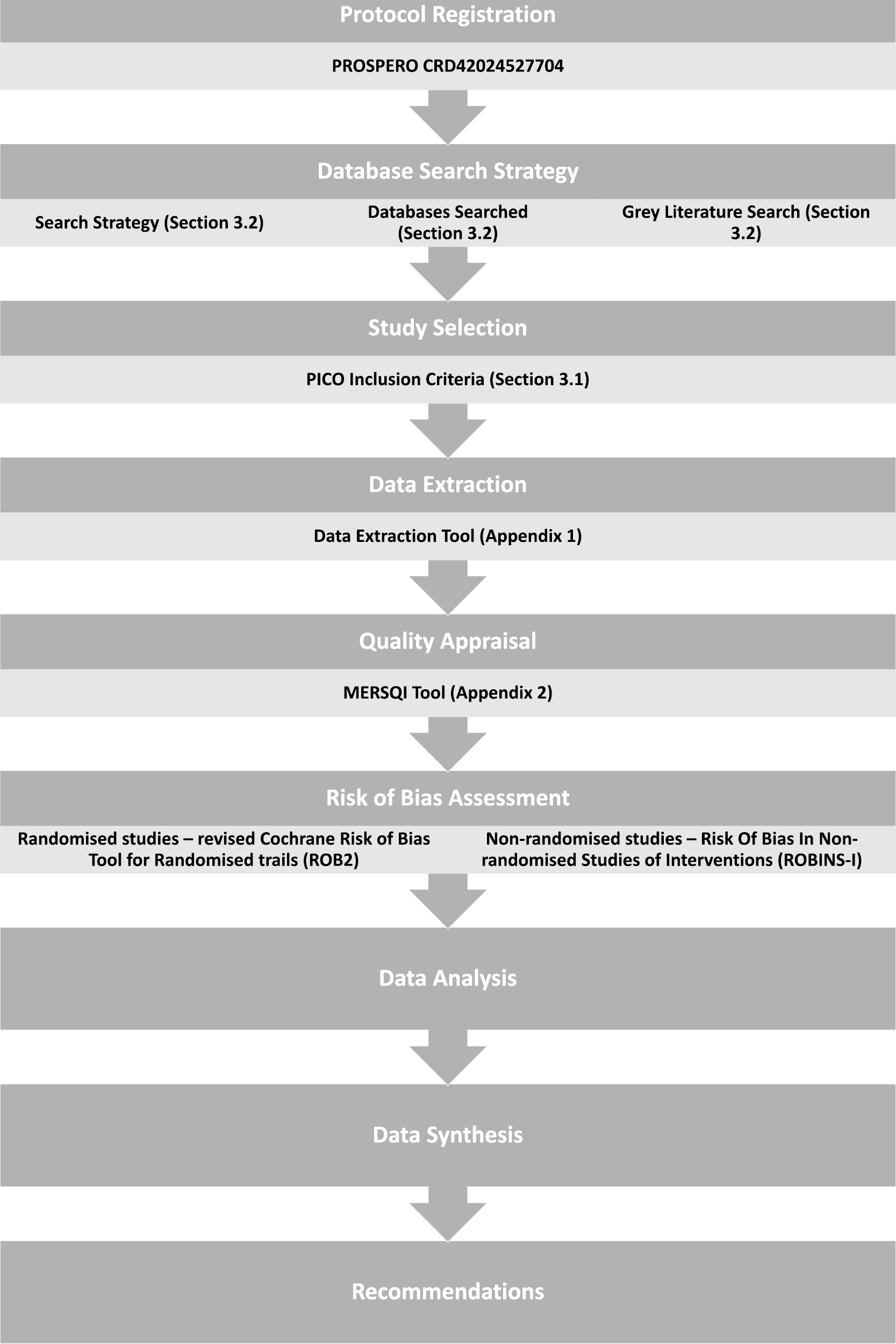
The protocol for this review has been submitted for registration on PROSPERO (registration number CRD42024527704) and has been reported in accordance with PRISMA-P recommendations for Systematic Review Protocols [39]. The proposed methodology is based on the Cochrane Handbook recommendations for conducting a systematic review [40]. This combination of positivist and constructivist approaches not only evaluates the effectiveness of the intervention against other educational interventions but also allows for further exploration of any findings, resulting in a greater understanding of the research question than can be achieved using solely a quantitative or qualitative strategy [41]. An overview of the systematic review process is given in Figure 1.

Systematic review method
The criteria for inclusion within the systematic review is based on the PICO framework as advocated by the Cochrane Handbook recommendations [40]. This structure is widely used in the construct of systematic reviews within the simulation community [42, 43].
Given that the research examining the use of XR methods to train and develop clinical skills is emerging and evolving, a broad search strategy was created to capture the likely diversity of published literature currently in existence [40].
Studies including any medical professional from undergraduate medical student to consultant/attending will be further reviewed for inclusion.
Initial learning curves for microsurgical skill acquisition show rapid improvement before flattening off as greater proficiency is reached [44]. Previous literature has identified that those deemed proficient, most commonly senior trainees and consultant/attending surgeons, demonstrate a clustering of skill rating scores at a high level; however, few surgeons are able to demonstrate perfect expert performances [45]. This suggests that the potential for skill acquisition and refinement continues throughout all surgical grades and may be affected by novel training modalities.
Additionally, studies evaluating learning in allied health professionals (for example, physician associates or surgical care practitioners) will also be considered for inclusion if the individual’s job role means they may be expected to assist with microsurgical techniques. Overlap exists between the skills required of the primary surgeon and assistant during a microsurgical procedure. Assistants can be expected to cut sutures and stabilize anatomic structures [46] so are required to demonstrate proficiency when manipulating surgical instruments under microscopic magnification [47].
In this systematic review, studies utilizing XR interventions (comprising of AR, VR or MR) to teach microsurgical skills will be reviewed. Key definitions for AR, VR and MR are included in Table 1. Microsurgical skills are defined as: part of or whole operative procedure completed under magnification with specialized instruments and equipment [48].
Several microsurgical skills courses currently exist catering for participants from differing surgical specialities [49] as the basic microsurgical skills acquired during simulation such as instrument manipulation and tremor control are applicable across many speciality fields [50]. Therefore, interventions based on any speciality undertaking microsurgical procedures will be considered. Ophthalmology, for example, has established several methods of microsurgical skills education [51], however, undertakes a separate training pathway to other surgical specialities [52].
Only studies where a comparison group exists and has been exposed to an educational intervention will be considered for inclusion. This is because the educational community accepts that any educational intervention is likely to influence participant learning and related outcome measures [53].
Studies utilizing an institution’s previous educational practice as a comparison group will be reviewed for suitability providing this consists of active educational involvement. Several educational models currently exist for microsurgical skills acquisition and training, including bench models, human cadaveric tissue and live animals [18, 54]. The lack of a clear optimum training modality to compare novel models necessitates that all simulation models currently used in current educational practice be considered as a comparison.
Studies will only be considered for inclusion where evidence of an assessment of the educational outcome exists. Manuscripts presenting proof of concept or validity evidence of a novel model without demonstration of learner development will be excluded.
Both objective measures such as error scores and subjective results, for example, confidence ratings will be accepted as outcomes for quantitatively designed studies. Despite attempts of global working groups, there is no consensus as to the best assessment tool for microsurgical skills acquisition [55]. Several methods of evaluation have been proposed, including objective measures such as global rating scales and task checklists [56], and self-appraisal instruments [57]. Deliberating the merits and limitations of different forms of surgical skill assessments is not within the scope of this protocol, however, will be considered in the final review when evaluating the conclusions drawn by individual studies. However, of note, previous microsurgical research concluded that self-evaluated confidence scores reflect objective scores of skill competency such as time to task completion and test scores [57] and therefore will be accepted for inclusion in this review.
Any qualitative data evaluating learner outcomes using XR simulation modalities will also be accepted. Again, self- and externally assessed measures of learner outcomes will be included in the analysis. Use of qualitative data reflects both numerical scoring when evaluating the performance of post-graduate medical trainees and shows greater sensitivity for reflecting vital non-technical skills, such as professional behaviours [58].
The search terms, including wildcard and explosive phrases, are included in Table 2. Search terms were created from the initial PICO inclusion criteria and the initial pilot search of Embase and Medline databases; titles, key words and MeSH headings from identified articles were reviewed and collated to create the proposed search strategy. Initial pilot searches highlighted that the use of ‘microsurgery’ based terms only did not identify notable ophthalmological studies within this field, however, were retrieved by using ophthalmological procedure terms (search lines 9–11).

| 1 | (Augmented reality OR AR OR augmented virtual reality OR augmented reali* OR exp augmented reality).af |
|---|---|
| 2 | (Virtual reality OR VR OR virtual reali* OR exp virtual reality).af |
| 3 | (Mixed reality OR MR OR mixed reali* OR exp mixed reality).af |
| 4 | (Extended reality OR XR OR extended reali* OR exp extended reality).af |
| 5 | Exp education/ OR exp teaching/ OR exp training/ OR exp learning/ OR exp skill/ OR exp simulation/ OR exp curriculum/ OR exp competency |
| 6 | Exp microsurgery/ OR micromanipulation |
| 7 | (Microsurg* OR micromanipulat* OR microvasc* OR microneurosurg* OR microneurovasc* OR supermicrosurg* OR microscope assisted surg*).af |
| 8 | (Free tissue flap* OR free tissue transfer* OR free flap* OR replant* OR revasc* OR anastomos* OR neurovasc*).af |
| 9 | (Vitreo-retin* OR vitreoretin*).af |
| 10 | Exp cataract |
| 11 | Cataract OR Phacoemulsif*.af |
| 12 | 1 OR 2 OR 3 OR 4 |
| 13 | 6 OR 7 OR 8 OR 9 OR 10 OR 11 |
| 14 | 5 AND 12 AND 13 |
Terms-related comparison groups or outcome measures have not been included in the search strategy. References to the study outcomes are not often well detailed within study titles or abstracts, and as they have low retrieval potential, are suggested to not be included within the strategy search terms [59]. Given that educational research within XR is a rapidly growing and developing field, utilizing a more comprehensive strategy allows for maximization of the potential number of relevant identified studies.
The search will be undertaken utilizing Cumulative Index to Nursing and Allied Health Literature (CINAHL), Cochrane Library of Reviews, Embase, Medline (Ovid), and Web of Science databases. Where a major journal related to health professionals’ education or simulation training is not indexed within a database, a specific search of their published literature will be undertaken. Examples of such journals include the International Journal of Healthcare Simulation and MedEdPublish. No limitation on published date or language will be set.
Reviewing and inclusion of relevant grey literature is advantageous in reducing the risk of publication bias within systematic reviews [40]. Grey literature will be searched for in Google Scholar, ProQuest Dissertations, and Theses Global and Open Access Theses and Dissertations. Grey literature, in full-text format such as a report or doctoral thesis, will be included. Where only an abstract is available for grey literature, the corresponding full-text record will be sought from the authors. Abstracts themselves will not be included as conference abstracts are often noted to poorly report research findings, making quality assessment challenging, and so have little effect on the overall conclusions of a review [60].
Both randomized trials and cohort studies will be considered for review, as non-randomized research such as cohort studies, is advised to be evaluated for inclusion when insufficient randomized research exists to thoroughly address the initial investigative question [40]. Literature that does not assess a learning outcome such as editorials or commentaries will be excluded. All literature reviews identified by the search terms and studies selected for inclusion will have reference lists examined to ensure any additional studies are identified.
All search results will be imported into Mendeley (Elsevier, Amsterdam, NED) reference management software for assessment. Duplicate results will be removed prior to review.
Two independent reviewers will screen all results initially based on the title and abstract. Once this has been completed or where compliance with the inclusion criteria is unclear from the abstract, full-text review of the article will be undertaken to evaluate the appropriateness of its selection. Each reviewer will be blinded to the study inclusion decision of the other members of the review team during the screening process. Disagreements will be discussed with the senior author to achieve consensus.
The process of searching, retrieving, reviewing and appraising will be recorded and reported in the systematic review report in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement in the recommended flowchart form [61].
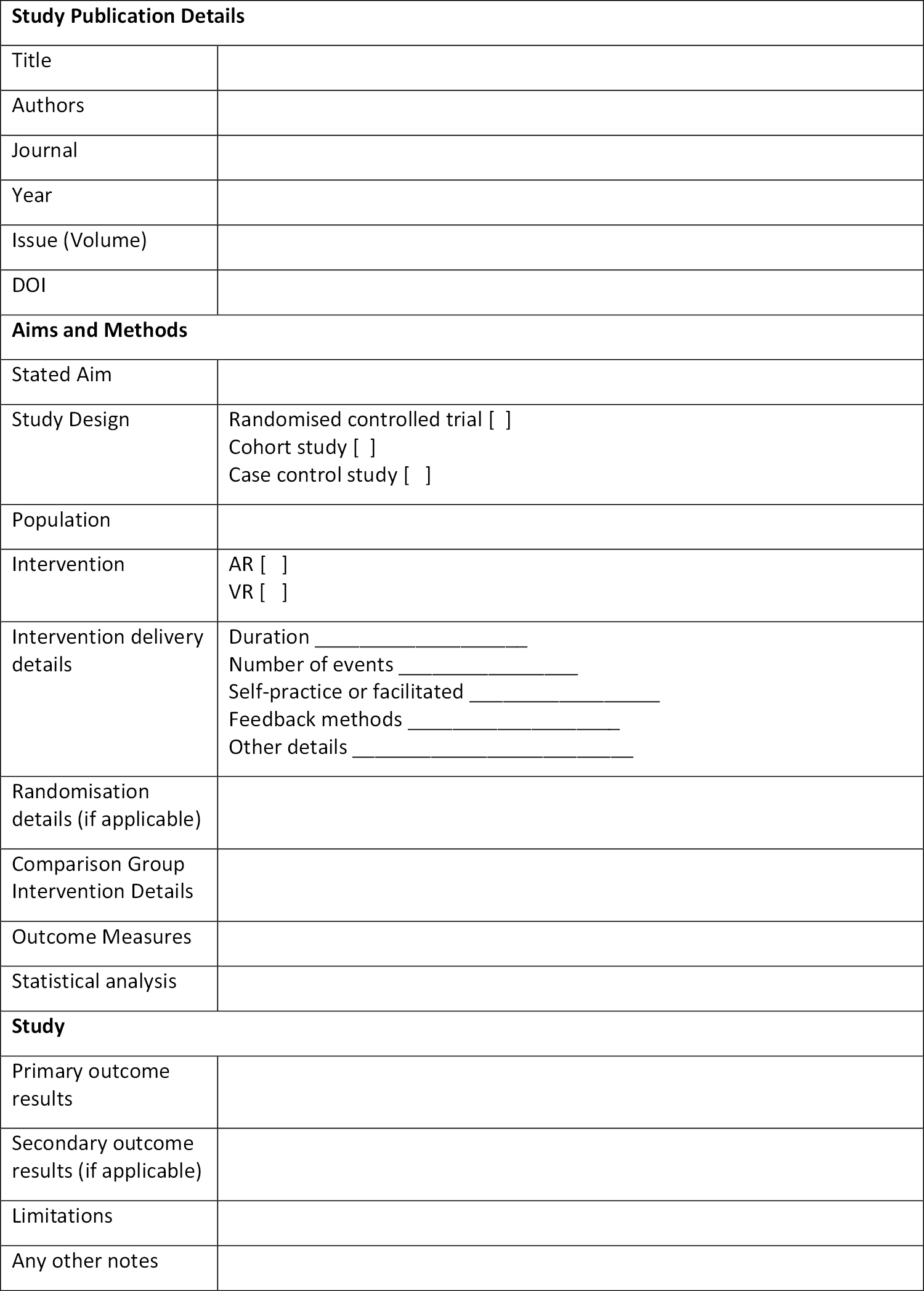
A study detail extraction form was created within Microsoft Excel (Microsoft, Washington, DC) based on the stated inclusion criteria (Appendix 1). Data points include publication information, aims and methods, results, and conclusions. As part of the data extraction process, studies will also be assessed for the relevant modified Kirkpatrick level [62] based on the measured outcome. Although the use of the Kirkpatrick levels is advantageous when appraising rapidly measurable training outcomes, it is more limited in its use when assessing longer-term complex outcomes [63]. Therefore, a low modified Kirkpatrick level will not be utilized as a study exclusion tool.
The data extraction instrument will be piloted by the two independent reviewers, evaluating five randomly selected articles for inclusion. This will act as a form of training exercise for reviewers to ensure familiarity with the extraction tool and allow for any required revisions to be identified prior to the formal data extraction process. This step is in accordance with the Cochrane recommendations for conducting systematic reviews [40].
Data extraction will be undertaken independently by two authors, as this reduces error in comparison to single-author extraction followed by verification by a second author [64]. The results will be verified by reviewing all retrieved data from both authors to ensure consensus. Where disagreements occur, a senior author will review the relevant literature to establish the overall outcome. Missing data or any aspects requiring clarification will be sought from the original study authors.
A second tool appraising the quality of included studies has been generated using the Medical Education Research Study Quality Instrument (MERSQI) (Appendix 2) [65]. The data input process is hosted within Google Forms (Google, Mountain View, CA), to be exported into Microsoft Excel once complete. The MERSQI tool has been proven to be a reliable method of appraising methodological quality within medical educational studies, with high levels of interrater reliability and between-instrument correlation [66]. Neither the MERSQI score nor the previously mentioned Kirkpatrick level will be used as an exclusion tool; instead, their use will allow for additional context and comparisons of the conclusions drawn from individual studies.
Quality of the included studies (as assessed through MERSQI) will be presented in tabular form, with further narrative expansion of notable limitations or strengths that may impact the interpretation of the results.
Two risk-of-bias tools will be utilized. The revised Cochrane risk of bias tool for randomized trials (ROB2) [67] and Risk Of Bias In Non-randomized Studies of Interventions (ROBINS-I) tool [68] for non-randomized studies. In keeping with Cochrane recommendations [31], non-randomized studies deemed at a high risk of bias will be excluded. No exclusion criteria will be set for randomized studies; however, any risk of bias will be considered in the data synthesis stage.
Data analysis will be undertaken in three phases: narrative description of study data, quantitative analysis with meta-analysis if possible; qualitative analysis and overall data synthesis.
It is highly likely, due to the broad inclusion criteria, that differing study designs will be retrieved. Should sufficient numbers of studies be retrieved to allow for subgroup analysis, coherent group themes will be sought to minimize one facet of this heterogeneity, for example, comparing research by extended reality modality or population subtype. Cochrane acknowledges that true pre-specification of sub-groups may not be achievable, and allows for post hoc analyses provided these are clearly identified [40].
Publication details of included studies will be summarized and tabularized. Quantitative data relevant to the investigative question such as measures of central tendency will be presented in tables or figures depending on the nature of the results. As noted previously, it is unlikely that sufficient numbers of homogenous studies will be retrieved to allow for a meta-analysis to be conducted. This possibility is reduced further as it is recommended to undertake separate meta-analyses for randomized and non-randomized study designs [40].
However, should studies have sufficient commonalities in their methodology to allow for pooling and comparison of data, statistical analysis will be run via SPSS Statistics (IBM, New York, NY). Due to the many potential study outcomes measured, the proposal of the specific statistical tests to be undertaken is not possible within the protocol. The absence of committing to a specific statistical proposal allows for the undertaking of a robust review of the literature, as the adaptation of the study protocol in a contemporaneous manner ensures an optimal analysis of the current evidence retrieved. Details of the analysis appropriate for the studies retrieved will be stated in the final systematic review.
Should a meta-analysis be undertaken, a funnel plot for each intervention modality (AR/VR/MR) will be created (comparing study effect estimates against standard error, as recommended by Cochrane [40]) and discussed.
Qualitative data identified will be analysed in a textual narrative format due to its ability to consider evidence across differing study types (including quantitative and qualitative designs) whilst maintaining an ability to evaluate and appraise the quality of included research [69]. A narrative approach is also advantageous when considering the effects of an intervention amongst many heterogenous studies, by discerning what study design characteristics may be responsible for the final result [70].
In addition, as one of the core applications of this form of synthesis is to create output directly applicable to the design, and therefore, evaluation of interventions [71], it holds particular relevance to the aims of this protocol.
After separate analysis of quantitative and qualitative study designs, a convergent integrative synthesis will be undertaken in a parallel-results approach (Figure 2). This allows for a gradual and constant refinement of the interpretation of the study results [72].

![Convergent integrative approach to data synthesis (Adapted from Hong et al. 2017 [73])](/dataresources/articles/content-1747245023308-281a179d-26aa-4e72-bcf4-d875596112ec/assets/ytbx9217_f002.jpg)
Convergent integrative approach to data synthesis (Adapted from Hong et al. 2017 [73])
In addition to the sections previously outlined, the final report will also include a discussion of:
strength of the cumulative evidence presented;
limitations related to the synthesis of included study results;
strengths and limitations associated with the undertaking of the systematic review process itself;
overall implications for microsurgical education, training and practice.
The Cochrane pre-submission checklist [40] will be completed prior to finalization of the study report to ensure a thorough and complete representation of the review’s findings.
Any amendments to the agreed protocol will be discussed amongst the review team to fully evaluate the need for and suitability of the proposed modifications. The PROSPERO record will be amended contemporaneously should any protocol changes be required. Details of any changes to the proposed protocol will be reported in the final systematic review.
The use of XR as a simulation modality for surgical skill acquisition is a rapidly growing field and will continue to do so as increasing advances in innovation improve accessibility to this technology. Microsurgical training presents substantial challenges that may be alleviated using this new method of simulation. The impact of its use when compared to existing surgical education interventions requires careful evaluation, however. This systematic review aims to begin the process of addressing this as well as identifying research gaps requiring further exploration as this discipline develops.
The authors would like to acknowledge Camila Garces-Bovett, Senior Information Specialist, Royal College of Surgeons of England Library and Archives Team, for creating our pilot literature search.
JM proposed the primary research concept and wrote the initial manuscript. RK provided senior support and support in manuscript refinement. All authors developed and refined the methodology and contributed to the editing and approval of the final manuscript.
The authors declare no sources of funding related to the preparation of this manuscript.
Not applicable.
The authors declare no conflict of interest. No author has previously published work related to extended reality in microsurgery. No author is affiliated with a commercial entity related to the field of extended reality education provision or development.
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
55
56
57
58
59
60
61
62
63
64
65
66
67
68
69
70
71
72
73